By Andrew Wong, MD, FACP,1
Tedra James, MA, MS,1 and
David Hagedorn, PhD, BCN2
Early Detection Conundrum
Physicians are uniquely charged to effectively determine the cause of patient complaints and to do so early in the course of the potential disease to maximize convalescence. This is especially salient for the growing number of patients presenting with memory loss.1 When patients present with hindered mental capacity to perform daily activities, the physician needs a rapid, easy-to-use, low-cost, non-invasive, and sensitive test. Electroencephalography (EEG) using digital analysis and event-related potentials (ERPs) supported by international medical research meet this clinical need for a non-invasive and office-based option for brain function assessment. The added advantage of this functional measure is that it can better guide brain-computer interface therapies that are increasingly showing remarkable safety and efficacy.
Brain Mapping Biomarkers
A hallmark symptom of dementia, affective, and cognitive disorders is memory loss. Because memory loss is common to several conditions, the benefits of tests that aid differential diagnosis are essential. Until recently, most medical providers have relied on self-report or caregiver-report questionnaires and occasionally some effort-based computerized testing to determine a diagnosis. Even when applied optimally, these assessments often fall short in detecting early or less severe disease presentations to include subjective cognitive impairment (SCI). While more complex, the alternative or adjunct use of functional biomarkers recorded with quantitative electroencephalography (qEEG) produces greater sensitivity and more recently improved specificity so that doctors can gauge condition severity and target functional neuro-biological networks from which the memory dysfunctions supervene.
The brain’s capacity for normal productive function relies heavily on a complex array of interconnected networks that facilitate communication within and across brain structures. Therefore, to understand and influence brain function, particularly memory, there is a need to isolate key functional biomarkers. Four major electrophysiology measurement categories relevant to memory function are: 1) thalamic generated alpha frequency (posterior peak alpha frequency); 2) slow-wave frequency band dominance by brain region (i.e., delta, theta); 3) the P300b component of event-related potentials; and 4) brain structure (Brodmann Areas) scoring against a gender- and age-normed reference group.
In recent years, additional EEG devices from the US and abroad have reached the general medicine market. Some devices new to the market still lack attention to aseptic techniques (e.g., helmet designs, non-removable scalp sensors). Other instruments are not medical-grade, only utilize a limited number of scalp EEG sensor locations, or do not correlate with the international standards of scalp electrode placement. There are advantages and disadvantages to each design. Still, some critical features to look for in utilizing qEEG for patient care include finding companies with a proven track record in the medical market that are ISO and FDA-compliant, are easy to use, and have excellent clinical support and protocols. The eVox System® (Evoke Neuroscience, Inc.) is one such example used by the US Military across all service branches because of its all-inclusive electrophysiology assessment features, automated data analysis, technical support, and integrated HRV and EEG biofeedback. With modern digital analysis and machine learning, memory dysfunction biomarkers are faster and easier to obtain at a low cost, translating into a lower patient burden during a general medical care appointment.2
Peak Alpha Frequency
The alpha frequency band (8 – 12Hz), the most dominant EEG frequency found in the brain, is a good measure of information processing capacity. One might even describe this function as the most salient feature of memory.3 Peak alpha frequency detected from the parietal and occipital scalp locations reflects thalamic functioning. Low posterior peak alpha frequencies (< 8Hz) are correlated with cognitive disturbances and dementia.4,5 On the other hand, higher alpha2 power—often around 11-12 Hz—is associated with central nervous system over-arousal conditions.6 Beyond the well-established relationship between low posterior dominant alpha rhythm peak (below 8Hz) and cognitive impairment are several alpha ratios (e.g., alpha3/alpha2) or alpha to even slower frequency (theta) ratios. These different EEG frequency band power ratios appear to offer further discrimination regarding memory loss types and disease course prediction.7-9
P300b
Memory functions and several cognitive processes within the brain can be measured using event-related potentials (ERPs).10,11 With ERPs, one can quantify time-locked neuronal responses following presented stimuli. The time delay or latency between stimulus onset and a patient’s physical response reflects processing speed. The ERP component’s amplitude reflects neuronal recruitment and subsequent activation. With good reliability, longer or delayed latency measures and low amplitudes are associated with aging and dementia conditions and indicate cortical and subcortical dysfunctions.12,13 Fundamental memory elements involve the degree of attention to a stimulus and the subsequent encoding of information for storage and retrieval. Two ERP components useful to measure these cognitive processes are P300a and P300b, respectively.14 The P300a component is dopamine-mediated and reflects frontal working memory functions or dysfunctions. The P300b component, however, is mediated by norepinephrine and is generated in the medial temporal lobe. These two components are helpful in differential diagnosis, EEG biofeedback, other neuromodulation therapies, and tracking the disease course and effects of treatment.
Brodmann Areas and LORETA Imaging
Brodmann Areas (BA) represent regions of the cortex cyto-architecturally organized into functional locations and are a well-respected and widely referenced system for brain mapping. The ability of qEEG to derive statistical scores (i.e., Z-score) on the BAs throughout the patient’s brain informs the clinician of deviation from normalcy and clarifies longitudinal treatment effects. When used in parallel with imaging libraries, scalp surface EEG low-resolution brain electromagnetic tomography (LORETA, sLORETA) permits added insight to differential diagnosis and treatment effects.15-17 For example, Alzheimer’s disease presents with EEG power abnormalities more globally than frontotemporal dementia; the ability to source localize to specific brain structures, using BAs, aids the clinician in cross-correlating known brain structures that are hallmarks of particular diseases. EEG and source localization sensitivity with sLORETA allow for a helpful assessment measure when considering memory impairment etiology, personalized treatment interventions, and treatment response patterns.
Office-Based Solutions
Medical office-based electroencephalography and event-related potential recording used with analysis equipment are recent advancements in general practice medicine. This patient access improvement emerged from military medicine where there was a need during the Middle East conflict to less invasively and quickly evaluate brain injury and trauma-related psychopathology. Physicians across various specialties began using this digital analysis hardware and software pioneered with the military. This first-line brain assessment approach has been easier on patients, appears to reduce imaging costs, and allows lower-income or underinsured patients greater access to functional brain-informed differential diagnosis and treatment decisions.
The FDA-registered medical equipment such as the eVox System® incorporates a portable and automated 24-channel electroencephalography (EEG) amplifier for standard 19-channel EEG and event related potentials (ERP), and 3-channel electrocardiography (ECG). EEG and ERP digital analysis with artificial intelligence algorithms have recently been sensitive and specific aids to physicians seeking to understand and track early onset dementia subtypes. Publications recently in-press and those soon to print highlight that EEG can reliably and quickly identify the major types of cognitive impairment, i.e. subjective cognitive impairment (SCI), mild cognitive impairment (MCI), and Alzheimer’s disease (AD).
Here we discuss the evaluation of patients’ cognitive function using the eVox System® in a primary care setting. Of note, this device is a medical grade EEG amplifier with integrated software that permits user selection of indicated tests. It also integrates heart rate variability and EEG biofeedback intervention should the assessment and clinical indications support this added therapy. Depending on their symptoms, patients in our functional medicine practice are often recommended to complete the EEG/ERP and calculated qEEG once a year. Patients receive a summary of their results and review the comprehensive report and receive treatment recommendations with their physician.
Case 1 – Early Dementia
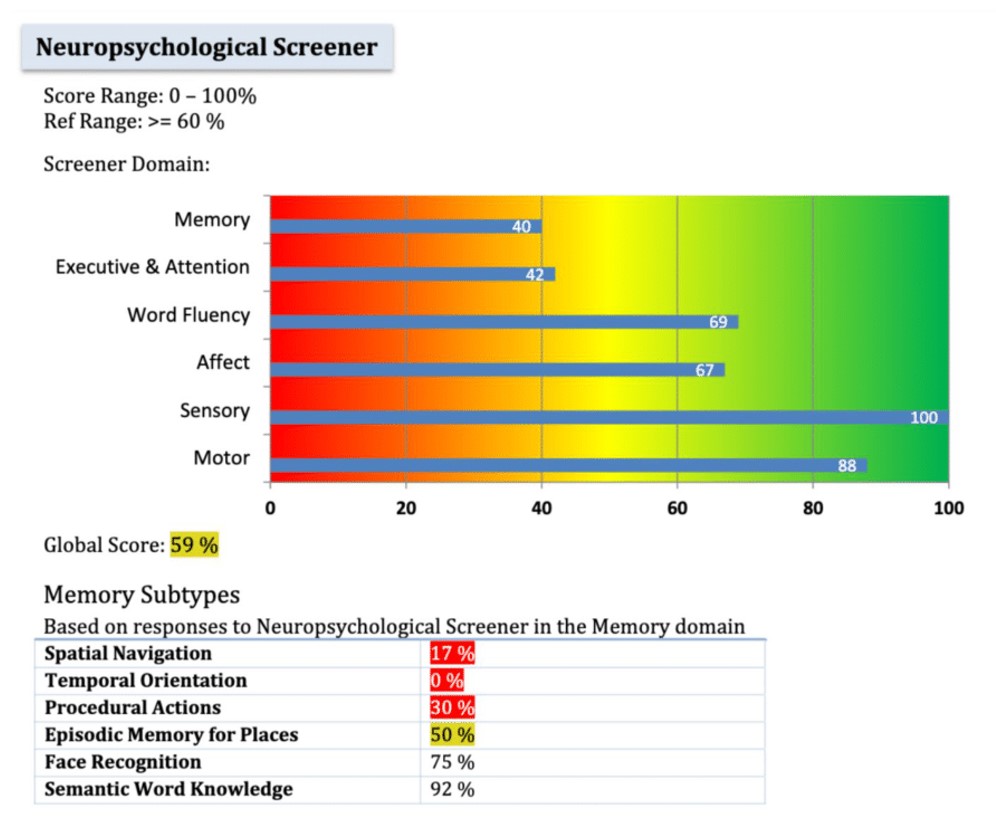
symptoms, reporting low memory, executive function,
and attention day-to-day (Case 1).
An 83-year-old patient presented to the clinic recently with a diagnosis of dementia after first receiving a diagnosis of mild cognitive impairment seven years prior. His medical history is also significant for sleep apnea and hypertension. The patient’s EEG/ERP measures indeed has several markers of dementia including a peak alpha frequency of 7.60 Hz, high alpha3/alpha2 power ratio of 1.01, excess delta and theta wave activity in the front of the brain, and low self-reported memory and executive and attention functioning (Figure 1). Treatments for this patient will focus heavily on functional nutrition where he receives guidance on the Bredesen Ketoflex diet, adding sources of nitric oxide to encourage blood flow, and focusing on anti-inflammatory foods. The EEG/ERP measures will help us monitor the progression of his symptoms and brain function.
Case 2 – Mild Cognitive Impairment
At a routine appointment, a 66-year-old male reported forgetfulness and disorganization such as missing his highway exit on his established route. He has a family history of Alzheimer’s and personal history of heart disease, hypertension, and metabolic syndrome. His qEEG report showed a peak alpha frequency (PAF) of 7.30 Hz, theta activity significantly above the population norms, and a P300b component with no defined peak (see Figure 2). The low PAF and indiscernible P300b, as mentioned above, are associated with diminished information processing abilities. The patient was referred to a neurologist for further evaluation. Here, he was diagnosed with memory impairment and with possible underlying cause of vascular inflammation, metabolic encephalopathy, and CNS hypo-perfusion. He was prescribed Ritalin and modafanil to help with his symptoms of hyper-somnolence and memory impairment. With our clinic, the patient continued acupuncture to manage inflammation-related pain and began working with our functional nutritionist to adopt lifestyle changes to decrease inflammation. He was recommended brain health supplements such as a high-quality MVI, vitamin D3, omega-3 fatty acids, CoQ10, and was encouraged to improve sleep quality and hygiene with an earlier bedtime and new mattress that decreased snoring, thus increasing oxygen supply to the brain. Other lifestyle interventions included daily walking to reduce inflammation and improve circulation to the brain.
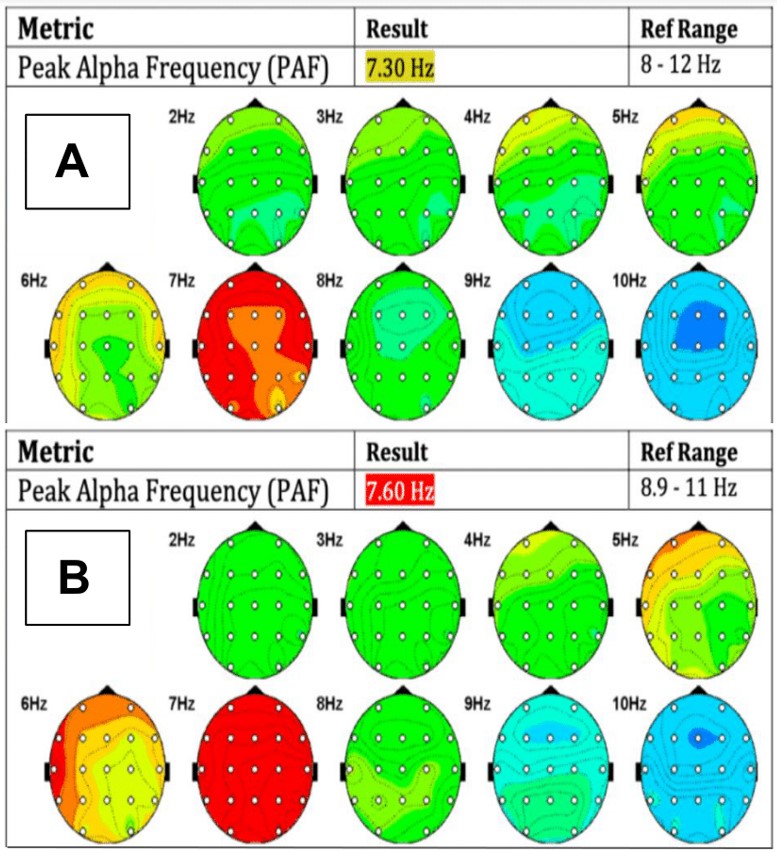
eyes-closed headmaps and peak alpha frequency before
(Panel A) and after (Panel B) two years of functional
medicine treatment (Case 2).
After two years of simple-yet-effective lifestyle interventions, the patient’s EEG/ERP measures showed both objective and subjective improvements in function. His PAF increased to 7.60 Hz from 7.30 Hz, demonstrating increased information processing capacity (Figure 2). Additionally, the power of his alpha3/alpha2 ratio in the occipital region decreased slightly from 0.97 to 0.95; as higher ratios are correlated with cortical atrophy of the inferior parietal lobule and worsened cognitive symptoms, the conservation of this measure is promising.8 In addition to these neural changes, the patient’s self-reported daily executive function and attention symptoms improved from 4% to 38% capacity as measured by the neuropsychological screener incorporated in the procedure. To address the patient’s remaining struggles with word recall, we are working on improving sleep quality with supplementation and further supporting brain health through addressing hormone balance. We hope to continue to see improvements and prevent the progression of his mild cognitive impairment.
Case 3 – Early Dementia
A 59-year-old female patient presented to the clinic with a diagnosis of early onset Alzheimer’s that was confirmed by a glucose PET scan. She had to leave Post-It™ notes around her entire house because of her extremely compromised short-term working memory. Her history was significant for Sjogren’s, POTS, chronic kidney disease, and Hashimoto’s. The results of her first EEG/ERP measures contained a delayed P300b component, excess power relative to the population at 7-9 Hz at rest, and a borderline low peak alpha frequency of 9.20 Hz (Figure 3). Her treatment regimen included frequent neurocognitive screening as well as the addition of thyroid hormone replacement, low-dose naltrexone (LDN), and nitric oxide-boosting supplementation. She continued management of her POTS and chronic kidney disease through her other specialists.
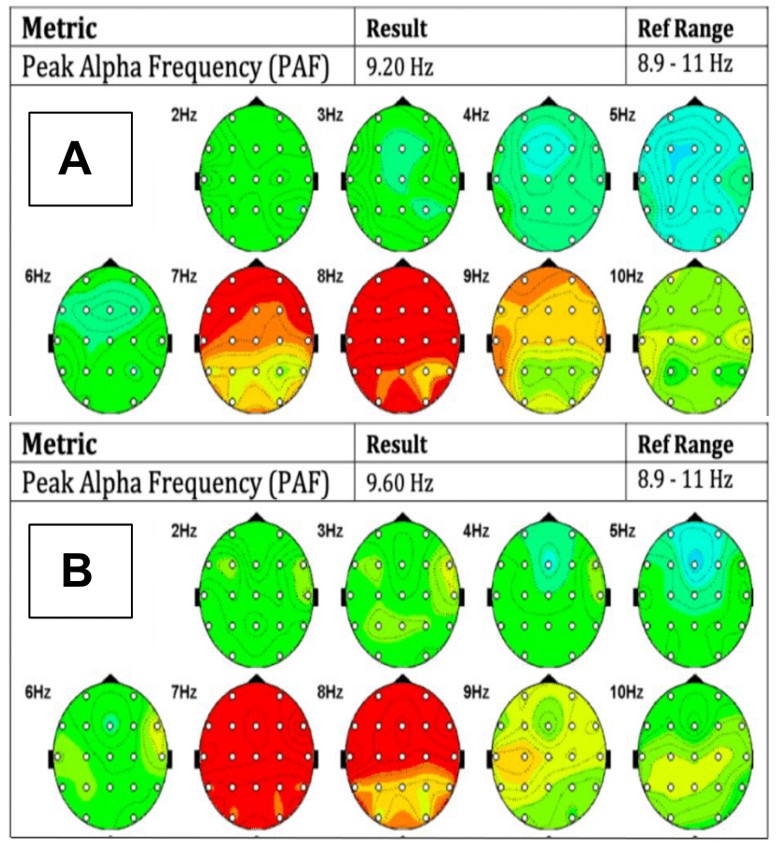
eyes-closed headmaps and peak alpha frequency
before (Panel A) and after (Panel B) one year
of functional medicine treatment (Case 2).
Functional nutrition treatment included the Bredesen Ketoflex protocol, healing gut inflammation, and improving digestion.
After 1 year of treatment, she reported improved memory. This improvement was supported by neural changes in her quantitative EEG. Significantly, her peak alpha frequency increased from 9.20 Hz to 9.60 Hz (Figure 3), suggesting improved capacity to process and retain information. Additionally, the latency of the P300b component decreased slightly from 636ms to approximately 600ms with a slight increase in power, likewise suggesting improved working memory. The patient was able to get rid of using Post-It™ notes around her house and reported less brain fog and better executive function and working memory. We continue to monitor this patient’s symptoms closely and expect to see slow but steady improvement.
EEG biofeedback
In addition to the use of electrophysiology measures for early detection and tracking progress, these tools can guide individualized brain-computer interface (BCI) treatment interventions (EEG biofeedback or neurofeedback), both for office-based or home-based therapy (Versus®). The ability to supplement cognitive rehabilitation using EEG biofeedback avoids additional drug interaction effects. In addition, the home-use devices permit daily personal training that reduces medical costs and gives patients more autonomy over their health.
EEG biofeedback has had a history of clinical efficacy since the early 1970s. This intervention has several forms or methods of application, including real-time referenced normative database Z-score training, EEG frequency band amplitude modulation, and research-level complex fMRI guided neurofeedback.18,19 International peer-reviewed research literature posits medium to large effect sizes, thereby making EEG biofeedback a safe and viable treatment modality in the multimodal medical management of conditions such as attention-deficit disorder,11,20-24 pain,25 dementia/memory loss,19,26-35 and others.36 With the added benefits of having no relative harm compared to other more common standard treatments, there is good reason for physicians to integrate EEG biofeedback in treating brain-related conditions.
Conclusions
The Alzheimer’s Association 2020 facts and figures report found that 87% of primary care physicians expect to see an increase in dementia cases. This clinical population of adults with memory loss paired with the lackluster standard of care treatment results necessitates a more physiologically functional set of measures. Electrophysiology measures should aid in the determination of dementia subtype and severity and guide alternative medication and non-medication treatments. With growing trends toward personalized medical treatments enhanced by machine learning advances,37,38 the EEG/qEEG and ERPs have become an ever more helpful office-based brain function analysis method. It is easy to use and has a relatively low cost, enough to be used routinely and frequently to track patient progress. Physicians appreciate the eVox System® as an office-based tool yielding sensitive measures to help patients see the value of treatment compliance, with additional biomarker information to support differential diagnosis and a more individualized EEG biofeedback intervention option. These advances in applied medical neuroscience, if brought out on a large-scale to the population and combined with a root-cause medicine approach, will be instrumental in preventing or even reversing the effects of cognitive impairment on the population.
Make sure to get ALL our fascinating articles – Subscribe Today!