By Erik Peper, PhD, BCB, and Richard Harvey, PhD
San Francisco State University
COVID-19 disproportionally affects older people with serious underlying medical conditions and non-white racial and ethnic minorities. Prevention may depend upon the initial dose of viral exposure and the individual’s immune system competence. Suggested are strategies to reduce viral dose exposure by increasing fresh air circulation and a list of factors that strengthen or weaken the immune system.
COVID-19 can sometimes overwhelm young and old immune systems and in some cases can result in ‘Severe Acute Respiratory Syndrome’ pneumonia and death (CDC, 2020). The risk is higher for older adults and people of any age who have serious underlying medical conditions such as hypertension, diabetes, obesity, heart disease, lung disease, emphysema, immunocompromised, kidney, and liver disease; and the burden of illness and death is disproportionate among non-white racial and ethnic minority groups (CDC, 2020a; CDC, 2020b). As we age, the immune system deteriorates (immunosenescence), which reduces the response of the adaptive immune system that needs to respond to the virus infection (Aw, Silva & Palmer, 2007; Osttan, Monti, Gueresi, et al., 2016).
Severity of Disease May Depend Upon Initial Dose of the Virus
In a brilliant article, “How does the coronavirus behave inside a patient? We’ve counted the viral spread across peoples; now we need to count it within people,” assistant professor of medicine at Columbia University and cancer physician Siddhartha Mukherjee points out that severity of the disease may be related to the initial dose of the virus. Namely, if you receive a very small dose (not too many virus particles), they will infect you; however, the body can activate its immune response to cope with the infection. The low-dose exposure acts similar to vaccination. If on the other hand you are exposed to a very high dose, then your body is overwhelmed with the infection and is unable to respond effectively. Think of a forest fire. A small fire can easily be suppressed since there is enough time to upgrade the fire-fighting resources; however, during a firestorm with multiple fires occurring at the same time, the fire-fighting resources are overwhelmed and there is not enough time to recruit outside fire-fighting resources.
As Mukherjee points out this dose exposure relationship with illness severity has a long history. For example, before vaccinations for childhood illnesses were available, a child who became infected at the playground usually experienced a mild form of the disease. However, the child’s siblings who were infected at home develop a much more severe form of the disease.
The child infected in the playground most likely received a relatively small dose of the virus over a short time period (viral concentration in the air is low). On the other hand, the siblings who were infected at home by their infected brother or sister received a high concentration of the virus over an extended period that initially overwhelmed their immune system. Higher virus concentration is more likely during the winter and in well insulated/sealed houses where the air is recirculated without going through HEPA or UV filters to sterilize the air. When there is no fresh air to decrease or remove the virus concentration, the risk of severity of illness may be higher (Heid, 2020).
The risk of becoming sick with COVID-19 depends on whether you are exposed to the coronavirus and the competency of your immune system. This can be expressed in the following equation.
This equation suggests two strategies to reduce risk: reduce coronavirus load/exposure and strengthen the immune system.
What to Do to Reduce the Coronavirus Load/Dose of Virus Exposure
Assume that everyone is contagious even though they may appear healthy. Research suggests that people are already contagious before developing symptoms or are asymptomatic carriers who do not get sick and thereby unknowingly spread the virus (Furukawa, Brooks, Sobel, 2020). Dutch researchers have reported that, “The proportion of pre-symptomatic transmission was 48% for Singapore and 62% for Tianjin, China” (Ganyani et al, 2020). Thus, the intervention to isolate people who have symptoms of COVID-19 (fever, dry cough, etc.) most likely will miss the asymptomatic carriers who may infect the community without awareness. Only if you have been tested, do you know if you have been exposed or recovered from the virus. To reduce exposure to the virus, avoid the “Three C’s” — closed spaces with poor ventilation, crowded places, and close contact (Dooley & Inoue, 2020)—and do the following:
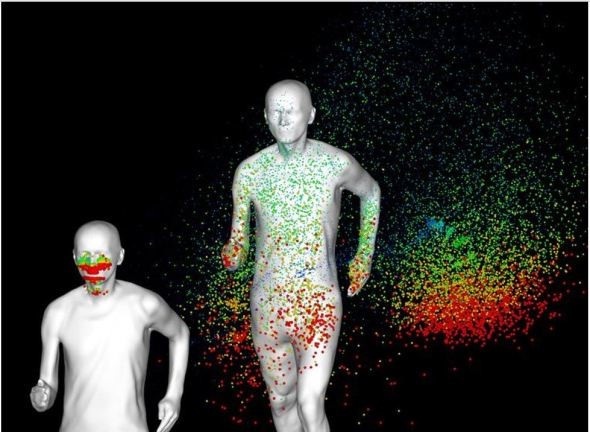
contain the virus extends behind the person in their
slipstream (photo from KU Leuven en TU Eindhoven).
The plume of exhaled droplets in the person’s slipstream
may extend more than 15 feet while walking and more
than 60 feet while jogging or bicycling. Thus, social
distancing under these conditions is much more
than six feet, and it means avoiding the slipstream
and staying much further away from the person.
1. Follow the public health guidelines:
• Social distancing (physical distancing while continuing to offer social support)
• Washing your hands with soap for at least 20 seconds.
• Not touching your face to prevent microorganisms and viruses from entering the body through mucosal surfaces of the nose mouth and eyes.
• Cleaning surfaces which could have been touched by others, such as door bells, door knobs, packages.
• Wearing a mask and gloves to reduce spreading the virus to others.
2. Avoid the person’s slipstream that may contain the droplets in the exhaled air. The purpose of social distancing is to have enough distance between you and another person so that the exhaled air of the other person would not reach you. The distance between people depends upon their activities and the direction of airflow.
In a simulation study, Professor Bert Blocken and his colleagues at KU Leuven and Eindhoven University of Technology reported that the plume of the exhaled air that potentially could contain the virus droplets could extend much more than five feet. It would depends upon the direction of the wind and whether the person is walking or jogging as shown above in Figure 1 (Blocken, 2020).
3. Increase fresh air to reduce virus concentration. By increasing the fresh outside air circulation, you dilute the virus concentration that may be shed by an infected asymptomatic or sick person (Qian & Zheng, 2018; Atkinson, Chartier, Pessoa-Silva, et al, 2009). Thus, if you are exposed to the virus, you may receive a lower dose and increase the probability that you experience a milder version of the disease. To increase fresh air (this assumes that outside air is not polluted), explore the following:
~Open the windows to allow cross ventilation through your house or work setting. One of the major reasons that the flu season spikes in the winter is that people congregate indoors to escape weather extremes. People keep their windows closed to conserve heat and reduce heating bill costs. Lack of fresh air circulation increases the viral density and risk of illness severity (Foster, 2014).
~Use exhaust fans to ventilate a building. By continuously replacing the inside “stale” air with fresh outside air, the concentration of the virus in the air is reduced.
~Use high-efficiency particulate air (HEPA) purifiers to filter the air within a room. These devices will filter out particles whose diameter is equal to 0.3 µ m. They will not totally filter out the virus; however, they will reduce it.
~Avoid buildings with recycled air unless the heating and air conditioning system (HAC) uses HEPA filters.
~Wear a mask to protect other people and your community. The mask will reduce the shedding of the virus to others by people with COVID-19 or those who are asymptomatic carriers. An N-95 mask will reduce personal exposure to the virus.
4. Avoid long-term exposure to air pollution. People exposed to high levels of air pollution and fine particulate matter (PM2.5) are more at risk to develop chronic respiratory conditions and COVID-19 death rates. In the 2003 study of SARS, ecologic analysis conducted among 5 regions in China with 100 or more SARS cases showed that case fatality rate increased with the increment of air pollution index (Cui, Zhang, Froines, et al. , 2003). The higher the concentration of fine particulate matter (PM2.5), the higher the death rate (Conticini, Frediani, & Caro, 2020). As researchers, Xiao Wu, Rachel C. Nethery and colleagues (2020) from the Harvard T.H. Chan School of Public Health point out:
A small increase in long-term exposure to PM2.5 leads to a large increase in COVID-19 death rate, with the magnitude of increase 20 times that observed for PM2.5 and all cause mortality. The study results underscore the importance of continuing to enforce existing air pollution regulations to protect human health both during and after the COVID-19 crisis
5. Breathe only through your nose. The nose filters, warms, moisturizes and slows the airflow so that airway irritation is reduced. Nasal breathing also increases nitric oxide production that significantly increases oxygen absorption in the body. During inspiration through the nose, nitric oxide helps dilate the airways in your lungs and blood vessels (McKeown, 2016). More importantly for COVID-19, nitric oxide, produced and released inside the nasal cavities and the lining of the blood vessels, acts as an antiviral and a secondary strategy to protect against viral infections (Mehta, Ashkar & Mossman, 2012).
How to Strengthen Your Immune System to Fight the Virus
The immune system is dynamic and many factors as well as individual differences affect its ability to fight the virus. It is possible that a 40-year-old person may have an immune system that functions as a 70 year old, while some 70 year olds have an immune system that function as a 40 year old. Factors that contribute to immune competence include genetics, aging, previous virus exposure, and lifestyle (Lawton, 2020).
It is estimated that 70-80% mortality caused by COVID-19 occurred in people with comorbidity who are 1) over 65, 2) male, 3) lower socioeconomic status (SES), 4) non-white, 5) overweight/obese, 6) cardiovascular heart disease, and 7) immune suppressed. The majority of these risk factors are the result of economic inequality and lifestyle patterns such as eating a Western inflammatory diet (Pollan, 2020).
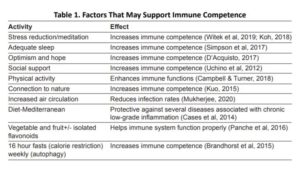
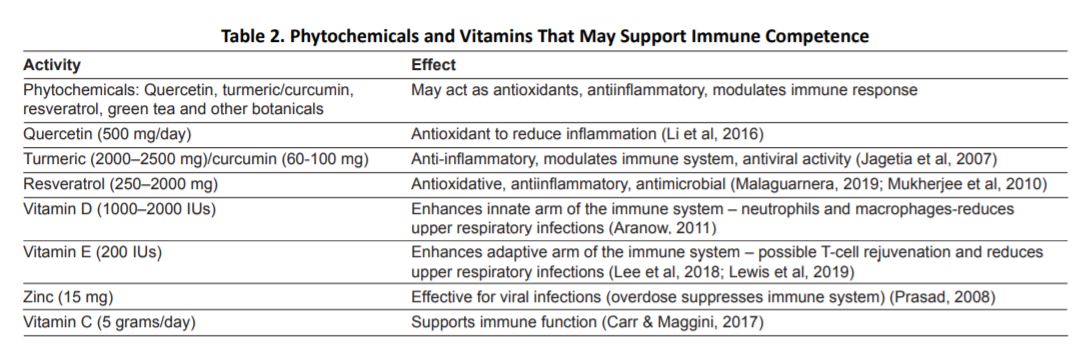
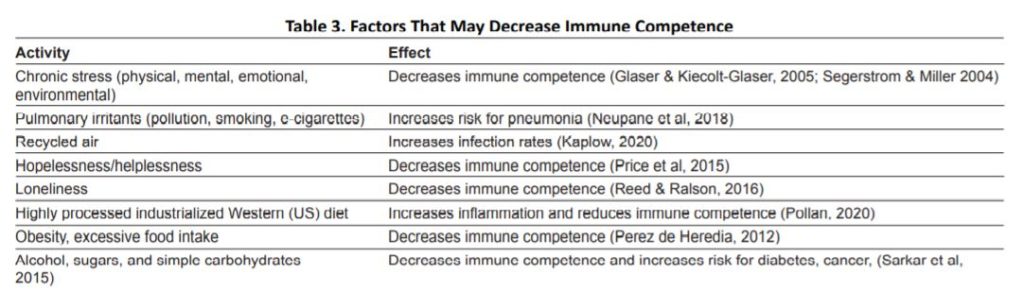
By taking charge of your lifestyle habits through an integrated approach, you may be able to strengthen your immune system (Alschuler et al, 2020; Lawton, 2020). Tables 1, 2, and 3, adapted from the published articles by Lawton (2020) and Alschuler et al, (2020), list some of the factors that may support or decrease the immune system.
Conclusion
An ounce of prevention is worth a pound of cure. Thus, to reduce the risk of COVID-19 disease severity, implement strategies to reduce viral dosage exposure and strengthen the immune system. Many of these factors are within our control. Thus, increase fresh air circulation, reduce stress, and reduce the intake of foods that tend to increase inflammation (the industrialized Western diet and a significant cause of chronic disease) and increase foods, vitamins, and nutrients that support immune competence.
Correspondence should be addressed to:
Erik Peper, PhD, Institute for Holistic Health Studies/Department of Recreation, Parks, Tourism and Holistic Health, San Francisco State University, 1600 Holloway Avenue, San Francisco, CA 94132 Tel: 510 681 6301 Email: epeper@sfsu.edu web: www.biofeedbackhealth.org blog: www.peperperspective.com.
This article is adapted from the blog, Reduce initial dose of the virus and optimize your immune system, https://peperperspective.com/2020/04/04/can-you-reduce-the-risk-of-coronavirus-exposure-and-optimize-your-immune-system/.