…article continued:
Root Canal Teeth
Root canal failure can be caused by many factors such as:
- Persistence of bacteria (intra-canal and extra-canal),
- Inadequate filling of the canal (canals that are poorly cleaned and obturated),
- Overextensions of root filling materials,
- Improper coronal seal (leakage),
- Untreated canals (both major and accessory),
- Iatrogenic procedural errors such as poor access cavity design, and
- Complications of instrumentation (ledges, perforations, or separated instruments).
However, the most common cause of root canal failure is persistent bacterial infection.22
Montalvo et el. investigated how Treponema denticola influenced disease progression in endodontically treated teeth. Treponema denticola is commonly found in root canals and may cause tissue damage. Due to its pervasiveness, it may be responsible for periapical bone lesions. The genus Treponema has been linked to numerous chronic diseases, such as syphilis (Treponema pallidum), periodontal diseases (including chronic periodontitis and acute necrotizing ulcerative gingivitis), endodontic infections, and some acute dental abscesses.23
The pathogens of acute apical abscesses and asymptomatic root canal teeth were studied to evaluate the occurrence of the most common taxa using a two-step 16S rRNA gene-based PCR protocol. All samples found bacterial DNA. In abscesses, the most prevalent taxa were Fusobacterium nucleatum ssp. (60%), Porphyromonas endodontalis (53%), Parvimonas micra (51%), and Streptococcus species (45%).
The most frequently detected taxa in asymptomatic teeth were P. endodontalis (63%), Dialister invisus (58%), Olsenella uli (56%), and F. nucleatum ssp (51%).24
A systematic review by Muacevic et al. also found that the principal reason for endodontic failure is due to bacteria, with the most common culprit being Enterococcus faecalis, noting that it more likely found in asymptomatic cases than symptomatic cases. Enterococcus faecalis was also found to be highly resistant to disinfectant treatments.25 Microorganisms found in root canal treated teeth such as P. gingivalis, T. denticola, T. forsythia, and Solobacterium moorei have been connected with osteomyelitis, bacterial endocarditis, brain abscess, obesity, and preterm low birthweight. Root canal infections can develop into systemic infections.26
Lačević et al explored the relationship between Tannerella forsythia, Porphyromonas gingivalis, Fusobacterium nucleatum, and Aggregatibacter actinomycetemcomitans at dual sites in concurrent endodontic- periodontal diseases. They found in the sixty samples from both the endodontium and periodontium the following:
- F. nucleatum ssp (100% of both endodontic and periodontal samples)
- T. forsythia (93% of periodontal pocket samples; 90% in primary endodontic infection)
- P. gingivalis (53% of periodontal pocket samples; 70% in primary endodontic infection)
- A. actinomycetemcomitans (13% of periodontal pocket samples; 3% in primary endodontic infection)
They concluded that the endodontic bacteria most likely originated from periodontal pockets and that endodontic infections maintained periodontal pockets and periodontal infection.27
DNA ConneXions Oral Panel
The DNA ConneXions Oral Panel is a DNA PCR-based panel designed to detect the presence or absence of 88 microbes in oral samples. Sampling methods vary, inclusive of teeth, oral blood, bone, dental implants, Super Floss, etc. The question was raised if it is necessary to grind or otherwise fractionate whole tooth samples before employing our DNA extraction techniques. We hypothesized that a more robust and comprehensive microbial DNA extraction could be obtained by fractionating or grinding whole tooth samples. The objective of this study was to elucidate whether or not the porosity of teeth alone allows for the comprehensive release of the microorganisms of such solid samples.
Materials and Methods
The DNA extraction protocol employed at DNA ConneXions requires a 200 ul starting volume of sample. Blood, cavitations, and otherwise liquid samples submitted in volumes in excess of 200 ul are thoroughly homogenized and 200 ul is aliquoted and purified to obtain a prepared DNA sample. The volume of liquid samples received that are less than 200 ul are supplemented with Molecular Grade Water and are thoroughly homogenized; and 200 ul is aliquoted and utilized. Considering other sampling types (Super Floss, Paper Points, etc.), predetermined volumes of Molecular Grade Water are added, is thoroughly homogenized and 200 ul is obtained for testing/purification. Teeth, implants, either dry or accompanied by tissue, bone, blood, etc. are sampled in the same manner. The amount of Molecular Grade Water added to each sample is designed to supplement low volume/dry samples without compromising sample integrity.
Theoretically the addition of volume, followed by excessive agitation via vortex is thought to ‘dislodge’ the microbes present from the sample type provided, facilitating their transfer into the Molecular Grade Water, which is then drawn off and subjected to the DNA extraction protocol.
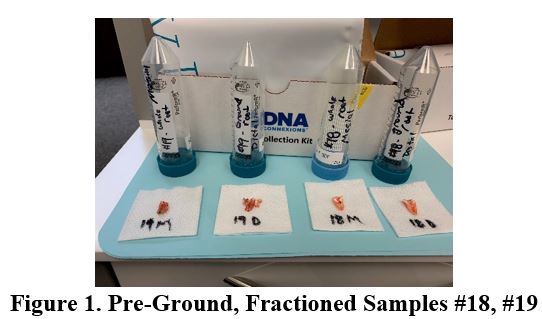
For DNA ConneXions, two juxtaposed samples were extracted from the same patient at the same time: #18 Non-vital tooth, #19 Root canal tooth. Each tooth was fractioned into two samples (Figure 1). One half of each sample was placed in sterile, single use plasticware that had been flushed with nitrogen gas to preserve genetic material during return shipping (provided by DNA ConneXions). The remaining half of each sample was ground into a fine powder using the KometaBio Dentin grinder (Fig. 2). Each grinding blade is a single use, sterile blade/collection cup, ensuring no cross contamination between samples occurs. The ground sample was also placed into a single use plasticware that has been flushed with nitrogen gas. All samples were returned to DNA ConneXions for analysis, where two extractions for each sample was performed with the intent of comparing current and hypothesized methodologies.
Each sample was subjected to the standard DNA ConneXions customary protocol for Oral Panel samples. Quantification via NanoDrop spectrophotometry was performed to ensure both nucleic acid purity and concentration. Samples were inoculated into prepared PCR plates encompassing the 88 microorganisms, included on the DNA ConneXions Oral Panel.
DNA extraction is performed utilizing a non-organic, spin column extraction protocol. DNA is precipitated with ethanol, and a series of ethanol-based washes are utilized, and purified DNA is collected and suspended in an elution buffer.
Purified samples are quantified for nucleic acid purity and concentration utilizing NanoDrop instrumentation. Acceptable concentration range is between 3-24 ng/ul, and acceptable 260/280 ratio is between 1.5-187. All four purified samples passed quantification.
Batches of 40 Oral Panel reaction plates are prepared at a time and stored at -20oC. Each 96 well plate contains 88 unique sets of species-specific PCR primers, five positive controls and one negative control. A multichannel pipette is employed to dispense 3 ul of purified DNA per reaction well containing typical PCR reaction components. The plates are sealed with thermal films and amplified in Bioer Thermocyclers on a 23-step annealing gradient profile.
Amplification products are run on 1.2% agarose gels, with products ranging in size from 198bp – 1020bp, visualized with ultraviolet light and ethidium bromide stain.