By Erik Peper, PhD,[1] and Richard Harvey, PhD
Abstract
Most likely, COVID-19 disease will become endemic because the SARS-CoV-2 virus will continuously mutate. To reduce future infections, the focus of interventions should 1) reduce virus exposure, 2) vaccinate to activate the immune system, and 3) enhance the innate immune system competence. Public health policies need to focus on intervention strategies and positive health behaviors that optimize the immune system capacity to respond since comorbidity such as obesity, diabetes, cardiovascular disease and other chronic diseases are the significant risk factors that contribute to COVID-19 deaths. The focus needs to be on incorporating behavioral medicine prescriptions that support a healthy lifestyle into treatment plans, such as increasing vitamin D, eating organic locally grown vegetable and fruits foods, exercise and stress management.
The number of hospitalizations and deaths from COVID-19 are decreasing as more people are being vaccinated. At the same time, herd immunity will depend on how vaccinated and unvaccinated people interact with one another. Close-proximity, especially indoor interactions, increases the likelihood of transmission of coronavirus for unvaccinated individuals. During the summer months, people tend to congregate outdoors, which reduces viral transmission and also increases vitamin D production, which supports the immune system (Holick, 2021).
Most likely, COVID-19 disease will become endemic because the SARS-CoV-2 virus will continue to mutate. Already Pfizer CEO Albert Bourla stated on April 15, 2021 that people will “likely” need a third dose of a Covid-19 vaccine within 12 months of getting fully vaccinated. Although, at this moment the vaccines are effective against several variants, we need to be ready for the next COVID XX outbreak.
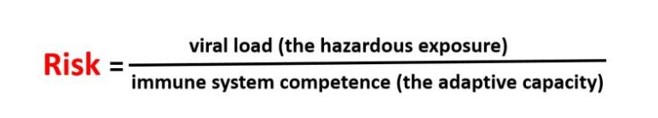
To reduce future infections, the focus of interventions should 1) reduce virus exposure, 2) vaccinate to activate the immune system, and 3) enhance the innate immune system competence. The risk of illness may relate to virus density exposure and depend upon the individual’s immune competence (Gandhi & Rutherford, 2020; Mukherjee, 2020) which can be expressed in the following equation.
Reduce Viral Load (Hazardous Exposure)
Without exposure to the virus and its many variants, the risk is zero which is impossible to achieve in democratic societies. People do not live in isolated bubbles but in an interconnected world and the virus does not respect borders or nationalities. Therefore, public health measures need to focus upon strategies that reduce virus exposure by encouraging or mandating wearing masks, keeping social distance, limiting social contact, and increasing fresh air circulation.
Wearing masks reduces the spread of the virus since people may shed viruses one or two days before experiencing symptoms (Lewis et al., 2021). When a person exhales through the mask, a good fitting N95 mask will filter out most of the virus and thereby reduce the spread of the virus during exhalation. To protect oneself from inhaling the virus, the mask needs be totally sealed around the face with the appropriate filters. Systematic observations suggest that many masks such as bandanas or surgical masks do not filter out the virus (Fisher et al., 2020).
Fresh air circulation reduces the virus exposure and is more important than the arbitrary 6 feet separation (CDC, May 13, 2021). If separated by 6 feet in an enclosed space, the viral particles in the air will rapidly increase even when the separation is 10 feet or more. On the other hand, if there is sufficient fresh air circulation, even three feet of separation would not be a problem. The spatial guidelines need to be based upon air flow and not on the distance of separation as illustrated in the outstanding graphical modeling schools by Nick Bartzokas et al. (February 26, 2021) in the New York Times article, Why opening windows is a key to reopening schools.
The public health recommendations of sheltering-in-place to prevent exposure or spreading the virus may also result in social isolation. Thus, shelter-in-place policies have resulted in compromising physical health such as weight gain (e.g. average increase of more than 7lb in weight in America according to Lin et al., 2021), reduced physical activity and exercise levels (Flanagan et al., 2021) and increased anxiety and depression (e.g. a three to four fold increase in the self-report of anxiety or depression according to Abbott, 2021). Increases in weight, depression and anxiety symptoms tend to decrease immune competence (Leonard, 2010). In addition, the stay at home recommendations especially in the winter time meant that individuals are less exposed to sunlight which results in lower vitamin D levels which is correlated with increased COVID-19 morbidity (Seheult, 2020).
Increase Immune Competence
Vaccination is the primary public health recommendation to prevent the spread and severity of COVID-19. Through vaccination, the body increases its adaptive capacity and becomes primed to respond very rapidly to virus exposure. Unfortunately, as Pfizer Chief Executive Albert Bourla states, there is “a high possibility” that emerging variants may eventually render the company’s vaccine ineffective (Steenhuysen, 2021).Thus, it is even more important to explore strategies to enhance immune competence independent of the vaccine.
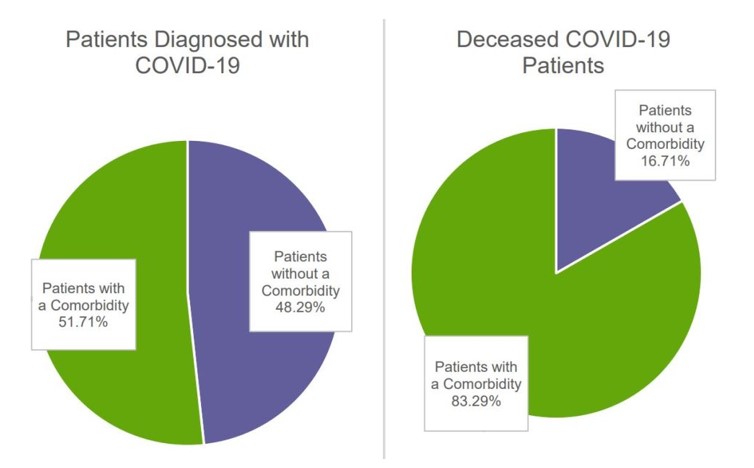
among all patients diagnosed with COVID-19 (left) and all deceased
COVID-19 patients (right) April-August 2020. Reproduced by
permission from: https://www.ajmc.com/view/contributor-links-
between-covid-19-comorbidities-mortality-detailed-in-fair-health-study
Public health policies need to focus on intervention strategies and positive health behaviors that optimize the immune system capacity to respond. The research data has been clear that COVID -19 is more dangerous for those whose immune systems are compromised and have comorbidities such as diabetes and cardiovascular disease, regardless of age.
Comorbidity and being older are the significant risk factors that contribute to COVID-19 deaths. For example, in evaluating all patients in the Fair Health National Private Insurance Claims (FH NPIC’s) longitudinal dataset, researchers identified 467,773 patients diagnosed with COVID-19 from April 1, 2020, through August 31, 2020. The severity of the illness and death from COVID-19 depended on whether the person had other co-morbidities first as shown above, in Figure 1.
Each person who died had about 2 or 3 types of pre-existing co-morbidities such as cardiovascular disease, hypertension, diabetes, obesity, congestive heart failure, chronic kidney disease, respiratory disease and cancer (Ssentongo et al., 2020; Gold et al., 2020). The greater the frequency of comorbidities the greater the risk of death, as shown in Figure 2.
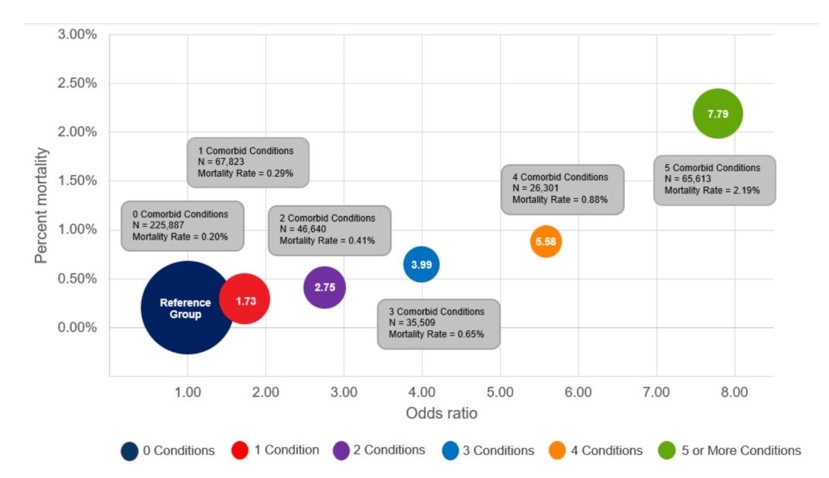
significantly as a patient’s number of comorbidities increased. Compared
to patients with no comorbidities. Reproduced by permission from https://s3.amazonaws.com/media2.fairhealth.org/whitepaper/asset/
Risk%20Factors%20for%20COVID-19%20Mortality%20among%20Privately
%20Insured%20Patients%20-%20A%20Claims%20Data%20Analysis%20-%20A%20FAIR%20Health%20White%20Paper.pdf
Although the risk of serious illness and death is low for young people, the presence of comorbidity increases the risk. Kompaniyets et al. (2021) reported that for patients under 18 years with severe COVID-19 illness who required ICU admission, mechanical ventilation, or died most had underlying medical conditions such as asthma, neurodevelopmental disorders, obesity, essential hypertension or complex chronic diseases such as malignant neoplasms or multiple chronic conditions.
August 2020. Reproduced by permission from: https://s3.amazonaws.
com/media2.fairhealth.org/whitepaper/asset/Risk%20Factors%20for
%20COVID-19%20Mortality%20among%20Privately%20Insured
%20Patients%20-%20A%20Claims%20Data%20Analysis
%20-%20A%20FAIR%20Health%20White%20Paper.pdf
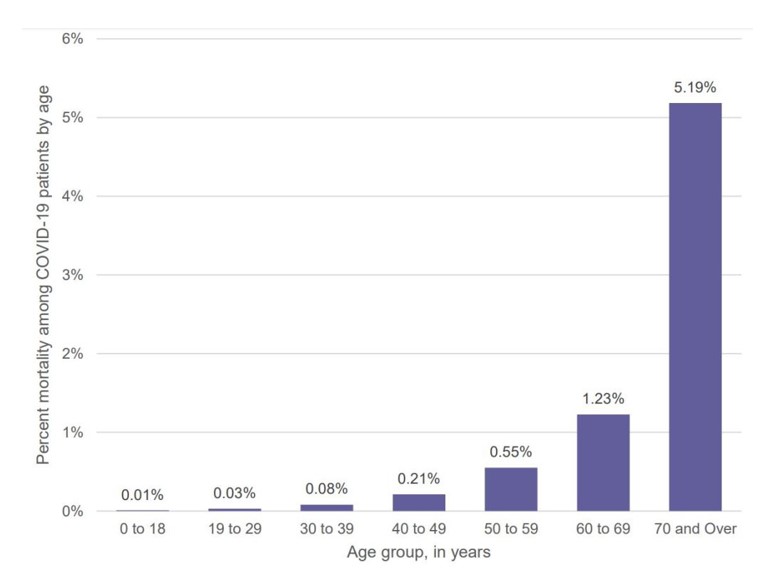
Consistent with earlier findings, the Fair Health National Private Insurance Claims (FH NPIC’s) longitudinal dataset also showed that the COVID-19 mortality rate rose sharply with age as shown in Figure 3.
Optimize Antibody Response from Vaccinations
Assuming that the immune system reacts similarly to other vaccinations, higher antibody response is evoked when the vaccine is given in the morning versus the afternoon or after exercise (Long et al., 2016; Long et al., 2012). In addition, the immune response may be attenuated if the person suppresses the body’s natural immune response–the flulike symptoms which may occur after the vaccination–with Acetaminophen (Tylenol (Graham et al, 1990).
Support the Immune System with a Healthy Lifestyle
Support the immune system by implementing a lifestyle that reduces the probability of developing comorbidities. This means reducing risk factors such as vaping, smoking, immobility and highly processed foods. For example, young people who vape experience a fivefold increase to become seriously sick with COVID-19 (Gaiha, Cheng, & Halpern-Felsher, 2020); similarly, cigarette smoking increases the risk of COVID morbidity and mortality (Haddad, Malhab, & Sacre, 2021).
There are many factors that have contributed to the epidemic of obesity, diabetes, cardiovascular disease and other chronic diseases. In many cases, the environment and lifestyle factors (lack of exercise, excessive intake of highly processed foods, environmental pollution, social isolation, stress, etc.) significantly contribute to the initiation and development of comorbidities. Genetics also is a factor; however, the generic’s risk factor may not be triggered if there are no environmental/behavioral exposures. Phrasing it as colloquially, Genetics loads the gun, environment and behavior pulls the trigger.
Reducing harmful lifestyle behaviors and environment is not simply an individual’s responsibility but a corporate and governmental responsibility. At present, harmful lifestyles choices are actively supported by corporate and government policies that choose higher profits over health. For example, highly processed foods made from corn, wheat, soybeans, rice are grown by farmers with US government farm subsidies. Thus, many people especially of lower economic status live in food deserts where healthy non-processed organic fruits and vegetable foods are less available and more expensive (Darmon & Drewnowski, 2008; Michels, Vynckier, Moreno, L.A. et al. 2018; CDC, 2021). In the CDC National Health and Nutrition Examination Survey that analyzed the diet of 10,308 adults, researchers Siegel et al. (2016) found that “Higher consumption of calories from subsidized food commodities was associated with a greater probability of some cardiometabolic risks” such as higher levels of obesity and unhealthy blood glucose levels (which raises the risk of Type 2 diabetes).
Immune competence is also affected by many other factors such as exercise, stress, shift work, social isolation, and reduced micronutrients and Vitamin D (Zimmermann & Curtis, 2019). Even being sedentary increases the risk of dying from COVID as reported by the Kaiser Permanente Southern California study of 50,000 people who developed COVID (Sallis et al., 2021).
People who exercised 10 minutes or less each week were hospitalized twice as likely and died 2.5 times more than people who exercised 150 minutes a week (Sallis et al., 2021). Although exercise tends to enhance immune competence (da Silveira et al, 2020), it is highly likely that exercise is a surrogate marker for other co-morbidities such as obesity and heart disease as well as aging. At the same time sheltering–in-place along with the increase in digital media has significantly reduced physical activity.
The Importance of Vitamin D
Low levels of vitamin D is correlated with poorer prognosis for patients with COVID-19 (Munshi et al., 2021). Kaufman et al. (2020) reported that the positivity rate correlated inversely with vitamin D levels as shown in figure 4.
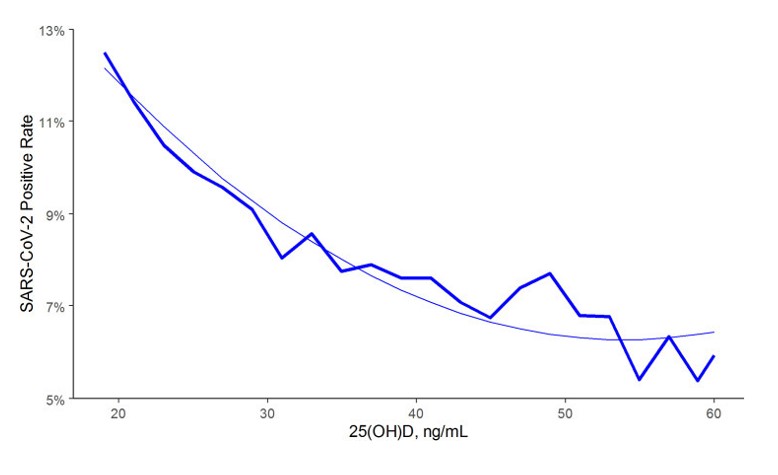
levels in the total population. From: Kaufman, H.W., Niles, J.K., Kroll,
M.H., Bi, C., Holick, M.F. (2020). SARS-CoV-2 positivity rates associated
with circulating 25-hydroxyvitamin D levels. PLoS One.
15(9):e0239252. https://doi.org/10.1371/journal.pone.0239252
Vitamin D is a modulator for the immune system (Baeke, Takiishi, Korf, Gysemans, & Mathieu, 2010). There is an inverse correlation of all-cause, cardiovascular, cancer, and respiratory disease mortality with hydroxyvitamin D concentrations in a large cohort study (Schöttker et al., 2013). For a superb discussion about how much vitamin D is needed, see the YouTube presentation, The D-Lightfully Controversial Vitamin D: Health Benefits from Birth until Death, by Dr. Michael F. Holick, Ph.D., M.D. from the University Medical Center Boston (Holick, 2021).
Low vitamin D levels may partially explain why in the winter there is an increase in influenza. During winter time, people have reduced sunlight exposure so that their skin does not produce enough vitamin D. Lower levels of vitamin D may be a cofactor in the increased rates of COVID among people of color and older people. The darker the skin, the more sunlight the person needs to produce Vitamin D and as people become older their skin is less efficient in producing vitamin D from sun exposure (Harris, 2006; Gallagher, 2013). Vitamin D also moderates macrophages by regulating the release, and the over-release of inflammatory factors in the lungs (Khan et al., 2021). Vitamin D may also be a factor in preventing and possible treatment of the coronavirus (SARS CoV 2) as described by Professor Roger Seheult, MD, UC Riverside School of Medicine in the YouTube presentation, Vitamin D and COVID 19: The Evidence for Prevention and Treatment of Coronavirus (SARS CoV 2) (Seheult, 2020).
What Can Be Done NOW to Enhance Immune Competence?
We need to recognize that once the COVID-19 pandemic has passed, it does not mean it is over. It is only a reminder that a new COVID-19 variant or another new virus will emerge in the future. Thus, the government public health policies need to focus on promoting health over profits and aim at strategies to prevent the development of chronic illnesses that affect immune competence.
One take away message is to incorporate behavioral medicine prescriptions supporting a healthy lifestyle into treatment plans, such as prescribing a walk in the sun to increase vitamin D production and develop dietary habits of eating organic locally grown vegetable and fruits foods. Even just reducing the refined sugar content in foods and drinks is challenging although it may significantly reduce incidence and prevalence of obesity and diabetes (World Health Organization, 2017. The benefits of such an approach has been clearly demonstrated by the Pennsylvania-based Geisinger Health System’s Fresh Food Farmacy. This program for food-insecure people with Type 2 diabetes and their families provides enough fresh fruits and vegetables, whole grains, and lean proteins for two healthy meals a day five days a week. After one year there was a 40 percent decrease in the risk of death or serious complications and an 80 percent drop in medical costs per year (Brody, 2020).
The simple trope of this article ‘eat well, exercise and get good rest’ and increase your immune competence concludes with some simple reminders.
- Increase availability of organic foods since they do not contain pesticides such as glyphosate residue that reduce immune competence.
- Increase vegetable and fruits and reduce highly processed foods, simple carbohydrates and sugars.
- Decrease sitting and increase movement and exercise
- Increase sun exposure without getting sunburns
- Master stress management
- Increase social support
For additional information see: https://peperperspective.com/2020/04/04/can-you-reduce-the-risk-of-coronavirus-exposure-and-optimize-your-immune-system/
[1] Correspondence should be addressed to:
Erik Peper, Ph.D., Institute for Holistic Healing Studies/Department of Recreation, Parks, Tourism and Holistic Health, San Francisco State University, 1600 Holloway Avenue, San Francisco, CA 94132 COVID-19 mailing address: 2236 Derby Street, Berkeley, CA 94705 Email: epeper@sfsu.edu web: www.biofeedbackhealth.org blog: www.peperperspective.com