Hydrotherapy à la Française
The proverbial question kids are asked during their first week back at school is “what did you do this summer?” “Went to the beach,” “Stayed on the lake,” “hiked in the mountains,” “visited relatives,” “traveled to the city,” or “attended sleep-away camp” are the usual answers. My “camping” experience for two weeks was sojourning in Tel Aviv at a hotel with a lovely view of the Mediterranean, beach, and city avenue. (It was just what the Doctor ordered!). I was visiting my 94-year-old Aunt Lucy who has lived in Israel nearly since its founding. My brother, David, and his family joined me for the vacation. For someone who spends the year in the rains of the Pacific Northwest, Tel Aviv provided me with beach therapy and natural vitamin D.
The naturopathic profession has long touted hydrotherapy as an important component in the treatment process. During the late 1800s and early 1900s many of the naturopathic pioneers established clinics offering cold showers, foot baths, wraps, massages and more. US physicians like Benedict Lust learned from ole timers in Europe. While the spas in Europe gained wide-spread renown and popularity, practitioners in the US were more typically loners needing to advertise their services. Lust and other practitioners wrote articles and pamphlets discussing the scientific basis for water treatment. NUNM (formerly the National College of Naturopathic Medicine in Portland, Oregon) has collected an extensive library of the writings of these early naturopaths. Sussana Czeranko, ND, edited a 12-volume collection of these writings entitled The Origins of Naturopathic Medicine, published as the Helvert Collection (available for purchase).
Recently, I saw a posting on the social media site, LinkedIn, by Dr. Mark Hyman, renowned functional medicine MD. He was immersed in a bath filled with ice cubes and water. Hyman’s typical pedantic discussion explaining how nutrition improves one’s health was shockingly replaced with a photograph of himself sitting upright in the tub, all smiles. He didn’t explain how long he was in the icy water, but I imagine it could not have been much more than 60 seconds—just long enough to pose for a photo with an expression of nervous bliss. I know there is value to a cold shower in getting the circulation going and there is an invigorating feeling once one has finished and dried off. However, I think the plunge into the ice water is a little too extreme for my comfort. As far as I know, Hyman hasn’t touted the benefits accrued from this frigid immersion on LinkedIn since the original posting.
In France hydrotherapy is neither cold nor the sole domain of naturopathic physicians. Instead, it is usually warm, sometimes quite warm, and the thermal cure is prescribed by one’s physician. There are 113 official thermal spas in France, and the cost for the water cure as long as you are a French citizen is covered by the state’s social security system. Lauren Collins, a writer for The New Yorker, discusses her experiences with “social thermalism” in the May 30, 2022 issue in an article entitled “Soaking It In.” Just like there is a provincialism with wine and cheese in France, thermal spas also have their own “terroir”; a spa in central France’s Vichy is entirely different from one on the Atlantic, like Roscoff.
As Collins discusses in her article there are two types of hydrotherapy—a sulfurous one and a salty one. The first definitely has the odor of rotten eggs and cabbage soup; the latter is known as thallasotherapy (from thallaso-, Greek, for the sea) using sea water. Thermal spas were originally discovered and used by Gauls and Romans thousands of years earlier. However, it was not until Henry IV in the 17th century officially decreed thermal baths for medical use that thermalism become an institution in France. Napoleon III designed palatial buildings in Vichy making for a very aesthetic version of hydrotherapy. By the late 1800s spas were cropping up throughout France in mountain hamlets and coastal locales affording hydrotherapy treatment for all. Recently the thallasotherapy spas are no longer reimbursed by the French social security meaning all clients must privately pay. Nevertheless, millions come to spas for a three-week session of treatments each year. Moreover, the thermal sulfurous spas remain a mostly government-paid medical hydrotherapy for all who get a physician’s prescription.
Those who have read Georges Simenon’s “Maigret in Vichy” (also a TV series entitled Maigret) may recall the boring and tedious aspects of a Vichy water cure:
They would have sworn that they had been at Vichy for an eternity, while it was only their fifth day. Already, they’d created for themselves a schedule that they followed meticulously, as though it was of importance, and the days were marked by a certain number of rituals, to which they lent themselves with the utmost seriousness.
In fact, the curistes, as they are called, who come for water treatment know that they must diligently participate in their hydrotherapy treatments if they are to succeed in turning around their ills. Carrots and other root vegetables are considered part of the treatment to be consumed daily. At Vichy there are five different waters all at different temperatures ranging from 22 to 43 degrees Centigrade. One is generally prescribed to drink a half liter of a certain water six times daily (more or less). One patron described the water as tasting awful, “super nasty.” When the author, Collins, took a sip, it not only tasted like “rotten eggs” and “cabbage soup” but also it had a chalky sensation, “like she had licked a blackboard.” A hydrotherapy series at Vichy might include “18 mud baths, 18 high pressure underwater showers, 18 pool sessions, 9 water massages, and 9 steam-chair treatments over 3 weeks.” For some curistes, the program also may require sessions of enteroclyse meaning colonic enemas using the Vichy water. For each spa there is a doctor and the curiste is examined by the physician before treatment, then half-way through the three weeks, and at the completion of the program. Most physicians undergo special training and accreditation as a spa doctor.
For the thallasotherapy, Collins visited Roscoff, a region known for its pink, sweet onions that are enjoyed not just in France but in England as well. The favorite treatment at Roscoff is known as the douche a jet, which the director described as a “vigorous jet of water that left one’s legs feeling like they were made of cotton.” Collins’ description of it gives a personal perspective:
Soon I was standing stark naked at the far end of a narrow, gray-tiled room, clutching the side bars of a waist-high metal support. About 10 feet away, the therapist was unfurling a thick hose from a wall mount.
“’Turn to the right,’” she said. “’Ready?’”
I braced myself. The water pressure was intense—almost strong enough to clean a sidewalk. I could taste the salt. The therapist was yelling instructions, but I could hardly hear them over the roar of the spray. She started with my ankles, working methodically up the line: calves, thighs, butt, triceps, shoulders.
“’Lift up your feet,’” she said.
She hosed down my soles. Then my palms. My whole body was being spray painted, and she was determined not to miss a spot.
At the end of the treatment, the therapist had me turn toward her. Here it was: the full-on douche a jet, straight to the gut. I closed my eyes.
When she asked if I’d like a final blast of cold water, I surprised myself by saying ‘yes.’
In the US hydrotherapy is not recognized as a medical treatment. Of course, patients are encouraged to go swimming for exercise, enjoy sauna and steam baths, bathe in a jacuzzi. Unfortunately, going to a spa for hydrotherapy is considered tourism not medical therapy and is not covered by insurance. Still we need to consider hydrotherapy for our patients. It may help the illness, relax the patient, and does no harm.
Jonathan Prousky, ND, MSc, on Physician Burnout
Dr. Jonathan Prousky is the chief medical officer as well as professor at the Canadian College of Naturopathic Medicine. Prousky’s specialty lies in treatment of mental illness combining his knowledge of conventional psychiatry and psychology, naturopathic medicine, as well as orthomolecular medicine. He has been a contributing writer to the Townsend Letter submitting many articles over the past two decades. One of his earliest submissions was awarded the Best in Naturopathic Medicine Townsend Letter award. We are pleased to include his writing substantiating naturopathic and orthomolecular mental health treatment contrary to the psychiatric profession’s disdain for such therapy. Indeed, while skeptics such as the contributors and moderators of Wikipedia have belittled nutritional and natural treatments for mental health, Prousky’s examination of the literature establishes evidence-based medicine for such approaches.
The Greek proverb, “Physician, Heal Thyself,” which also appears in the biblical Old and New Testaments as well as Aeschylus’s Prometheus Bound and in Aesop’s fables behooves the physician to heal oneself before healing others. Of course, contemporary medical ethics according to the AMA stipulate that a physician should not treat oneself or one’s family members, which presents an awful dilemma for the doctor who is burned out. After all, we all should take care that we know how to balance work and life and not overwork to the point of burnout.
Unfortunately, burnout is all too common. According to statistics cited by Prousky between 25-50% of physicians in the US and Canada experience burnout. These numbers are dramatically higher than non-medical workers in both countries. We all talk about how stress contributes to illness, but doctors are no better at managing stress than those in other professions or work activities. Burnout is not just stress but a state of dysfunction impairing a physician’s ability to practice effectively while potentially harming the patient. It is manifested by depression, anxiety, cognitive impairment, and overall work life imbalance. But how does one diagnose and treat burnout?
Prousky reviews allostasis, the ability to adapt to stresses that we experience. We generally describe this as impairment to the HPA axis with diurnal dysfunctioning of cortisol levels. However, Prousky points out that allostasis involves much more than cortisol dysfunctioning. Changes in our neurochemistry especially involving mono-amino acids such as norepinephrine, epinephrine, dopamine, and serotonin transpire during burnout. Brain derived neurotrophic factor (BDNF) is noted in research studies to be substantially lower in the burned-out individual compared to the normal one.
What is the physician to do if he/she is burned out? Lifestyle changes are key. Work responsibilities at office and home need to be reduced and more time must be allotted for relaxation, exercise, nutrition, and sleep. Elimination of toxic exposures both chemical and interpersonal is necessary. Prousky presents the evidence of micronutrient and herbal support. And not just for a few of us, counselling and meditation will be part of the prescription.
Perhaps the most difficult part for the physician is admitting that one is suffering from burnout.
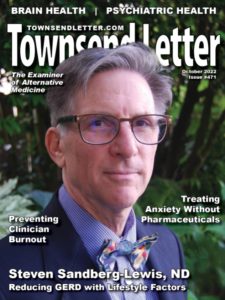
Cover Article: Steven Sandberg-Lewis, ND, on Reflux
In the late 1970s while practicing in Bellevue, Washington a patient consulting with me recommended that I go visit his hometown, Port Townsend, 60 miles and a ferry ride away. After enjoying its local county fair, I became interested in moving to the Victorian town on the Olympic Peninsula. In 1981, Dr. Steven Sandberg-Lewis was looking to spread his wings and put his practice and cottage on the market. I thought that this was a splendid opportunity to do the same and we worked out an agreement for me to give it a trial for one year. After that year the deal was finalized, and I have continued to practice medicine as well as publish the Townsend Letter in Port Townsend.
Meanwhile, Dr. Sandberg-Lewis moved back to Portland where he established a private practice and served as adjunct faculty at NCNM. From 1996-2019 he served as a full-time professor at the National College of Naturopathic Medicine (now NUNM). His specialty at the college was in gastroenterology, establishing in 2010 a center for the study of SIBO. Sandberg-Lewis is the author of Functional Gastroenterology: Assessing and Addressing the Causes of Functional Digestive Disorders.
In this issue we publish an excerpt of Dr. Sandberg-Lewis’s new book: Let’s Be Real About Reflux: Getting to the Heart of Heartburn. He wants us to differentiate between reflux and heartburn—they are not the same thing. For one thing one can have reflux without heartburn (rare) and heartburn without reflux (not so rare). It is reflux that we need to be concerned about. Long standing untreated reflux can lead to Barrett’s as well as cancer of the esophagus.
In a word, one of the most effective ways to reverse GERD is by lessening dietary intake of carbohydrates. Dr. Sandberg-Lewis has a mnemonic, CARBS to keep in mind those carbohydrates most responsible for reflux symptoms. Cola, coffee, and chocolate; alcohol and acidic foods; and refined carbohydrates are among those foods to restrict. He also cautions against eating big meals and snacking.
Sandberg-Lewis’s prescription is a welcome alternative to the prescribing of antacids and proton-pump inhibitors.