by David T. Zava, PhD
The use of saliva and finger-prick capillary blood (dried blood spot – DBS) for testing sex steroid hormones (estradiol – E2, progesterone – Pg, testosterone – T) was developed out of the need to circumvent some of the problems and inconveniences of collecting venipuncture blood. Comparison of saliva and capillary DBS has shown that when these hormones are produced endogenously, they show excellent correlation with serum/plasma tests,1,2 and to some extent urine sex steroid metabolites.
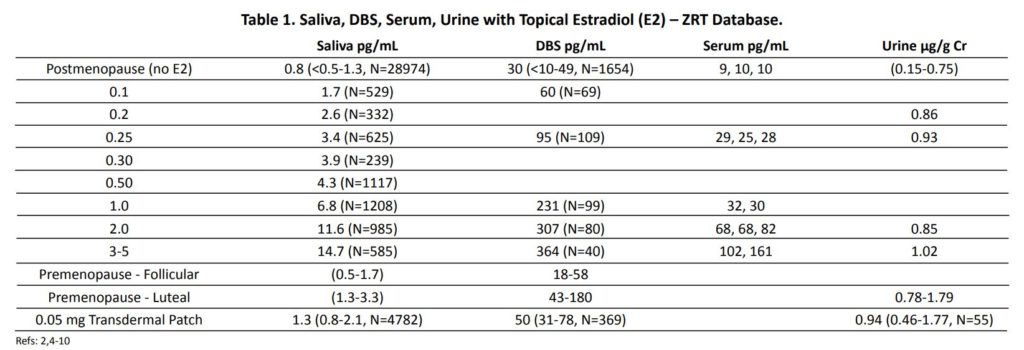
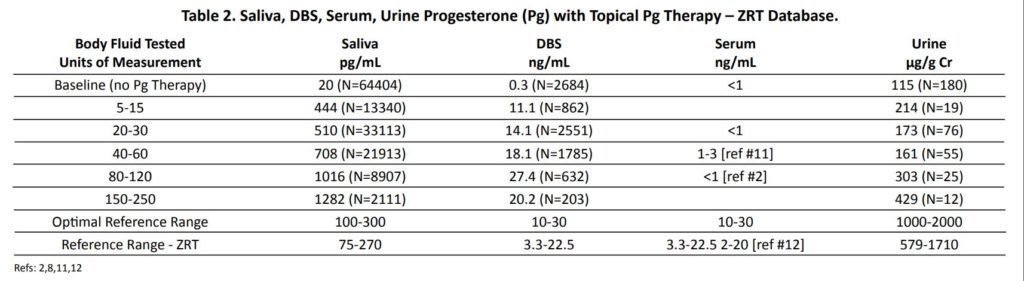
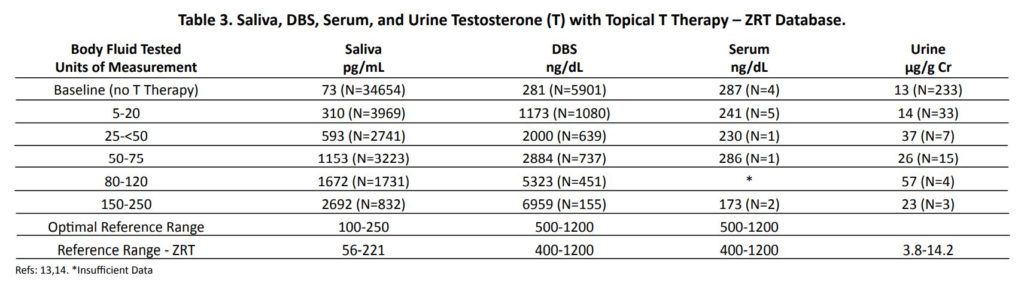
While the quantitative equivalencies of saliva, capillary blood, and serum/plasma are excellent when hormones are produced endogenously, we and others2,3 have shown that with topical (percutaneous) delivery of sex hormones, saliva and capillary DBS levels of hormones are strikingly different from conventional venipuncture serum and urine levels of the supplemented hormones. Topical steroid hormone therapy with increasing dosage results in very little, or only a very slight, dose-related increase in conventional venipuncture serum or urine metabolite levels of the dosed hormone (Tables 1-3). In striking contrast, topical dosing results in a relatively linear dose dependent escalation of hormone in saliva and capillary blood DBS. In fact, saliva and capillary whole blood levels for the sex hormones delivered topically no longer show quantitative equivalence and often exceed serum levels by as much as 10-to-100-fold.2
Because topical sex hormone therapy at physiological dosing has little impact on venipuncture serum or urine levels of the dosed hormones but raises salivary and capillary blood levels to high physiological levels, this has led to the question of what topical dose (physiological or pharmacological) is more effective and appropriate for achieving physiological levels of hormones in tissues. It also begs the question: why are saliva and capillary blood levels so much higher, and serum and urine levels so much lower, with conventional pharmacological dosing of topical E2 and Pg in women and topical T in men, as seen in Tables 1-3?
Most noteworthy and often unappreciated is that physiological dosing with the sex hormones, meaning that the dose used topically is equivalent to the amount of sex hormone produced daily by the ovaries, testes, and/or adrenal glands (see Table 4), leads to physiological levels in saliva and capillary blood (see Tables 1-3), but has little effect on increasing serum or urine levels from low menopausal/andropausal to healthy levels seen in young females and males (Table 4)
While physiological dosing of topical E2 (0.1-0.5 mg) and Pg (10-50 mg) in postmenopausal women and topical T (5-20 mg) in older men (>50 y/o) raises the capillary blood and saliva levels to physiological levels seen in healthy premenopausal women (Table 4) and in younger men, little change is seen in serum or urine levels until dosing approaches high physiological or pharmacological amounts (Tables 1-3).
At the peak of the luteal phase (about days 19-21 of the menstrual cycle) where daily Pg production by the ovaries ranges from about 5-30 mg, venipuncture serum and fingerstick capillary blood (DBS) Pg levels are quantitatively nearly equivalent at about 5-25 ng/mL, with saliva about 1-2% of blood levels at about 50-300 pg/mL, and urine pregnanediol, a surrogate for Pg, levels are about 500-2000 µg/g Cr (Table 2). To achieve premenopausal luteal physiological ranges in postmenopausal women with topical Pg therapy only requires physiological dosing (10-30 mg) when measuring saliva and capillary whole blood2,15 (Table 2). Even at pharmacological dosing with topical Pg, serum and urine never even reach physiological levels.2,3,11,15
Even with pharmacological topical sex hormone dosing, serum and urine levels of E2 in women and T in men rarely increase even to within mid-physiological ranges. Pharmacological dosing with E2 (>1-5 mg) in postmenopausal women, and T (>50-200 mg) in hypogonadal men16, only increases serum and urine E2 and T from low to mid-physiological levels (Tables 1 and 3).
When T is synthesized endogenously by the testes at about 3-7 mg/day, serum/ plasma and capillary blood levels of T in healthy men are quantitatively near equivalent (optimal range about 400-800 ng/dL), and salivary levels are at about 2% of serum/capillary blood T levels (optimal range about 80-160 pg/mL). When topical T is used in hypogonadal men (serum T <300 ng/dL) at FDA-approved pharmacological dosing (50-200 mg), it distributes into saliva and capillary blood at very high levels, with saliva and DBS levels of T about 10-to-20-fold higher (median ranges about 800-2500 pg/mL in saliva and 3000-7000 ng/dL in DBS – Table 3).
In sharp contrast, this pharmacological dosing only increases T to midphysiological range of about 400-600 ng/ dL in serum, as reported by others.13 In parallel with serum, urine levels rise only slightly with pharmacological T dosing. In sharp contrast to pharmacological dosing (50-200 mg), topical dosing more in the physiological range of about 5-20 mg of T has little to any impact on serum/ plasma or urine levels of T, but increases capillary blood T from hypogonadal to mid-range levels seen in healthy young men (500-800 ng/dL) (Table 3). The lack of a significant increase in serum and urine levels of topically delivered sex hormones to physiological ranges (Table 4) at physiological dosing (i.e., about 50-300 µg E2 and 5-30 mg Pg in women and 5-20 mg T in men) (Tables 1 and 3), has resulted in justification of dose escalation of FDA approved and compounded products to amounts that are 10-to-20-fold higher (i.e., 500-5000 µg E2 and 100-300 mg Pg in women and 50-200 mg T in men) than levels of these hormones that are produced daily by the gonads of healthy young women and men (Table 4).
These data suggest that at least for topical E2 and Pg in women, and topical T in men, serum and urine underestimate by at least 10-fold the amount of topically delivered hormones distributed to the salivary gland and capillary beds of the fingertip, which are likely representative of other tissues throughout the body.