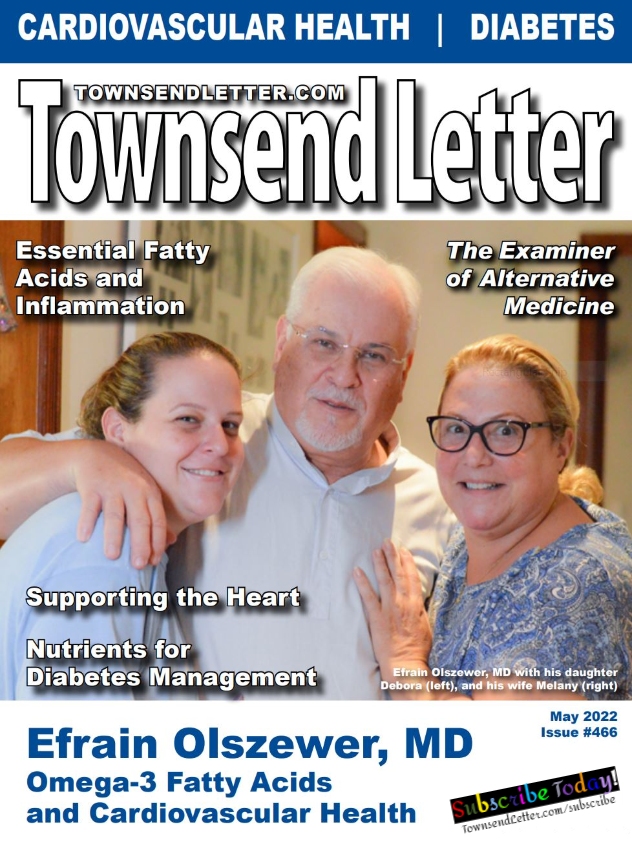
By Efrain Olszewer, MD
Abstract
This systematic review involves studies and meta-analyses that looked at the intake of omega-3 polyunsaturated fatty acids (PUFAs) and their role in cardiovascular prevention and CVD pathologies. We identified and analyzed the benefits of different doses. The studies use varied dosages, which is why, we believe, the studies and meta-analyses have varied, and sometimes controversial, results.
We concluded that there is an inverse relationship between consuming omega-3s and cardiovascular pathologies; the higher the dose of omega-3, the better the results seem to be.
The authors recommend more studies with adequate doses of omega-3 to establish an ideal dosage with a strong inverse relationship between omega-3 consumption and cardiovascular disease.
Understanding Omega-3s
Omega-3 polyunsaturated fats consist of carbon atoms and double bonds; the first double bond is three carbon atoms from the omega end. The omega-3 alpha-linolenic acid (ALA) has 18 carbon atoms with three double bonds. When the enzyme elongase is activated, linolenic acid incorporates two more carbon atoms for a total of 20 and is converted to EPA (eicosapentaenoic acid); and the addition of two more carbon atoms turns EPA into another omega-3, DHA (docasahexaenoic acid). EPA is also metabolized into prostaglandin E3 (PGE3), which has the following effects: anti-inflammatory, vasodilatation, platelet anti- aggregation, and anti-thrombotic.1-2
EPA and, to a lesser extent, DHA have been shown to affect endothelial function, dyslipidemia, hypertension, atherosclerosis, and arteriosclerosis.4
The nutritional pharmacological activity of linolenic acid and its derivatives EPA and DHA is based on the presence of three important molecules: protectins, resolvins, and lipoxins. These three molecules modulate the anti-inflammatory pathway of PGE3, which has a modulation-inhibitory effect over the pro-inflammatory activity of PGE2, and modulate the lipoxygenase pathway and pro-inflammatory alternative mechanism related to the buildup of the leukotrienes family.3
The pro-inflammatory pathway includes the formation of arachidonic acid (AA) by cytokines activated from white blood cells and visceral fats, converting linoleic acid (AA precursor) by use of the phospholipase A enzyme, stimulating the cyclooxygenase enzyme, and building up the last molecule PGE2,4 that has the following properties: vasoconstrictor, pro-inflammatory, platelet aggregation, and pro-thrombotic.5
Asmaa Abdelhamid, published in 2018, a negative meta-analysis between omega-3 and cardiovascular diseases in the Cochrane Database Systemic Review. From this study, we decided to randomly choose five studies from the 70 cited to see if we found the same relationship; none of the five cited this relationship. Instead, we found the following:
- Culp, 1980: it found beneficial effects of omega-3 in cardiovascular diseases.
- Proudman, 2015: all the studies involved rheumatoid arthritis.
- Erdogan, 2007: the study was only related to atrial fibrillation.
- Welcome, 2015: only looked at non-fatty liver disease.
- Sofa, 2006: the study was on tachyarrhythmia and implantable defibrillator.
The DOT study included different studies one showing benefit in endothelial markers and controlling interleukin. Identifying this controversial use of medical studies, we decide to study only those research papers that have a direct relationship between omega-3 and cardiovascular disease.
In 2020 Abdelhamid et al added updated evidence suggesting that increasing LCn3 [long chain omega 3] slightly reduces coronary heart disease events and mortality (previously the evidence suggested little or no effect). Our understanding of effects of LCn3 on other outcomes, and of ALA on all outcomes, has not been altered.6
Based on the physiological and nutria-pharmacological action of omega-3, we reviewed studies in order to see the relationship between the ingestion as nutrients and the cardiovascular risks.
Omega-3 and Cardiovascular Disease
An study published in 2020 showed that the omega-3 (n-3) fatty acids, EPA and DHA, in long-term prospective cohort studies, consistently demonstrate an association between higher intakes of fish, fatty fish, and marine n-3 fatty acids (EPA + DHA) or higher levels of EPA and DHA in the body and lower risk of developing cardiovascular disease (CVD), especially coronary heart disease (CHD) and myocardial infarction (MI), and lower cardiovascular mortality in the general population. This cardioprotective effect of EPA and DHA is most likely due to the beneficial modulation of a number of known risk factors for CVD, such as blood lipids, blood pressure, heart rate and heart rate variability, platelet aggregation, endothelial function, and inflammation.7
Zhang et al made a long study involving a total of 240,729 men and 180,580 women from NIH-AARP Diet and Health Study who were prospectively followed-up for 16 years. Dietary intakes were assessed using a validated NIH Diet History Questionnaire. A total of 54,230 men and 30,882 women died during 6.07 million person-years of follow-up. Higher fish and LCn-3 PUFAs intakes were significantly associated with lower total mortality (P < 0.0001). Comparing the highest with lowest quintiles of fish intake, men had 9% (95% confidence interval, 6-11%) lower total mortality, 10% (6-15%) lower cardiovascular disease (CVD) mortality, 6% (1-10%) lower cancer mortality, 20% (11-28%) lower respiratory disease mortality, and 37% (17-53%) lower chronic liver disease mortality; women had 8% (5-12%) lower total mortality, 10% (3-17%) lower CVD mortality, and 38% (20-52%) lower Alzheimer’s disease mortality.8
For men whose intake of omega-3 fatty acids placed them among the highest 20%, the risk of mortality from any cause was 11% lower than the risk experienced by men whose intake was among the lowest 20%. Similarly, women who were among the top 20% of omega-3 consumers had a 10% lower risk.
When the risk of death from specific diseases was analyzed, men who had the highest intake of omega-3s experienced a 15% lower risk of dying from cardiovascular disease, and for women in the top group, the risk was 18% lower. Another interesting finding was that the greater omega-3 fatty acid intake was significantly associated with a lower risk of mortality due to respiratory disease and Alzheimer’s disease in men and women, and with a lower risk of chronic liver disease and cancer in men.8
The Netherlands Heart Foundation showed that low-dose supplementation with EPA–DHA or ALA did not significantly reduce the rate of major cardiovascular events among patients who had a myocardial infarction and who were receiving state-of-the-art antihypertensive, antithrombotic, and lipid-modifying therapy, showing clearly that low doses of omega-3 have no influence on cardiovascular disease.9
Another study done at Harvard University researched the benefits of vitamin D and omega-3 in cardiovascular disease; it included 25,871 people, with mean age of 50 years, using 1 gram of omega-3 daily. Though the authors’ conclusions established there was no effect on cardioprotective pathologies by either vitamin D or omega 3, the second end point was extremely relevant.
Upon closer examination, the results showed a reduction in heart attacks without a reduction in strokes. Specifically, the omega-3 fatty acid intervention lowered the risk of heart attack by 28% and the risk of fatal heart attack by 50% but had no benefit on stroke or cardiovascular deaths not related to heart disease. Additionally, omega-3 fatty acids reduced the rate of angioplasty procedures by 22%. In the same study African Americans had a remarkable 77% reduction in heart attacks compared to the placebo.10
The most compelling evidence for CV benefits of omega -3 PUFA comes from four controlled trials of nearly 40,000 participants randomized to receive eicosapentaenoic acid (EPA) with or without docosahexaenoic acid (DHA) in studies of patients in primary prevention, after myocardial infarction, and most recently, with heart failure (HF).
The evidence from retrospective epidemiologic studies and from large randomized controlled trials show the benefits of omega-3 PUFA, specifically EPA and DHA, in primary and secondary CV prevention and provide insight into potential mechanisms of these observed benefits. An important aspect was that the target EPA-DHA consumption should be at least 500 mg/day for individuals without underlying overt CV disease and at least 800 to 1,000 mg/day for individuals with known coronary heart disease and HF.11
Randomized controlled trials (RCTs) assessing use of long-chain omega-3 polyunsaturated fatty acids (LC-OM3), primarily eicosapentaenoic acid and/or docosahexaenoic acid, have shown mixed results. A study included fourteen RCTs (randomized controlled studies) for the primary analysis (71,899 subjects). In the long chain omega-3 (LC-OM3) arms, 1613 cardiac deaths were recorded (4.48% of subjects), compared with 1746 cardiac deaths in the control groups (4.87% of subjects). The pooled relative risk estimate showed an 8.0% (95% confidence interval 1.6%, 13.9%, P = .015) lower risk in the LC-OM3 arms vs controls. Subset analyses showed numerically larger effects (12.9%-29.1% lower risks, all P <.05) in subsets of RCTs with eicosapentaenoic acid plus docosahexaenoic acid with dosages >1 g/day. Also, larger effects were seen with patient groups with higher risks, including baseline mean or median triglycerides ≥150 mg/dL; low-density lipoprotein cholesterol ≥130 mg/dL; and statin use <40% of subjects.12
Statistically significant protective effects were observed for cardiac death (RR, 0.68; 95% CI, 0.56 to 0.83), sudden death (RR, 0.67; 95% CI, 0.52 to 0.87), and myocardial infarction (RR, 0.75; 95% CI, 0.63 to 0.88) in a meta-analysis done by Yun-Tao Zhao et al.
Eight trials were identified, comprising 20,997 patients. In patients with prior myocardial infarction (MI), omega-3 fatty acids reduced relative risk (RR) of SCD (RR = 0.43; 95% CI: 0.20-0.91). In patients with angina, omega-3 fatty acids increased RR of SCD (RR = 1.39; 95% CI: 1.01-1.92). Relative risk for cardiac death and all-cause mortality were 0.71 (95% CI: 0.50-1.00) and 0.77 (95% CI: 0.58-1.01), respectively. Overall, their results supply evidence that long-term effect of high-dose omega-3 fatty acid supplementation may be beneficial for decreasing the risk of cardiac death, sudden death, and myocardial infarction among patients with a history of cardiovascular disease.13
Dietary supplementation with omega-3 fatty acids reduces the incidence of sudden cardiac death in patients with MI but may have adverse effects in angina patients, and this should be studied.13
Omega-3 and Vascular Diseases, Inflammation, and Atherosclerosis
“Vascular inflammation is a key component involved in the process of arthrosclerosis, which in turn increases the risk for cardiovascular injury. In the last 10 years, there have been many trials that looked at omega-3 fatty acids to reduce cardiovascular risk.”14 Omega-3s have decreased triglyceride levels in several studies and increased increased LDL and HDL levels, “likely because omega-3 fatty acids promote triglyceride conversion into HDL/LDL.”14
In their review article, Sarabjeet Singh et al looked at the effects of omega-3 fatty acids DHA and EPA on triglycerides, LDL-cholesterol and HDL-cholesterol in seven clinical studies. In a second data search, Singh et al looked at vascular biomarkers and cardiovascular risk in articles that focused on high-sensitivity C-reactive protein and oxidized low-density lipoprotein.14 Two of the more recent trials, MARINE and ANCHOR, looked at omega-3 effects on vascular inflammatory markers as well as triglycerides, LDL, and HDL.
“The results of two of these trials not only showed reduction in cardiovascular risk because of reduction in vascular inflammation and reduction in the lipid panel but also showed that one of the MARINE-derived omega-3 fatty acids is superior to the other.”14
Although both EPA and DHA decreased triglyceride level and increased HDL-C in earlier studies, those studies also showed that DHA “has more undesirable effects on LDL.” EPA does not have the same effect on LDL. “Furthermore, the MARINE and ANCHOR trials have both shown that not only does EPA improve the lipid panel but also helps to decrease the levels of the vascular inflammatory biomarkers, thus further helping to decrease cardiovascular risk.”14
Biochemical studies have shown the PUFAS pathway’s role in inflammation resolution. Omega-3 fatty acids serve as the substrate for the formation of a group of lipid mediators that mediate the resolution of inflammation. The cardiovascular inflammatory response in atherosclerosis and vascular injury is characterized by a failure in the resolution of inflammation, resulting in a chronic inflammatory response.15
Importantly, the resolution of cardiovascular inflammation is an active, multifactorial process that involves modulation of the immune response, direct actions on the vascular wall, as well as close interactions between macrophages and vascular smooth muscle cells. Promoting anti-atherogenic signaling through the stimulation of endogenous resolution of inflammation pathways may provide a novel therapeutic strategy in cardiovascular prevention.15
EPA and DHA have proven effective at inhibiting calcification in vivo.16,17 Specifically, EPA inhibit warfarin-induced vascular calcification in rats and spontaneous vascular calcification in klotho mutant mice.18
Mechanically, some work trying to elucidate the mechanism of action of DHA and EPA has been carried out using calcifying vascular cells (CVCs), a subpopulation of bovine aortic medial cells that undergo spontaneous osteoblast differentiation and calcification.15
DHA promotes the phosphorylation of p38 mitogen-activated protein kinase (MAPK), alongside the activation of the peroxisome proliferator-activated receptor-γ (PPAR-γ). In line with these results, EPA prevents the β-catenin-induced VSMC trans-differentiation towards osteoblast-like cells through the activation of PPAR- γ.15
In another study the author established that there is a vast disagreement in relation to the possible beneficial effects of omega-3 polyunsaturated fatty acids (omega-3 PUFA) supplementation in patients with diabetes and cardiovascular disease.19 The conflicting results between the various original studies and meta-analyses could be partially explained as a result of variable supplementation dosage and duration, either of which may modify the effects of omega-3 PUFA on cardio-metabolic biomarkers. Meta-analyses are limited usually by the inability to draw inferences regarding dosage, duration and the interaction of dosage and duration of omega-3 PUFA intake. Even so, almost all endpoints in the so-called “negative” meta-analyses leaned toward a trend for benefit with a near 10% reduction in cardiovascular outcomes and a borderline statistical significance. Many trials included in these meta-analyses tested an insufficient daily dose of omega-3 PUFA of less than 1000 mg. Other studies clearly indicate that, probably, the consistent cardiovascular effects of omega-3 PUFA supplements could be expected only with daily doses above 2000 mg.20,21
In the Diet and Reinfarction Trial, 2033 men who had recovered from MI were advised to increase fatty fish intake, to increase dietary fiber, to decrease saturated fat. This study done by MRC Epidemiology Unit, Cardiff, where subjects were given a fatty fish diet/week (~350 mg of EPA/d) had a 29% reduction in all‐cause mortality over two years.22
In a follow-up study, the researchers looked at blood pressure in the men who were told to eat two portions of fatty fish/week or take EPA (330 mg/d) and compared that group to the men who did not receive that advice. They found that the fish group (when adjusted for age and BP at baseline) showed at difference of -0.61mm Hg at 6 months and 0.40 mm Hg at two years. The difference in diastolic BP was -0.50 mm Hg at 6 months and 0.19 mm Hg at two years.23
In a GISSI-Prevenzione trial, conducted between 1993‐1995, 2836 men and women who had survived a recent MI (≤3 months) MI received EPA/DHA (1 g/day) for 3.5 years. Results showed 30% reduction of CV death, 20% reduction in major fatal events and 45% reduction from sudden cardiovascular death (SCD). However, no significant beneficial effect was obtained in patients with stroke or non‐fatal MI. The beneficial protective effect from SCD was four times higher in patients with left ventricular systolic dysfunction.24,25
In the JELIS trial, between 1996‐1999, 18,645 hypercholesterolemic (≥6.5 mmol/L) patients on statin therapy, with or without CHD, in Japan were given 1800 mg EPA/day. At the 5-year follow up, the EPA group had 19% reduction in major CV events and 25% reduction in LDL cholesterol.26
The GISSI‐HF randomized, placebo-controlled trial, between 2002‐2008, enrolled 6975 CHF patients (New York Heart Association class II‐IV) irrespective of cause and left ventricular ejection fraction >40%. The treatment group received 1 g daily EPA/DHA. At median 3.9 years follow up, there was a 6% reduction in CV death or hospitalization.27
A decreased mortality rate from CHD was evidenced in a Japanese population when they consumed three or more servings of not fried seafood. Furthermore, when compared to the subjects with little or no seafood intake, the protection is better for moderate consumers of one to two servings/week.28-30
A strong review done in 2019 briefly describes why some studies may have shown no benefits and reviewed three very recent major clinical trials that did show CVD benefits for omega-3 fatty acids. These studies included healthy individuals, patients with diabetes, and patients with mildly elevated triglycerides taking statin drugs.31
They also describe possible mechanisms that explain the cardiovascular benefits of omega-3 fatty acids, define current long-chain omega-3 fatty acid intakes, and advise clinicians about what can be done in practice to first determine and then optimize the omega-3 fatty acid intake for their patients.

• Clinical trial results released in the past 12 months have demonstrated clear benefits of omega-3 fatty acid intake for cardiovascular disease risk, with significant reductions in risk of heart attacks, other major cardiovascular events, and cardiovascular disease death.
• The mixed results regarding the effects of omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) on the primary and secondary prevention of cardiovascular disease from previous studies may be due in part to methodological limitations, such as using composite end points, a short intervention duration, low omega-3 fatty acid supplementation dose, and high background fish intake.
• Based on results from REDUCE-IT, the addition of 4 g/d of EPA should be considered for statin-treated patients who have cardiovascular disease or diabetes and elevated triglycerides.
• For clinical practice, evidence from the most recent clinical trials supports the recommendation to consume at least one to two servings of fish/seafood per week, with additional primary prevention benefits conferred by consuming ~1 g/d of EPA and DHA.31
Kathy Musa-Veloso et al reached in their study the following conclusions: “Prospective observational and intervention data from Japan, where intake of fish is very high, suggest that n-3 LCFA intakes of 900 to 1000 mg/d and greater may confer protection against non-fatal myocardial infarction. Thus, the intake of 250 mg n-3 LCFA per d may, indeed, be a minimum target to be achieved by the general population for the promotion of cardiovascular health.”32
A meta-analysis of 13 randomized controlled trials, one of which was REDUCE-IT (Reduction of Cardiovascular Events with Icosapent Ethyl-Intervention Trial), looked at myocardial infarction, coronary heart disease (CHD) death, total CHD, total stroke, CVD death, total CVD, and major vascular events. This current updated meta-analysis incorporating data from 13 RCTs, including three recent large trials, suggests that marine omega-3 supplementation is associated with lower risk of MI, total CHD, total CVD, and death from CHD or CVD causes. Such inverse associations may be particularly evident at higher doses of marine omega-3 supplementation:
Inverse associations for all outcomes were strengthened after including REDUCE-IT while introducing statistically significant heterogeneity. Statistically significant linear dose-response relationships were found for total CVD and major vascular events in the analyses with and without including REDUCE-IT…. Marine omega-3 supplementation lowers risk for myocardial infarction, CHD death, total CHD, CVD death, and total CVD, even after exclusion of REDUCE-IT. Risk reductions appeared to be linearly related to marine omega-3 dose.33
Atheroma’s Instability
Tetsuya Aman et al found: “A lower serum content of ω3 PUFAs (especially of EPA and DPA) was significantly associated with lipid-rich plaques, suggesting the contribution to the incidence of acute coronary syndrome.”34
Patients with low EPA levels, low DPA levels, and low DHA levels had a significantly higher % lipid volume (p = 0.048, p = 0.008, and p = 0.036, respectively) and a significantly lower % fibrous volume (p = 0.035, p = 0.008, and p = 0.034, respectively) than those with high levels of these fatty acids. Even after adjustment for confounders, the presence of both low EPA and low DPA levels proved to be an independent predictor for lipid-rich plaques in any of the two categories.34
Results from cross-sectional studies,35 cohort studies,36 and RCTs37, 38 on the associations of consumption of fish or fish oil with the progression of atherosclerosis are mixed. Our observed HRs, which were close to 1.00 for the association between n-3 LCPUFAs and the progression of atherosclerosis, including both native disease and restenosis, support previous studies observing no or modest effects.35,37 In contrast, Erkkila et al observed reduced progression of atherosclerosis among diabetic women with existing CAD consuming two servings of fish per week compared with women with lower intakes.36 However, the EPA+DHA intakes in the reference group in that study were much lower than in our study, and this may be an explanation in populations with lower intakes than ours.
In a population with established and well-treated CAD and with a relatively high intake of n23 LCPUFAs, we observed no significant association between intakes of n-3 LCPUFAs or fish and risks of coronary events or mortality. Only patients with very low intakes of these fatty acids may reduce their risk of coronary events by increasing their intakes.38
Epidemiological and clinical evidence suggests that an increased intake of long-chain n-3 fatty acids protects against mortality from coronary artery disease.
A five-year Japanese study recruited 18,645 patients with high cholesterol (6.5 mmol/L or more) between 1996 and 1999. They were randomized into two groups: 1800 mg of EPA/day with statin (n=9326) or statin only (control, n=9319). Any major coronary event was the primary endpoint: sudden cardiac death, fatal and non-fatal myocardial infarction, and other non-fatal events including unstable angina pectoris, angioplasty, stenting, or coronary artery bypass grafting.
In patients with a history of coronary artery disease who were given EPA treatment, major coronary events were reduced by 19% (secondary prevention subgroup: 158 [8·7%] in the EPA group vs 197 [10·7%] in the control group; p=0·048). In patients with no history of coronary artery disease, EPA treatment reduced major coronary events by 18%, but this finding was not significant (104 [1·4%] in the EPA group vs 127 [1·7%] in the control group; p=0·132).
EPA is a promising treatment for prevention of major coronary events, and especially non-fatal coronary events, in Japanese hypercholesterolemia patients.39
The results of the Omacor Carotid Endarterectomy Intervention (OCEAN) study showed that advanced atherosclerotic plaques incorporated omega-3 fatty acids when available; “and this results in lower numbers of macrophages, foam cells, and T cells, as well as the lower expression of inflammatory markers.”40 Histologically, the plaque appears to be less inflamed and more stable. This may contribute to reduced mortality in patients consuming omega-3 fatty acids, for example, in the GISSI-Prevenzione trial.
In his 2012 article, Phillip C. Calder explained:
Eicosanoids produced from arachidonic acid have roles in inflammation. EPA also gives rise to eicosanoids and the products are usually biological weak. EPA and DHA give rise to resolvins, which are anti-inflammatory and inflammation resolving. EPA and DHA also affect production of peptide mediators of inflammation (adhesion molecules, cytokines, etc.). Thus, the fatty acid composition of human inflammatory cells influences their function; the contents of arachidonic acid, EPA and DHA aperture especially important. The anti-inflammatory effects of marine n-3polyunsaturated fatty acids (PUFAs) may contribute to their protective actions towards atherosclerosis and plaque rupture.41
A clinical trial published in The Lancet (February 8, 2003) found that omega-3 fatty acids enhanced the stability of atherosclerotic plaques. The researchers randomized 162 patients awaiting carotid endarterectomy into three groups. They received six capsules of either fish oil (1.4 grams omega-3 fatty acids), sunflower oil (3.6 grams of the omega-6 fatty acid linoleic acid), or an oil blend designed to provide the intake of the average adult diet (control) before surgery. Median treatment time was 42 days. They found:
Atherosclerotic plaques readily incorporate n-3 PUFAs from fish-oil supplementation, inducing changes that can enhance stability of atherosclerotic plaques. By contrast, increased consumption of n-6 PUFAs does not affect carotid plaque fatty-acid composition or stability over the time course studied here. Stability of plaques could explain reductions in non-fatal and fatal cardiovascular events associated with increased n-3 PUFA intake.42
Omega-3 and Hypertension
Lawrence J. Appel and colleagues conducted a meta-analysis of controlled clinical trials that looked at the effect of omega-3 on blood pressure.
In the 11 trials that enrolled normotensive individuals (n=728), ω-3 PUFA supplementation led to significant reductions of systolic BP (SBP) and diastolic BP (DBP) in two and one trials, respectively. In the six studies that enrolled untreated hypertensives (n=291), significant reductions of SBP and DBP were present in two and four trials, respectively….
Doses of ω-3 PUFA tended to be high (average dose >3 g/d in 11 trials). The magnitude of BP reduction was greatest at high BP but was not significantly associated with dose of ω-3 PUFA….
Our analyses indicate that diet supplementation with a relatively high dose of ω-3 PUFA, generally more than 3 g/d, can lead to clinically relevant BP reductions in individuals with untreated hypertension.43
In their investigation of EPA, DHA, and blood pressure, Paige E. Miller and colleagues used random-effects meta-analyses to generate weighted group mean differences and 95% confidence intervals (CIs) between the EPA+DHA group and the placebo group: “Modification of the blood pressure effects by age, gender, blood pressure, and body mass index was examined.”44
Their meta-analyses of seventy RCTs showed that EPA+DHA provision reduced systolic blood pressure (−1.52 mm Hg; 95% confidence interval (CI) = −2.25 to −0.79) and diastolic blood pressure (−0.99mm Hg; 95% CI = −1.54 to −0.44) compared to control. “Overall, available evidence from RCTs indicates that provision of EPA+DHA reduces systolic blood pressure, while provision of ≥2 grams reduces diastolic blood pressure.”44
Johanna M. Geleijnse et al conducted a meta regression analysis of 90 randomized trials (1966-March 2001) involving fish oil and blood pressure. “Intake of fish oil was high in most trials (median dose: 3.7 g/day). Fish oil reduced systolic BP by 2.1 mmHg [95% confidence interval (CI): 1.0, 3.2; P<0.01] and diastolic BP by 1.6 mmHg (95% CI: 1.0. 2.2; P<0.01).”45
They concluded: “High intake of fish oil may lower BP, especially in older and hypertensive subjects. The antihypertensive effect of lower doses of fish oil (< 0.5 g/day) however, remains to be established.”45
Toshinori Hoshi et al describe a mechanism that helps explain the health-promoting effects of long-chain polyunsaturated omega-3 fatty acids. They report:
…DHA with an EC50 of ∼500 nM rapidly and reversibly activates BK channels composed of the pore-forming Slo1 subunit and the auxiliary subunit β1, increasing currents by up to ∼20-fold. The DHA action is observed in cell-free patches and does not require voltage-sensor activation or Ca2+ binding but involves destabilization of the closed conformation of the ion conduction gate. DHA lowers blood pressure in anesthetized wild type but not in Slo1 knockout mice. DHA ethyl ester, contained in dietary supplements, fails to activate BK channels and antagonizes the stimulatory effect of DHA. Slo1 BK channels are thus receptors for long-chain omega-3 fatty acids, and these fatty acids—unlike their ethyl ester derivatives—activate the channels and lower blood pressure. This finding has practical implications for the use of omega-3 fatty acids as nutraceuticals for the general public and also for the critically ill receiving omega-3–enriched formulas.46
Omega-3 Endothelial Rigidity
Matthew P. Pace and colleagues conducted a meta-analysis with 10 trials to assess the effect of omega-3 supplementation on arterial stiffness. Four trials used pulse wave velocity (PWV), and six used arterial compliance, measured as capacitive compliance or systemic arterial compliance, as outcome measures.
Meta-analysis revealed that n-3 was statistically significant in effectively improving both PWV (g = 0.33; 95% CI 0.12, 0.56; P<0.01) and arterial compliance (g = 0.48; 95% CI 0.24, 0.72; P<0.001). The findings of the present study reveal that supplementation with n-3 offers a scientifically supported means of reducing arterial stiffness. Reduction in arterial stiffness by n-3 may account for some of its purported cardioprotective effects.47
Gerasimos Siasos et al conducted a double blind, placebo-controlled cross-over study with 20 healthy smokers to see if supplementation with omega-3 polyunsaturated fatty acids had an effect on endothelial function or arterial stiffness. In the 12-week study, 2 grams/day of omega-3s resulted in significant improvement in pSm values of flow-mediated dilation (FMD; endothelial function; p<0.05), augmentation index (AIx; arterial wave reflections; p<0.001) and pulse wave velocity (PWV; aortic stiffness; p<0.01). Even though smoking caused a decrease in FMD and increases in Aix and PWV, omega-3 treatment “blunted the acute smoking-induced impairment of FMD (p<0.001), AIx (p<0.05) and PWV (p<0.05) and significantly decreased levels of TNFα (p<0.05) and IL-6 (p=0.01) and increased levels of PAI-1 (p=0.05).”48 In conclusion, healthy smokers who took omega-3 polyunsaturated fatty acids showed improved endothelial function, more elasticity in the arteries, and less inflammation.48
Marcela A. Casanova et al conducted a study to compare omega-3 and ciprofibrate effects on vascular structure and function in hypertensive patients with hypertriglyceridemia: “Association between hypertriglyceridemia and cardiovascular (CV) disease is still controversial.”49 The 29 adults with high triglycerides (150-499 mg/dL) were randomly assigned to receive omega-3 fatty acids (1800 mg/day) or ciprofibrate (100 mg/day) for 12 weeks. After an eight-week washout period, the treatment was switched.
Clinical evaluation and vascular tests were assessed at baseline and after intervention. Peripheral (131±3 to 125±3 mmHg, P<0.05) and aortic (124±3 to 118±2 mg/dL, P<0.05) systolic blood pressures were decreased by ciprofibrate in low-risk patients (CV risk<7.5%). In high-risk patients (CV risk≥7.5%), pulse wave velocity was reduced (10.4±0.4 to 9.4±0.3 m/s, P< 0.05) and flow-mediated dilation was increased (11.1±1.6 to 13.5±1.2%, P<0.05) by omega-3. In conclusion, omega-3 improved arterial stiffness and endothelial function, pointing out the beneficial effect of this therapy on vascular aging, in high-risk patients.49
Conclusion
Marine omega-3 fatty acids are effective in preventing cardiovascular and coronary events and cardiac deaths, especially in persons with high cardiovascular risk. In this systematic review, we found an overall decreased risk of cardiovascular event, a decreased risk of cardiac death, and a decrease of coronary events.
It seems also that there is an inverse relationship between the doses of omega-3 and the cardiovascular risk.
This study strongly suggests that supplementation with omega 3 is an important prevention measure in cardiovascular risk. “Most of the studies analyzed included persons with high cardiovascular risk.”50
Efrain Olszewer, MD, who specializes in internal medicine and cardiology, is clinical director of the International Center of Prevention Medicine (CMP) in Brazil. He is the president of the Brazilian Orthomolecular Society and editorial director of the Journal of Orthomolecular Practice. He has written 93 books on health and medicine.