Joseph Shen, MD, and
Raffi Bianchi Shen (editor)
This article is an edited and updated version of Chapter 12, “Multifunction Cardiogram, a.k.a. MCG” in Mark Houston’s book Personalized and Precision Integrative Cardiovascular Medicine (1st Edition).
Coronary artery heart disease (CAD), a subset (~15%) of ischemic heart disease, is a significant cause of death and disability in developed countries worldwide. Despite purported decreasing mortality rates over the past four decades (a questionable conclusion), ischemic heart disease due to obstructive CAD (an obsession or a religious belief of the entire cardiology field) remains the cause of about one-third of all deaths among individuals over 35. About one-half of all middle-aged men and one-third of middle-aged women in the United States will develop some manifestation of CAD, actually a late sign of metabolic dysfunctions due to eating processed “food,” a sedentary, stressful lifestyle, and environmental toxins with several unrecognized drivers or causes of this morbidity; the condition persists despite our general knowledge of significant risk factors based on population data such as the antiquated Framingham Heart Study.
Essential factors in this deficiency of medical care have been the lack of adaptable, inexpensive, noninvasive, and accurate modalities to detect early expressions of metabolic dysfunctions in their early stages and the lack of effective monitoring of the effects of diet and other safe and effective upstream lifestyle interventions before the late-stage sicknesses arise.
ECG stress testing, nuclear scintigraphy, stress echocardiography, and other various cardiac stress imaging testing types are the standard noninvasive techniques for evaluating cardiac ischemia. While these are recognized as sensitive tests for detecting CAD in two or more large epicardial vessels with 75% blockages (perhaps too little and too late), it has been widely acknowledged that they have relatively poor specificity, as shown by definitive evidence of many false positive results. There is a growing consensus that this lack of specificity results in many unnecessary coronary angiographies, thereby subjecting many patients to the potential risks of invasive procedures and radiation exposure without expected and shamelessly promoted commensurate clinical benefits, based on the evidence of the 10-year (still ongoing) and 100 million dollars “Ischemia Trial.”
For example, in 2010, Patel and colleagues published an analysis of the American College of Cardiology National Cardiovascular Data Registry, which included 397,954 patients without known CAD undergoing elective angiography. (70% obstruction or greater), When catheterized, 149,739 patients (37.6%) had obstructive coronary artery disease requiring an interventional procedure. This means, stated bluntly, that up to 62.4% of those patients could have avoided coronary angiography if more accurate noninvasive testing modalities had been available. Compounding the diagnostic inadequacy of conventional testing of obstructive CAD is the emerging consensus on the role of non-obstructive coronary and microvascular disease following years of metabolic dysfunction and hyperinsulinemia in the clinical manifestation of ischemic heart disease.
The Purpose of This Chapter
This chapter provides an opportunity for any health professional to learn about a “new” diagnostic tool that has been more than 20 years in the making. It outlines why conventional cardiac testing is inadequate and why this new tool, the Multifunction Cardiogram or MCG, is the ideal tool to fulfill this unmet need.
There have been several paradoxical or unexpected clinical developments in the management of CAD over the last several years. For example, while it is generally accepted in the legacy mainstream that LDL cholesterol plays a central role in the initiation of coronary plaque, it is also known that 50% of patients presenting with myocardial infarction (MI) have normal total cholesterol. Additionally, the data from several primary and secondary prevention trials have shown that the majority of the risk of CAD remains even after LDL reduction. The trillion-dollar big-pharmaceutical industrial complex statin push has yielded abysmal outcomes.
Perhaps the most glaring example of the inadequacy of the conventional approach to managing CAD is the COURAGE trial’s outcome status report. The 15-year status of this study essentially demonstrated that PCI (stent placement) in patients with stable CAD did not improve in mortality outcome compared to similar patients who were treated using only optimal medical management.
Perhaps related is an older but exciting piece of data from the FAME study as well, which looked at one–year outcomes (death, MI, major adverse cardiovascular event) in one group of patients whose management was guided by angiographic results versus a similar group headed by the fractional flow reserve (FFR) data, with the FFR–guided group demonstrating significantly better outcomes in all categories. The impact of hyperinsulinemia, oxidative stress of eating processed “food,” living stressful lives, neurohormonal, psychiatric disorders, infectious agents, viral, bacterial, fungal, and exposure to environmental toxins, or conditions, such as space travel, deep sea diving, and high altitudes, have been sidelined and willfully ignored. A systems approach is desperately required to address the functional aspects of this complex biological problem to give the patients the quantitative, reliable, non-invasive, safe, and effective physiological reasoning behind the call for an optimized lifestyle reshuffle.
Most importantly, the root cause of 90+% of cardiovascular diseases and 70% of cancers are based on metabolic dysfunctions. All the current conventional imaging cardiology tools, including the gold standard coronary angiography, do not detect abnormal functional expressions contributing to metabolic dysfunctions. This lack of a better, accurate, and early detection bedside tool is probably a significant contributor to the sudden premature deaths of middle-aged or even younger people, more women than men. A review in Circulation (1995) by Erlin Falk demonstrated that the progression to plaque rupture and myocardial infarction over time occurs most frequently in patients with obstruction of 50% or less.
It is within this context of complex and evolving concepts that Premier Heart is proud to introduce the Multifunctional Cardiogram (MCG), a noninvasive, physical-stress-free, and non-ionizing diagnostic tool that can be used to quantitatively assess the lesions across the very early stage non-obstructive to obstructive spectrum.
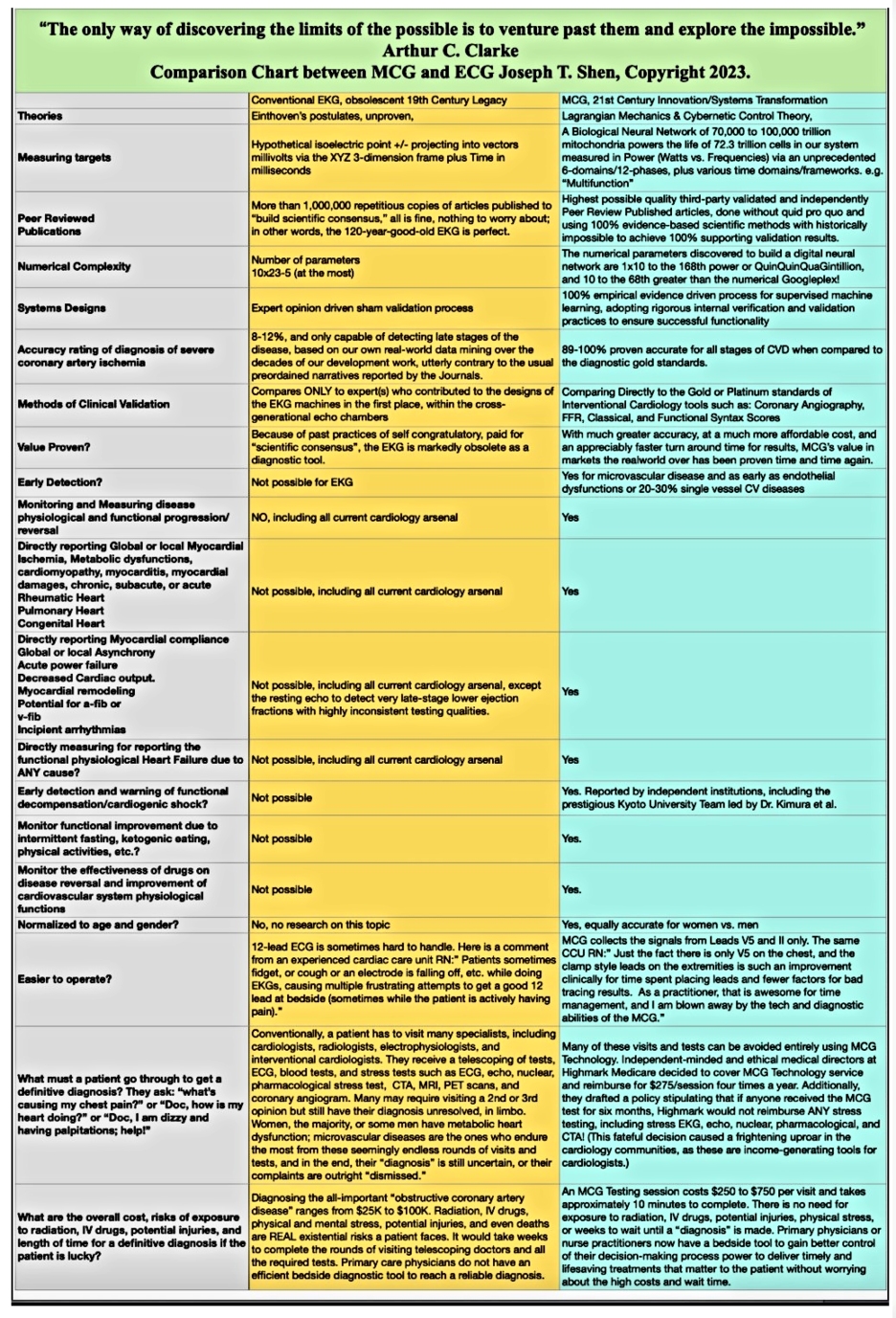
CLICK HERE https://mcgdoc.substack.com/p/a-side-by-side-comparison-chart-between FOR A CLEARER VERSION OF THE CHART
What Is MCG and What Does It Measure?
The Multifunction Cardiogram (MCG) is the first embodiment of a mathematical application of systems theory to a dynamic biological (cardiovascular) environment that expresses the physiological state of the heart, with a primary focus on the level of its ischemic burden. In other words, the MCG describes the dynamic functional state of the cardiovascular system beyond relying upon anatomical status.
Premier Heart’s greatest priority was measuring the biological neural network of the human body’s cardiovascular system in power (watts vs. frequencies) via an unprecedented six domains/twelve phases, plus various time domains/frameworks—thus, the “Multifunction.” Our primary focus is on detecting functional alterations caused by ischemic burden.
However, additional markers needed to be recruited to describe the cardiovascular system’s power distribution and dynamics from a practical and valuable perspective. That expression is the mathematical articulation of the communication between two standard ECG leads over multiple cycles, beginning with converting the signals into a frequency domain via multiple non-linear mathematical functions, thus coining the term “multifunction cardiography.” The adaptation of systems analysis principles, combined with Lagrangian mechanics, empirical data mining, deep machine learning, and neural network development, created, to our knowledge, the first example of a commercially available information technology solution in the discipline of “Clinical Computational Electrophysiology.”
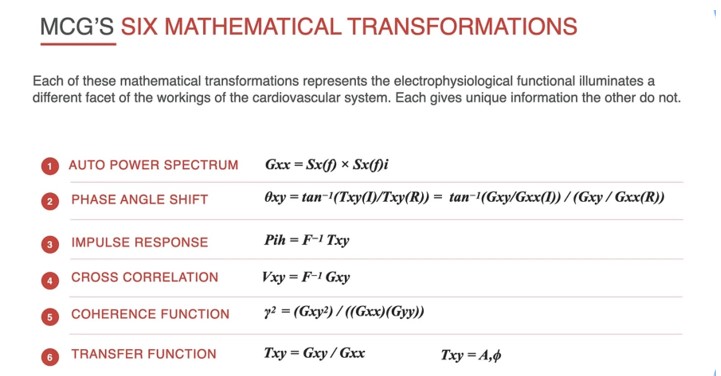
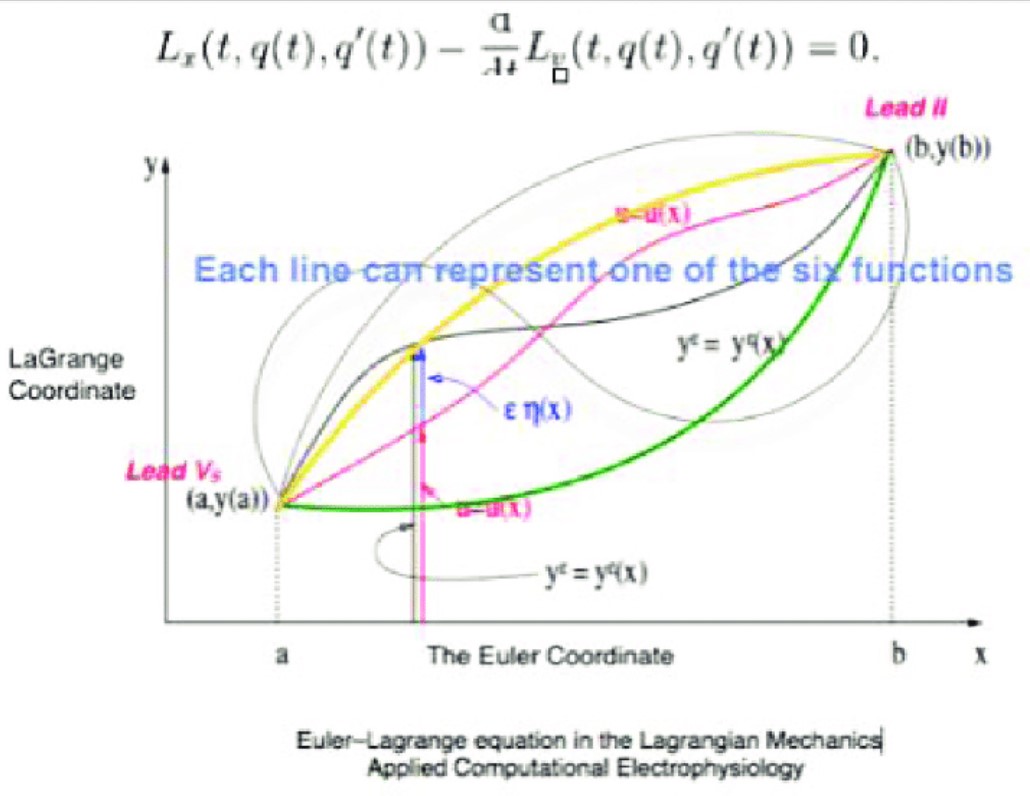
To illustrate the six mathematical transformations, please see the graphics above. Note that the applications of AUTO POWER and CROSS POWER spectra in MCG technology are used to directly measure the mitochondrial bio-neural network’s dynamic expressions in real-time.
Following decades of research and development, through the diligent work of two generations of dedicated scientists, clinicians, and engineers, MCG technology has evolved from conceptual mathematical designs to animal testing and finally to human application. While X-ray, computed tomography (CT), magnetic resonance (MR), or ultrasound technologies describe spatial anatomic separation, MCG describes frequency separation, where specific mathematical elements from the multiple functions in frequency domains are ascribed to particular anatomical or physiological functions of the entire whole cardiovascular system.
It is beyond the scope of this chapter to delve into a full explanation of the applied Lagrangian mechanics used by this technology. However, it is still helpful to outline a few basic principles. Blood flow is a non-Newtonian fluid optimally assessed and reported with Euler coordinates. Cardiac tissue and brain tissue are viscoelastic solids, and they are evaluated and reported with LaGrange coordinates. Among this system’s infinitely possible mathematical expressions, we have empirically selected six (6) dynamic and integrative mathematical functions that act as the backbone of our mathematical analysis: auto power spectrum, phase angle shift, impulse response, cross-correlation, coherence function, and transfer function. A Laplace transformation application then links the Euler and LaGrange coordinates. (See Figure 1)
Physiologically, for the first time, directly linking the underlying metabolic dysfunctions of the cardiovascular system to the early onset of insulin resistance and most chronic diseases objectively and quantitatively for early intervention and disease reversal; these include hypertension, ischemic heart disease, diabetes-related complications, stroke, and cancer, to list the top targets.
Quantifying the abnormal electromechanical dynamic expression patterns of stress (physical), strain, myocardial structures, and intra-cardiac blood flow from the earliest stages of the dysfunctions to understand the root causes physiologically and fundamentally to the end-stage to enable primary and secondary preventions for potential disease reversal to save lives at affordable costs in a digitized, scalable manner thanks to computational power.
Integration of all myocardial electrical power required to function under normal and abnormal conditions delivered by sodium (Na+), hydrogen (H+), potassium (K+), calcium (Ca++), magnesium (Mg++) channels and the biological network of 700,000 to 100,000 trillion mitochondria and their mitochondrial ATPase activities of all myocardial cells through multiple cardiac cycles to monitor progressions of ANY disease processes objectively and quantitatively. We need an equally complex system with a massive numerical advantage to wrap our arms around: by applying multiple functions expression of the dynamic expressions of the 70,000 to 100,000 trillion mitochondrial biological neuronetwork’s power output of the cybernetic principle, the empirically discovered “quinquinquagintillion” numerical complexity, which equals to 1,000,000 trillion parameters, 10X of the numbers of mitochondria, delivers that required analytical capability.
Measurement of oxidative stress caused by supply and demand imbalances, free radical formation, and lactic acidosis leading to ion channelopathies, particularly the gradient-dependent H+ channel (a subunit of F1-F0 ATPase) in addition to chronic damage/mutation of the mitochondrial gene transcription/translation mechanics, resulting in gradual myocardial power production deficiency. This information is critical for solving the lack of understanding of the underlying conditions that lead to premature death.
Most importantly, overall power production malfunctions due to mitochondrial dysfunctions due to multiple root causes, including but not limited to a sedentary lifestyle, overconsumption of alcohol, branched-chain amino acids, fructose, processed foods, seed oils, heavy metal toxins, exposure to chronic stress, numerous inflammatory causes, etc.
Ultimately, all diseases bear a metabolic origin; inevitably, the missing information gap, which our work has discovered and resolved, will change how we manage health from its source—by identifying early signs of metabolic dysfunctions directly downstream of mTOR (cell proliferation), AMPK (component building), and P13K (cell entry) pathways, and reversing them before too late.
Our dream: Our discoveries will fundamentally change the trajectory of future medicine to a sound and 100% evidence-based, patient-centric practice of early detection, primary lifestyle optimization, and decision-making aiming for the best outcomes at the lowest costs to the patients.
All this information and analyses are collected and collated by a bedside device within ten minutes on the average patient. The device itself is the size of a standard laptop. Electrocardiographic signals from two leads (II and V5) are recorded for 82 seconds per cycle and repeated 3 to 5 times per session. Data is then uploaded and compared to the patterns of hundreds of thousands of patients who have had the MCG test and had cardiac catheterization with an angiogram. The database also contains an equal split of males/females to eliminate gender bias, with an age range of 14 to 100. In effect, every patient with an MCG test in development undergoes a test with equivalent accuracy to a cardiac catheterization with an FFR assessment.
The database itself is the end product of a laborious effort central to understanding MCG technology and may be the most uniquely constructed database in the medical data industry. The team, led by Dr. Shen, embarked on a multi-decade-long journey of research and development via digital signal processing, empirical clinical data collection, data mining, supervised machine learning, deep-learning neural network development, artificial intelligence algorithm development, and countless iterations of painstakingly vetted and trained real-world datasets for algorithmic optimization and improvement to create computer recognition of all forms of heart disease. In this endeavor, two million individuals were tested on MCG. Over 200,000 people with various heart diseases had their angiographic data strategically added to the system to build a production database for software development. All the data sets used in the analysis and the proposed statistical models had to satisfy the Null Hypothesis and Alternative Hypothesis tests.
The exceptionally carefully verified and validated data sets were used to discover over 200+ mathematical elements from the six non-linear functions. We ensured that the development of the machine learning algorithms for the quantitative automatic heart disease pattern classification and differentiation was based purely on thoroughly vetted and trusted empirical evidence. Based on the well-defined frequency and separation, the aim was to systematically explore, define, express, measure, quantify, and differentiate the hidden NORMAL and ABNORMAL expressions of electromechanical, electro-structural, electro-biochemical, electro-hematic, electroneuroendocrine or neurohormonal, electro-immunological, and the highly elusive, yet vitally critical diverse electro-myocardial perfusion patterns of the cardiovascular system. It is this kind of unique analysis, coupled with the 24/7 accessibility and reliability, that positions MCG well beyond more expensive and cumbersome imaging and perfusion techniques.
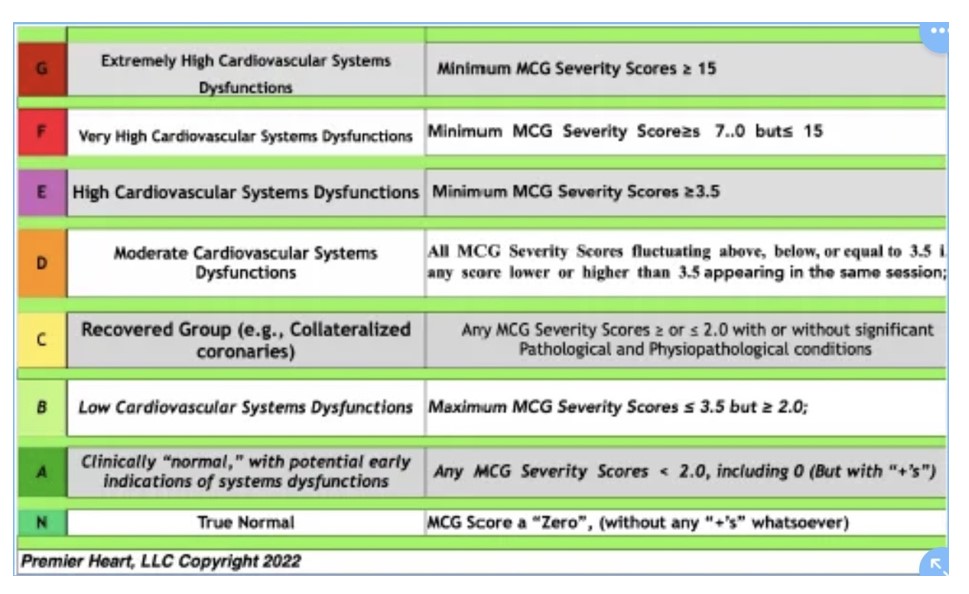
The final report gives an overall functional severity score between 0 (baseline normal) and 22 (the most deadly severe). The report also provides an assessment of secondary pathological and physiopathological conditions. These secondary conditions or makers include the following: cardiomyopathy (wall motion derangements), hypertrophy, arrhythmias or precipitating substrates, rheumatic pattern (LV, aortic/mitral valve derangements), pulmonary pattern (right heart, pulmonic/tricuspid valve derangements), myocardial damage (myocardial infarction, contusion, etc.), congenital abnormalities, compliance changes, remodeling, energy output, ejection fraction, phase shift, etc.
While there is a generally good correlation between the severity score and the level of obstruction, although more so to the FFR measurements, there is no specific numerical correlation between the severity score and the percentage of blockage. This fact underscores the contribution of the secondary factors to the functional assessment of the heart and highlights the difference between conventional anatomical imaging and MCG’s functional physiological assessment. It also underscores the importance of the FFR information alluded to in the above-mentioned FAME study.
Over the years of learning from real-world data, we noticed an underlying metabolic component for most abnormal expressions, including global or local ischemia, myocardial inflammation, cardiomyopathy, and abnormal impulse response and phase angle shift functions. Most abnormal high functional severity scores can be reversed following simple lifestyle optimization without medical intervention. The effectiveness of ANY treatment can now be evaluated objectively using the technology.
Also, we have learned that cases with a long history of chronic cardiovascular diseases, such as high blood pressure, diabetes, and coronary artery disease, undergoing medical and interventional treatments, all have the same underlying metabolic component responsive to the same lifestyle optimization. The improvements or the short, intermediate, and long-term outcomes are measurable objectively via the categories based on the MCG severity scoring applications.
To validate that our technology works in the real world, I traveled extensively to seven countries in North America, Asia, and Europe. I found independent, highest-quality clinical investigators with the same worldview and values to validate our technology without corrupt intent and ANY quid pro quo. The next section of this article describes this decade-long effort to complete the first series of third-party clinical validation for peer-reviewed publications to inform the physician and the public.
Townsend Editor note: Section II will be in a future issue of Townsend e-Letter. More information about MCG is available at the following links:
- This is Part I/III of the revised chapter published initially in Mark Houston’s Biomedical Textbook “Personalized and Precision Integrative Cardiovascular Medicine.” https://open.substack.com/pub/mcgdoc/p/the-cross-generationallifetime-work?r=q7iae&utm_campaign=post&utm_medium=web
- Revised chapter part II/III, “The Journey to Freedom of a Recovered Physician,” describes our experience honestly and ethically conducting the independent third-party clinical validation without the business as usually corrupt “pay to play” schemes or without ANY quid pro quo: https://open.substack.com/pub/mcgdoc/p/the-journey-to-freedom-of-a-recovered?r=q7iae&utm_campaign=post&utm_medium=web
- My DropBox Folder is organized to provide ALL the peer-review published papers and presentations performed by ourselves or by independent third parties:https://www.dropbox.com/sh/a9pg6te0ifn9o16/AAAVM-ZqeJbgs1E4kZJjgPyOa?dl=0
- Two case reports demonstrating the unique capabilities of our technology to help patients with “Syndrome X” – the first, a retired ICU nurse who suffered repeated debilitating chest pains and tested “normal” on ALL her cardiology tests under the sun, then MCG came to her rescue: https://open.substack.com/pub/williamhbestermannjrmd/p/women-with-repeated-chest-pain-and-711?r=q7iae&utm_campaign=post&utm_medium=web; a 43-year-old overweight type two diabetic also who suffered repeated debilitating chest pains and tested “normal” on ALL his cardiology tests under the sun, then MCG came to his rescue: https://youtu.be/HvzVqtcRDdk
- Our YouTube channel is created to educate and train customers:https://www.youtube.com/@premierheartllc7799
Published June 3, 2023
About the Author
Joseph T. Shen, a recovered physician, is the founder of Computational BioCybernetics & Lagrangian Mechanics Systems Engineering Technologies and Premier Heart, a company that produces the Multifunction CardioGram (MCG) technology. He was awarded the Medical and Science Achievement Award by the Women’s Heart Foundation in 2010 for his contributions to the development of MCG technology. Email: systemsmcg@icloud.com