By Samantha Davison and
Bradford Case, ND, DC
Abstract
Small intestinal bacterial overgrowth (SIBO) is one of the leading causes of irritable bowel syndrome (IBS) and presents with a range of intestinal and extraintestinal symptoms that impair quality of life.1 Prescription standards of care, which include oral antibiotics such as rifaximin or metronidazole, have shown variable success and have proven to be economically unfavorable. This case report involves the successful treatment of hydrogen-positive SIBO with a broad-spectrum antimicrobial approach incorporating the use of berberine, oregano, neem,2,3 and a specific carbohydrate low FODMAP diet with marked reduction of gastrointestinal symptoms, improved Bristol stool chart, and improved integumentary symptomatology.
Introduction
Small intestinal bacterial overgrowth (SIBO) is an excessive amount of abnormal bacteria in the small intestine.4 Symptoms associated include abdominal discomfort, distention, bloating, dyspepsia, flatulence, belching, fatigue, nausea, diarrhea and/or constipation, sensation of incomplete evacuation, and urgency.4,5 Less frequent but more serious manifestations of SIBO include malabsorption, weight loss, anemia, iron deficiency, and vitamin deficiency.4
Risk factors may include anatomical abnormalities (i.e., small intestinal diverticulosis), postsurgical structural changes (i.e., ileocecal valve resection, gastric bypass, Roux-en-Y), iatrogenic causes of slow gut motility (i.e., narcotics, anticholinergics, anti-diarrheals), hypo- or achlorhydria due to surgery, autoimmune gastritis, or proton pump inhibitors, and small bowel dysmotility regardless of cause (i.e., inflammatory bowel disease, celiac disease, radiation enteritis, small bowel adhesions, and systemic diseases associated with dysmotility, which include diabetes, amyloidosis, and scleroderma) and trauma (i.e., traumatic brain injury).4
The most common diagnostic tests for SIBO include glucose or lactulose breath tests, small intestinal aspiration and culture, and assessment of clinical symptom profiles.4 Breath testing has proven to be the most economic, non-invasive, and reliable approach. This involves enumerating hydrogen and methane gas via breath samples over an indicated period of time, generally two or three hours. Gas production is dependent on the concentration and strains of bacteria colonized in the small intestine, availability of carbohydrate residue, and small intestinal absorptive capacity. The presence of these gasses in human breath signifies metabolism of carbohydrate residues by the gut, absorption across the gastrointestinal mucosal barrier, and sequentially, expiration through the lungs. These findings yield significance due to the inability of human cells to produce hydrogen or methane gases.6 When lactulose or glucose solution is given to a patient with suspected SIBO, changes in hydrogen and methane concentration in breath samples indicates the presence of SIBO.
The generalized treatment strategy for SIBO is induction of remission through eradication; maintaining remission and addressing etiology; restoring mucosal function; and balancing the microbiome. Conventional treatment remains empirical, using broad spectrum antibiotics for two weeks. Oral antibiotics such as rifaximin or metronidazole have shown variable success. Rifaximin is the safer and more efficacious drug of choice; however it has proven to be economically unfavorable for the patient and its long-term safety profile is unclear. Potential side effects of rifaximin include flatulence, headache, incomplete bowel emptying, urgency, abdominal pain, nausea, vomiting, constipation, fever, bloating, dizziness, fatigue and swelling.7
Alterative treatment strategies provide a least invasive approach to SIBO eradication, which generate restoration of the mucosal lining and mechanical function. The elemental diet provides essential nutrients administered in liquid form for several weeks and is a safe, exceptional option for patients with allergies or aversion to antibiotics. Herbal antibiotics in combination with a low FODMAP diet are the treatments of choice for most naturopathic or other naturally oriented physicians. In a non-randomized, open label trial, herbal antibiotics compared to rifaximin yielded comparative results indicating herbal treatment is as effective as rifaximin in patients with lactulose-positive SIBO breath tests.8
Case Study
A 23-year-old Caucasian male presented to Bastyr University California (BUC) Clinic in April 2021, with complaints of abdominal discomfort and dry skin. His abdominal pain had been ongoing for the past three years and was increasing in intensity. Pain was worse after eating, lasting around thirty minutes to one hour and was primarily in the epigastric region of his abdomen. The patient described his pain as dull with cramping and minor pains throughout the day that strengthened in severity after each meal. He also complained of cramping and burning flatulence, and belching, both of which were foul in odor. He noticed that his symptoms were particularly worse after eating high fat containing foods such as peanut butter, pork, fish, or fish oils, and further reported that he’d had issues digesting fats since he was 13 years old.
The patient also had an eczematous rash on the tips of his fingers, palms of his hands, calves, knees, abdomen, and back, which was previously and unsuccessfully treated with coal tar and salicylic acid. The rash was scaled, dry, pruritic, and occasionally presented with hemorrhagic fissures. Additional signs and symptoms included leukonychia and cold intolerance. His 24-hour dietary recall consisted of eggs, gluten-free toast, ramen, slices of ham, vegan sausage, potatoes, and a peanut butter and jelly sandwich. He passed 1-2 bowel movements per day, which were well-formed, type 2-3 on the Bristol stool chart, but hard to pass and malodorous. He denied noticeable blood, mucus, or undigested food in his stool.
Clinical Findings
Physical exam revealed a scaled rash with dry, flaking skin along his back, sides of abdomen, extensor surfaces of arms, lower limbs, and a scaled, white plaque over his right patella. Fissures were visualized along his fingers bilaterally with leukonychia on the nail bed of his left fourth digit. Capillary refill was less than two seconds. Abdomen appeared flat. Bowel sounds were heard in all four quadrants with scattered dullness on percussion. The abdomen was soft with no hepatomegaly, but tenderness was noted in the right lower quadrant on palpation.
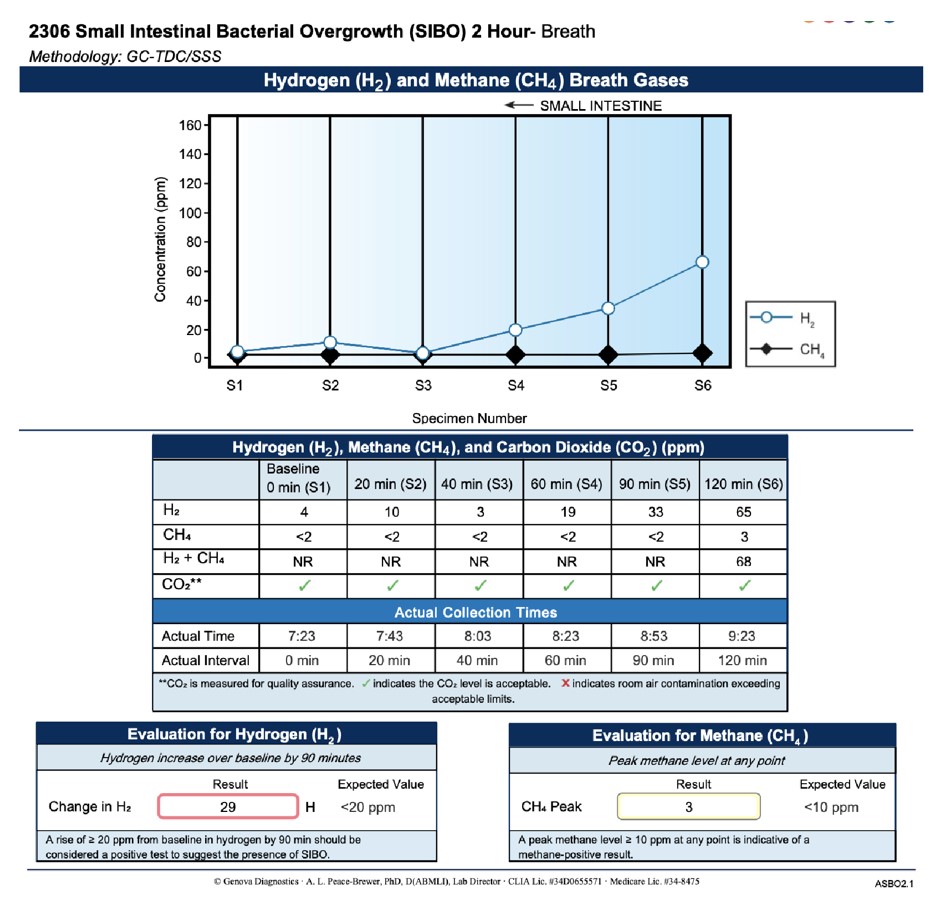
Laboratory analysis consisted of CBC with differential and comprehensive metabolic panel that were within normal limits, and a lipid panel showing low HDL. The lactulose breath test revealed a hydrogen level of 29 ppm at 90 minutes from baseline indicating hydrogen positive SIBO. Methane was negative, with a level of 3 ppm at 90 minutes and 120 minutes from baseline (Image 1).
Timeline
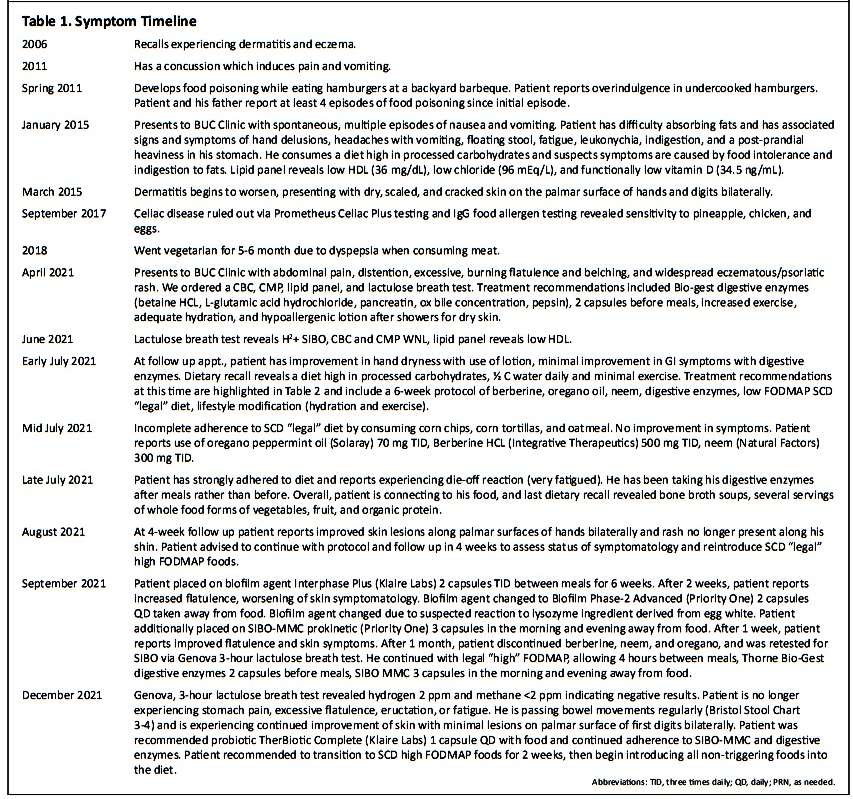
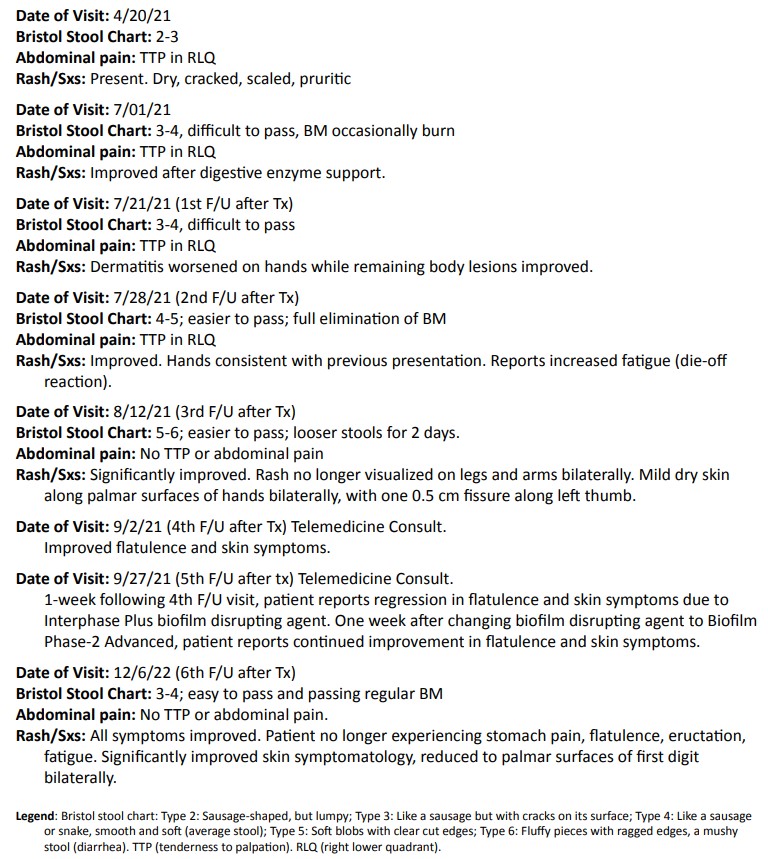
Upon taking a thorough history (Table 1), we discovered the patient began experiencing dermatitis and eczema around 2006. In 2011, he endured a concussion. In that same year, he also contracted gastroenteritis after eating undercooked beef. In 2015, the patient presented to Bastyr University Clinic with episodes of nausea and vomiting, which occurred sporadically a few times each year. At this visit, the patient and his father noticed a pattern of malabsorption when consuming foods high in fat. He further experienced signs and symptoms of hand delusions, headaches with vomiting, steatorrhea, fatigue, leukonychia, indigestion, and a post-prandial heaviness in his stomach. He consumed a diet high in processed carbohydrates and suspected symptoms were caused by food intolerance and indigestion of fats. Lipid panel revealed low HDL (36 mg/dL), low chloride (96 mEq/L), and functionally low vitamin D (34.5 ng/mL). Shortly after, in March 2015, his dermatitis began to worsen and presented with dry, scaled, and fissured skin on the palmar surfaces of his hands and digits bilaterally. In September 2017, another provider established celiac disease as unlikely via Prometheus Celiac Plus testing and IgG food allergen testing revealed sensitivity to pineapple, chicken, and eggs. As the patient’s dyspepsia with meat consumption worsened, he voluntarily began following a vegetarian diet for six months. The patient’s symptoms continued to worsen until seeking naturopathic care in April 2021.
Diagnostic Assessment
Results of the patient’s lactulose breath test are highlighted in Image 1. Given the results were conclusive for hydrogen positive bacterial overgrowth, we were able to confirm a positive diagnosis of hydrogen dominant SIBO. Treatment may range from six to twelve months and prognosis is individualistically dependent upon the patient’s adherence and physiological response. While herbal antibiotics have been shown clinically and statistically analogous to Rifaximin in SIBO eradication, herbal antibiotics induce worse Herxheimer reactions, i.e., flu-like symptoms including headache, joint and muscle pain, sore throat, malaise, sweating, chills, and nausea, compared to antibiotics. While this is largely understudied, the primary theory is that many patients have concomitant small intestinal fungal overgrowth (SIFO), likely caused from candida and their consequential biofilms. Herxheimer reactions may persist while targeted treatment disrupts biofilm integrity.9 Herxheimer reactions to SIBO eradication are successfully mitigated with activated charcoal as needed.10
Therapeutic Intervention
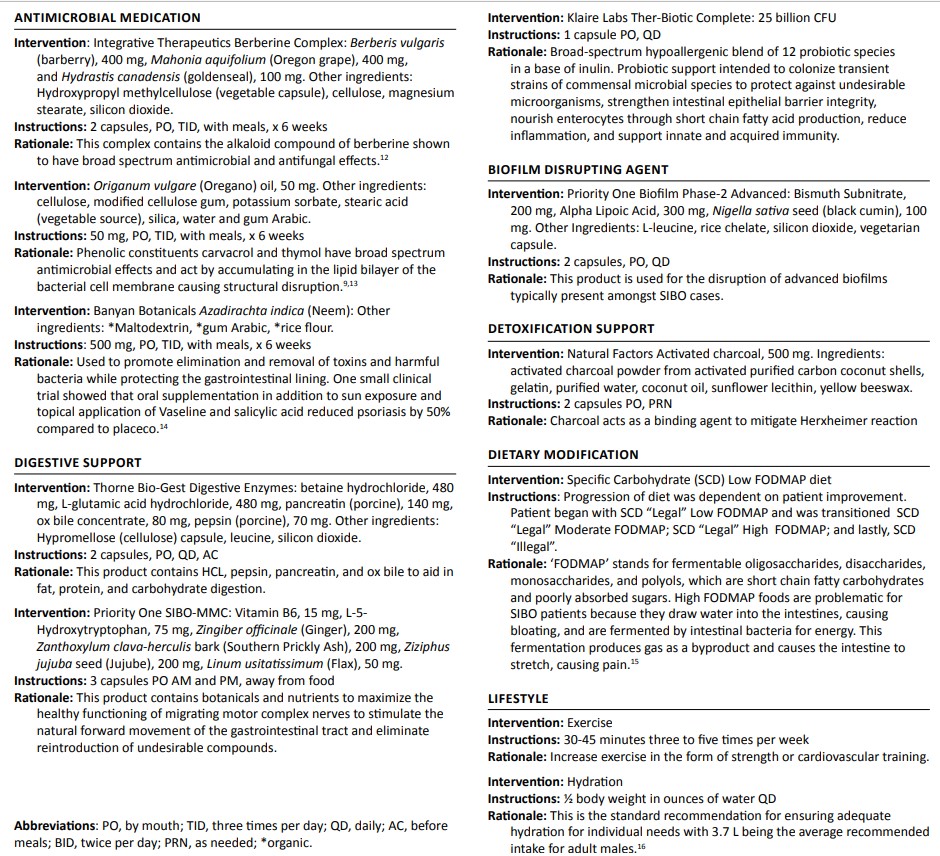
This patient had 10 visits in six months and received therapeutic interventions—antibacterial medication, dietary supplementation, nutritional and lifestyle recommendations—guided by laboratory testing (Image 1 and Table 2). Obstacles to cure at the time of initial treatment included dietary compliance, inadequate hydration, and inadequate physical exercise. Our treatment goals were to increase stomach acid, thereby improving digestion and absorption, and to eradicate small intestinal bacteria with use of the herbal antibiotics, highlighted in Table 2. Herbal therapy has been shown to be equivalent to Rifaximin in the treatment of SIBO.11 The following six-week supplementation protocol was originally developed by herbalist Steven Harrod Buhner and modified by Dr. Lela Altman. Our patient was initially placed on a six-week eradication protocol, including Integrative Therapeutics Berberine Complex, 500 mg three times daily; ADP Oregano Oil, 50 mg three times daily; Banyan Botanicals Neem, 500 mg three times daily; Thorne Bio-Gest Digestive Enzymes 2 capsules before meals; and a specific carbohydrate diet (SCD) in the “legal” low FODMAP category, developed by Dr. Allison Siebecker, reference Table 2 for detailed rationale. Additional determinants of health warranted recommendations to increase exercise 30-45 minutes three to five times per week in the form of strength or cardiovascular training and to ensure adequate hydration by consuming one-half of his body weight in ounces of water daily (Table 2).
As the patient’s gastrointestinal and integumentary symptoms lessened in severity, he was transitioned to the SCD “legal” moderate FODMAP diet for 4 weeks, then SCD “legal” high FODMAP diet for another four weeks.
Follow-up and Outcomes
At the patient’s three-week follow up, low FODMAP dietary adherence was incomplete due to daily consumption of high FODMAP foods including corn tortillas, corn chips, and oatmeal. The patient further reported that he was taking 70 mg of Solaray oregano with peppermint oil three times daily, 500 mg of berberine HCL three times daily, instead of the recommended berberine complex, and 300 mg of neem three times daily, instead of the recommended dose of 500 mg three times daily. Patient reported no improvement in symptoms at this time and was advised to follow the previously recommended therapeutic dosages. Through dietary counseling and patient education, complete adherence to the recommended protocol was achieved at the patient’s 4-week follow up. He had strongly adhered to the SDC legal low FODMAP diet and reported the Herxheimer reaction of increased fatigue.

At the patient’s six-week follow up, he reported significant improvement in symptoms with no abdominal pain, mild flatulence with distention after eating, and his skin symptoms had resolved along his legs, knees, arm, and elbows bilaterally. Mild dry and flaky skin was still noted along his first and second digits bilaterally and one 0.5 cm fissure was located along the palmar surface of his left thumb. The patient had experienced reconnection with his diet with increased consumption of clean protein sources and vegetables and reported no new onset of symptoms.
While there was an overall improvement in the patient’s presentation, symptoms of flatulence and distention indicated the persistence of SIBO, therefore, the patient was instructed to continue the herbal antimicrobial protocol, was transitioned to a SCD “legal” moderate FODMAP diet and instructed to incorporate more variety of fruits and vegetables. Patient was additionally placed on a biofilm disrupting agent, Klaire Labs Interphase Plus, 2 capsules three times daily, to reduce incidence of recurrence and potentiate effect of the herbal antibiotics.17
Atnine-week follow up, the patient was advised to discontinue Interphase Plus and initiate Priority One Biofilm Phase-2 Advanced, 2 capsules daily away from food, due to suspected reaction to lysozyme, an enzyme ingredient derived from egg white. Patient was advanced to the SCD “legal” high FODMAP diet for four-weeks duration. Treatment was further advanced to incorporate a prokinetic, SIBO-MMC, 3 capsules in the morning and evening away from food, to support the nerves of his migrating motor complex to stimulate the natural forward movement of the gastrointestinal tract and eliminate reintroduction of undesirable compounds.
At 13-week follow up, the patient reported complete resolution of symptoms. He was advised to discontinue berberine, neem, and oregano supplementation for a minimum of two weeks prior to three-hour Genova lactulose breath testing. Patient continued to adhere to the SCD “legal” high FODMAP diet in addition to eating his meals 3-5 hours apart to support his migrating motor complex. He continued to take digestive enzyme support and SIBO-MMC supplementation.
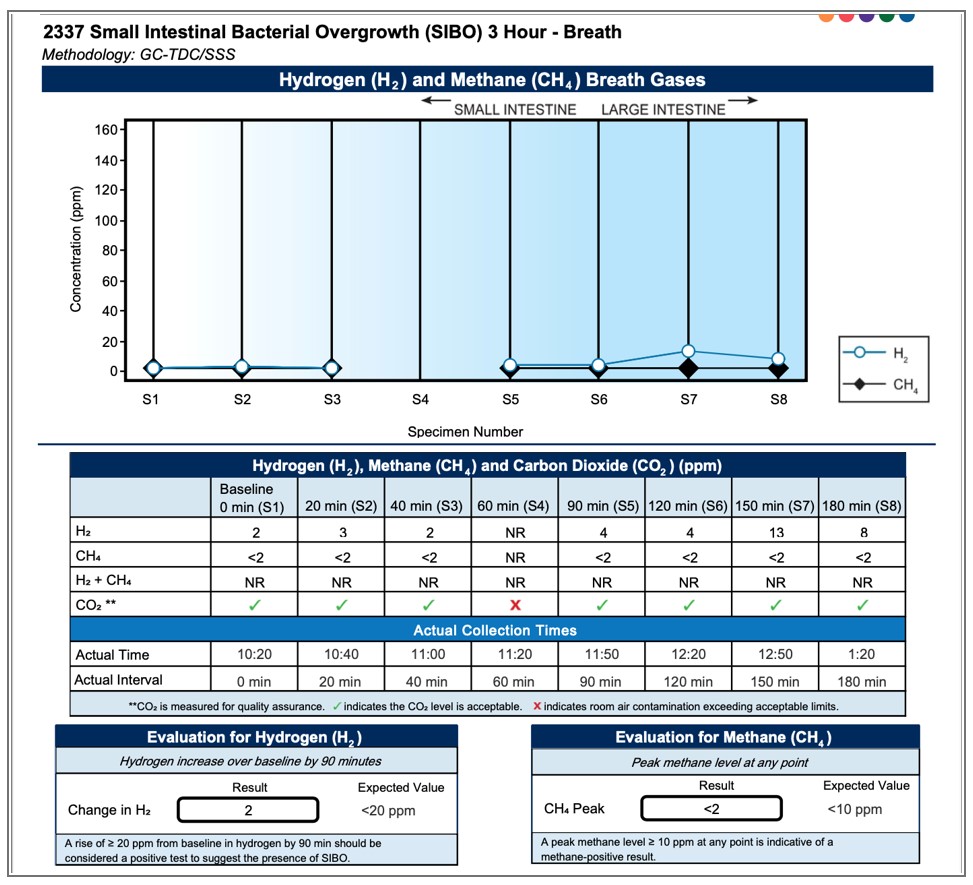
At the patient’s last follow up appointment, approximately 22 weeks after treatment initiation, Genova three-hour lactulose breath test (Image 2) revealed negative hydrogen (2 ppm) and methane (<2 ppm) results. Patient was no longer experiencing stomach pain, excessive flatulence, eructation, or fatigue. Skin symptoms reduced to one lesion along the palmar surface of thumb bilaterally. Patient was instructed to advance to SCD “illegal” foods for two weeks, continue taking digestive enzymes, 2 capsules before meals, SIBO-MMC, 3 capsules in the morning and evening. Patient was introduced to Klaire Lab’s Ther-Biotic Complete probiotic, 1 capsule daily with food, to support reinoculation of commensal bacteria and support gastrointestinal integrity. After two weeks, the patient was advised to begin challenging foods consumed prior to treatment protocol.
Discussion
This case reports on the approach of utilizing botanical medicine to optimally manage and successfully treat hydrogen positive, methane negative SIBO. It further addresses the obligation of extrapolating a patient’s determinants of health in a clinical care setting while incorporating motivational interviewing to support patient adherence to individualized medicine.
We suspect the pathogenesis of the patient’s hydrogen positive SIBO is multifactorial but was likely set in motion from multiple cases of infectious gastroenteritis. Food borne illness is commonly due to bacterial agents such as Campylobacter, Shigella, E. coli, and Salmonella. These bacteria generate cytolethal distending toxin-B (Cdt-B), a toxin that is structurally similar to vinculin, an intestinal protein responsible for small intestinal motility.18,19 After infection, antibodies develop to Cdt-B, but also attack vinculin due to molecular mimicry. The subsequent loss of vinculin from the enteric nervous system causes decreased motility and loss of migrating motor complex (MMC) function.18,19 The MMC normally creates a wave of motility during the fasting state that cleans the small intestine by pushing food and bacteria distally into the large intestine at a rate of approximately one foot every 5 minutes, which is faster than bacterial replication time. Compare this to the large intestine, in which food moves approximately 1 foot every five hours.9 When the MMC is impaired and food, especially fermentable food, becomes static, this allows bacterial proliferation and colonization, generating small intestinal bacterial and/or fungal overgrowth. Long after recovery from gastroenteritis, anti-vinculin antibodies remain in the body, attacking this important protein. The destruction of vinculin can lead to permanent loss of the MMC, which is presumably why so many patients with SIBO suffer from recurrence, even after a successful kill protocol.18,19
The patient’s concussion may have also contributed to or caused impaired gastric acidity through loss of vagal tone. When there is even minimal damage to the CNS, the ANS and enteric nervous system activate and signal inflammatory hormonal release, which negatively impacts vagal tone.13 Impaired vagal motor activity may cause SIBO due to reduced intestinal contractility; impaired motility, defecation, and valve control, which leads to bacterial translocation; and lack of HCl production.13 When a patient is deficient in HCl, the chyme entering the duodenum may not be acidic enough to cause sufficient cholecystokinin release, thus causing less bile and pancreatic enzyme release, including lipase. This causes lack of digestion, especially of fats, and malabsorption occurs.Fats are responsible for energy production and vitamin/mineral repletion; and though it is likely multifactorial, we suspect that fat malabsorption is strongly contributing to the patient’s dry skin condition. Besides fat malabsorption, his skin rash may also have a hereditary component as well as dehydration and inadequate nutrition.11 Other potential etiological factors in this patient’s presentation of SIBO may include ileocecal valve dysfunction and pancreatic insufficiency.
This case was concluded in December 2021 after reversal of symptoms and negative three-hour lactulose breath test. We can conclude through this case study that a naturopathic botanical approach to treating hydrogen-positive SIBO with herbal antibiotics, digestive enzymes, herbal prokinetics, and biofilm-disrupting agents demonstrates overall improvement in symptomatology and quality of life, while restoring gastrointestinal function. We can also conclude that more research is warranted regarding herbal medicine and its effective mechanism of action in targeting and eradicating methane and hydrogen positive small intestinal bacterial overgrowth and other dysbiotic conditions.
Conclusion
This case report presents a cost-effective, successful treatment of a patient with hydrogen-positive, methane negative SIBO and subsequent dermatitis. SIBO is becoming more prevalent in naturopathic primary care due to enhanced understanding of symptomatology, etiology, and pathogenesis. Through utilizing the Genova Diagnostics lactulose breath test, we were able to gain clarity in the patient’s symptomatology and construct an appropriate treatment plan. Our approach encompassed the use of herbal antimicrobials, berberine, oregano and neem, in conjunction with specific carbohydrate low FODMAP dietary modification. This approach has shown equivalent efficacy to conventional pharmaceuticals in research and from a clinical perspective, as showcased in this case study.
Acknowledgements
This case report was prepared according to the CARE guidelines.20
Author Disclosure Statement
Written informed consent was obtained from the patient for publication of this case report. A copy of the written consent is available for review. The authors sincerely thank the patient for his trust in our care, compliance, and willingness to participate in this case report.
References
- Shah A, Talley NJ, Jones M, et al. Small Intestinal Bacterial Overgrowth in Irritable Bowel Syndrome: A Systematic Review and Meta-Analysis of Case-Control Studies. Am J Gastroenterol. 2020;115(2):190-201.
- Pandey, S., Jha, A., and Kaur, V. Aqueous extract of neem leaves in treatment of psoriasis vulgaris. Indian Journal of Dermatol Venereol Leprol 1994;60(2):63-67.
- Irkin, R. and Korukluoglu, M. Growth inhibition of pathogenic bacteria and some yeasts by selected essential oils and survival of L. monocytogenes and C. albicans in apple-carrot juice. Foodborne Pathog Dis. 2009;6(3):387-394.
- Rezaie, A., Pimentel, M., & Rao, S. S. (2016). How to test and treat small intestinal bacterial overgrowth: an evidence-based approach. Current gastroenterology reports, 18(2), 8.
- Barros, L. L., Farias, A. Q., & Rezaie, A. (2019). Gastrointestinal motility and absorptive disorders in patients with inflammatory bowel diseases: Prevalence, diagnosis and treatment. World journal of gastroenterology, 25(31), 4414–4426. https://doi.org/10.3748/wjg.v25.i31.4414
- Levitt, M. D., & Bond Jr, J. H. (1970). Volume, composition, and source of intestinal gas. Gastroenterology, 59(6), 921-929.
- Pimentel, M. (2009). Review of rifaximin as treatment for SIBO and IBS. Expert opinion on investigational drugs, 18(3), 349-358.
- Chedid V. et al (2014). Herbal therapy is equivalent to rifaximin for the treatment of small intestinal bacterial overgrowth. Global Advances in Health and Medicine, 3(3), 16-24.
- Siebecker A. Clinical Experience, SIBO specialty private practice. SIBO Center for Digestive Health at NCNM Clinic, Portland,Or. 2010-present. www.siboinfo.com.
- Pound MW, May DB. Proposed mechanisms and preventative options of Jarisch-Herxheimer reactions. J Clin Pharm Ther. 2005;30(3):291-295.
- Drago, F., Ciccarese, G., Indemini, E., Savarino, V., & Parodi, A. (2018). Psoriasis and small intestine bacterial overgrowth. International journal of dermatology, 57(1), 112-113.
- Ling, Y., et al. (2018). Novel berberine derivatives: Design, synthesis, antimicrobial effects, and molecular docking studies. Chinese journal of natural medicines, 16(10), 774-781.
- Sandberg-Lewis, K. (2021, January 12). Brain injuries and sibo. National University of Natural Medicine. https://nunm.edu/2019/10/brain-injuries-and-sibo/.
- De Martino, L., De, Feo, V, Formisano, C., Mignola, E., and Senatore, F. Chemical composition and antimicrobial activity of the essential oils from three chemotypes of Origanum vulgare L. ssp. hirtum (Link) Ietswaart growing wild in Campania (Southern Italy). Molecules. 2009;14(8):2735-2746.
- Salem, A., & Roland, B. C. (2014). Small intestinal bacterial overgrowth (SIBO). J Gastroint Dig Syst, 4(225), 2.
- Sawka, M. N., Cheuvront, S. N., & Carter, R. (2005). Human water needs. Nutrition reviews, 63(suppl_1), S30-S39.
- Ruscio M. Biofilms- Presentation. 2017 SIBO Symposium, National University of Natural Medicine, June 3, 2016.
- Dukowicz AC, Lacy BE, Levine GM. Small intestinal bacterial overgrowth: a comprehensive review. Gastroenterol Hepatol (N Y). 2007;3(2):112-22.
- Altman L.. Natural Approaches to Small Intestinal Bacterial Overgrowth Introduction to SIBO, Diagnosis, Treatment Lecture. 2020.
- Riley DS, Barber MS, Kienle GS, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017;89:218-235.
BIO

Samantha Davison is completing her Doctorate of Naturopathic Medicine at Bastyr University-California and has further completed her studies with the Institute of Functional Medicine. In 2015 she received her BSc in biology and pre-health sciences at the University of North Dakota, graduating Magna Cum Laude, in addition to playing NCAA Division I women’s soccer. Samantha’s core clinical interests include gastroenterology, women’s health, fertility, oncology and environmental toxicity. She is passionate about root cause medicine while incorporating modern technology with nature cure. Samantha is dedicated to intentionally educating and empowering her patients throughout their health journey to optimum wellness.”

Brad Case, DC, ND, received his Doctor of Chiropractic from the National College of Chiropractic (now NUHS) in 1993, He ran a holistic chiropractic practice in Monterey County, California for eighteen years. In 2007, he was published in the book 101 Great Ways to Improve Your Health. In 2010, he published his own award-winning book, Thugs, Drugs and the War on Bugs. He then retired from practice and began his teaching career. He had his own radio show for a year and then taught anatomy and physiology at the undergrad level before entering into a three-year family practice residency at National University of Health Sciences. While completing his residency, he also acquired his ND degree, graduating Summa Cum Laude and valedictorian of his class.
He taught in the clinical sciences department at NUHS-Florida for two years as part of their Doctor of Chiropractic program. He now teaches naturopathic medicine at Bastyr University-California and is a clinical supervisor at Bastyr University Clinic in San Diego. While he claims no true specialty, GI health, physical medicine, AK/muscle testing, and whole food concentrates are mainstays of his practice life. He’s also a veteran, serving in the Army National Guard for six years, retiring as a staff sergeant.