By Michelle Perro, MD
Through the years, I’ve observed that certain children seem to be tick magnets. An entire family will be out for a hike, but just one of the kids comes home with a tick either behind the ear, embedded in the axilla or along the hairline (ticks’ favorite hiding spots in little kids. Ticks prefer the arms and legs in bigger children.) Interestingly, tick destinations on the body can also vary depending on the species of the tick. The State of Connecticut published the following graph to show where ticks generally gravitate:1
A surprising number of people experience subsequent reinfections with tick-borne infections.2 Upon performing a literature search, studies are sparse to non-existent on how best to manage bites in patients with preexisting infection, especially for children. It is clear that previous infection does not fully protect those with a potential re-infection. What’s also clear is that the management of this common issue has demonstrated the greatest divergence in treatment protocols between allopathic and integrative medicine.
Ticks Targeting Sophia
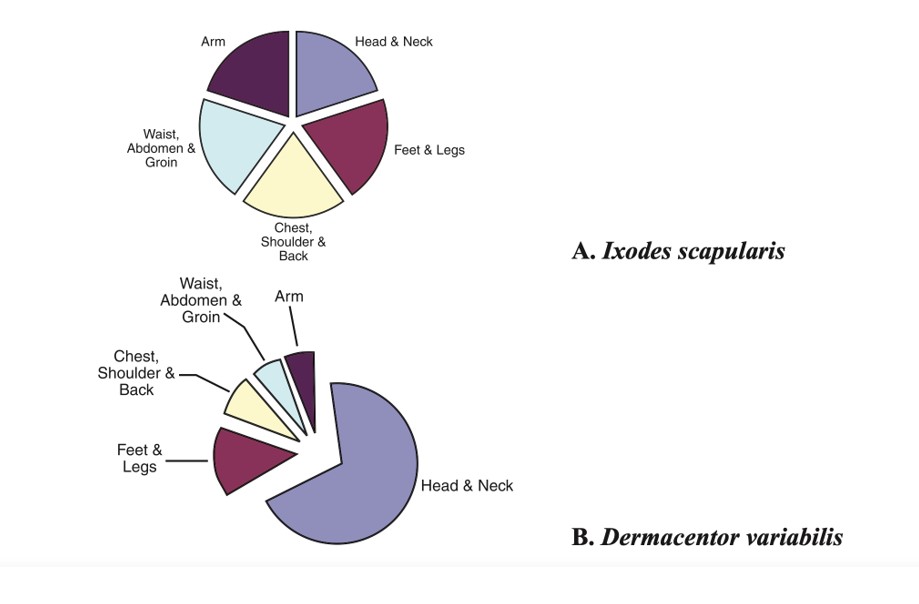
variabilis (B) submitted to The Connecticut Agricultural
Experiment Station recovered from various regions of
the body.
I received a frantic text from a distant relative regarding their 16-year-old daughter who just got a new tick bite while out hiking. The tick was carefully removed and intact. Sophia developed an immediate circular rash around the bite site, which could have been consistent with erythema migrans, one of the most common manifestation of Borrelia infection.3 Her situation was complicated by the fact that she had just developed symptoms of COVID-19, confirmed via a positive molecular antigen test. She reported feeling achy, tired, coughing and nasal congestion, and complained of a severe headache. She couldn’t be sure if what she was experiencing was secondary to COVID-19 or her underlying Lyme disease/co-infections (Epstein Barr Virus and Bartonella). Gone are the days of an “easy” patient or relative!
I am an avid supporter of trying to maintain the integrity of the tick and sending it for evaluation when feasible. A live tick can be placed in a container or plastic bag with a blade of grass and not taped or mounted. I use Tick Report (https://www.tickreport.com) for a tick analysis. Their recommendation is to avoid alcohol or preservative, but if already applied, they report that it doesn’t appear to change the outcome.
Tick Report tests for multiple pathogens at an affordable price. Additionally, an extensive surveillance database can be accessed showing the statistics and distribution in age, tick bite site, genus, tick host, stage of tick, and percentage of positivity by zip code. Fortunately, the percentage of infected ticks where Sophia was bitten was extremely low and subsequently lowered everyone’s anxiety until the report was completed. Good news for Sophia; her tick was clean.
End of Story?
It took five days to get Sophia’s report back. The question is with her history and symptoms, should she be covered with antibiotics for a potential infection while awaiting the results of her tick test? As a seasoned practitioner, this is where experience and “anecdotes” come into play due to the fact that data is sparse or lacking, especially in the patient with preexisting Lyme disease. Even when antibiotics are promptly administered after a tick bite, there is a treatment failure rate of 15-20%. Antibiotics or not? Consider the fact that mainstream physicians will think nothing of placing a teen with acne on antibiotics for months! If a tick-borne infection is missed, the child could be facing life-long devastating health consequences.
Because Sophia had the complicating factors of chronic Lyme disease/co-infections/COVID-19 infection simultaneously, I had quickly decided to treat her. There are herbal and pharmaceutical options, especially in a patient who has already received many of these antibiotics. Because Sophia preferred herbal treatments in general, this was the route we chose. The choice is often decided by what is available and what the patient has had success with in the past. Sophia had easy access to Biocidin®, which is an herbal formulation I’ve used successfully in tick-borne disease infection management. Biocidin® contains bilberry extract {25 percent anthocyanosides}, noni, milk thistle, echinacea (purpurea and angustifolia), goldenseal, shiitake, white willow (bark), garlic, grapeseed extract (minimum 90 percent polyphenols), black walnut (hull and leaf), raspberry, fumitory, gentian, tea tree oil, galbanum oil, lavender oil (plant and flower), and oregano oil (plant and flower). Of interest, a study from Finland in 2018 reported that Biocidin® demonstrated strong antimicrobial action against Borrelia in vitro.4 The liposomal formulation is preferable but wasn’t what the patient had on hand.
If a patient prefers a pharmaceutical route, doxycycline is my first choice since it can also cover other pathogens in addition to Borrelia, such as Anaplasma, Ehrlichia, Babesia, Bartonella and Rocky Mountain Spotted Fever. I prescribe 100 mg two times a day, although reports from colleagues inform me that they have increased that dose in adults to 200 mg two times a day. I treat pending the results of the tick report. If the tick wasn’t tested, I might treat for three to six weeks depending on the individual. In a small child, I use the following dosage for doxycycline: 2 mg/kg/day divided by two.5 If for any reason I need to treat a child under eight years old longer than three weeks, I would then switch to an alternative antibiotic such as azithromycin or amoxicillin. Recent studies have documented that a short course of doxycycline does not cause dental staining so may be used in a young child.6
End of Story Now?
From past “Pediatric Pearls,” the Townsend Letter reader may be familiar with my stance on treating COVID-19 using ivermectin. There were several factors that prompted me to begin treatment in Sophia:
- Significant symptoms at the start of infection
- Underlying chronic infection
- A history of difficulty clearing routine viral infections
- Concern regarding the effects of COVID-19 on someone with an impaired immune response.
Because ivermectin has been shown to have antimicrobial, antiviral (both RNA and DNA virus) and anti-parasitic action, I began a five-day course, 12 mg, two times a
day.7 To my knowledge, I have not read any studies regarding clinical outcomes of patients with tick-borne infections and COVID-19. Additionally, support was given to boost the innate immune system (NK cells, dendritic cells, macrophages, phagocytes, and mast cells), which is important in clearing COVID-19. Some of the other supplements prescribed included vitamin C, vitamin D, NAC, zinc picolinate, quercetin, curcumin, lumbrokinase, beta-glucans, and probiotics. One product that I think may be of particular benefit in this subgroup of COVID-19 patients is Transfer Factor Multi-Immune® which has been shown to increase NK function and was added to her protocol.8
Never-Ending Story
Over the following three weeks, Sophia had clinically improved and the majority of her symptoms resolved. However, the profound fatigue which she had experienced in the past, exacerbated by COVID-19, persisted. Hopefully, with the addition of mitochondrial support, she will continue to progress to her baseline. The looming question of long covid comes to mind and hopefully Sophia will not have to add this disorder to her list of chronic diseases she is managing at 16 years old.
References
- Nadelman, Wormser. Reinfection in Patients with Lyme Disease; Clinical Infectious Diseases. October 2007; 45 (8): 1032–1038.
- https://portal.ct.gov/-/media/CAES/DOCUMENTS/Publications/Bulletins/b1010pdf.pdf
- Nadelman, R. Erythema migrans; Infect Dis Clin North Am; 2015 Jun;29(2):211-39.
- Karvonen, K, Gilbert, L. Effective killing of Borrelia burgdorferi in vitro with novel herbal compounds; Gen Med Open, 2018; 2(6): 1-4.
- https://online.epocrates.com/drugs/20302/doxycycline/Peds-Dosing
- Poyhonen H, et al. Dental staining after doxycycline use in children; J Antimicrob Chemother; 2017 Oct 1;72(10):2887-2890.
- Heidary, F., Gharebaghi, R., Ivermectin: A systematic review from antiviral effects to COVID-19 complemental regimen; J Antibiot (Tokyo); 2020 Sep;73(9):593-602.
- Freund-Brown J, et al. Strategies to Enhance NK Cell Function for the Treatment of Tumors and Infections; Crit Rev Immunol. 2018;38(2):105-130.