By Tori Hudson, ND
Osteoporosis is one of the chronic health conditions for which many women seek my input and recommendations. This is a challenging area for practitioners who have a priority for natural medicines. While natural medicine and lifestyle issues are fundamental to prevention of osteoporosis and osteoporotic-related fractures, natural medicine-only treatment interventions can be naïve and insufficient for statistical and meaningful fracture prevention in what might be years from the present. On the other hand, the conventional medications come with risks along with the benefits… and some of the risks are not an acceptable risk for many patients. It is important to educate the patients on the risks of inadequate treatment, while also weighing the benefits and the risks of treatment options.
What I am going to focus on in this article is to point out some key aspects of osteoporosis, the prevalence, risk factors, and assessment and indications for bone density testing. The reason for this is that I find too many practitioners of all disciplines, just jump to exercise, vitamin D and other supplements and/or pharmacologic agents and do not do the due diligence of evaluation of the condition itself. I will not review with any depth the nonpharmacologic treatments and lifestyle modification and the pharmacologic agents for prevention of bone loss and treatment of osteoporosis.
Osteoporosis is the most common bone disorder in humans and is a general skeletal disorder characterized by a decrease in bone strength that then predisposes an individual to an increased risk of fracture with the most important sites being the spine and hip. Osteoporosis-related serious fractures occur most often in older postmenopausal women and can be life altering. The bone loss during the menopause transition and the early part of menopause is what results in osteoporosis. Fractures that are less serious than the spine or hip are those in the wrist in postmenopausal women often in their 50s and 60s that can be early warning signs of osteoporosis.
Fortunately, we can identify osteoporosis and identify those women who are at high risk of fracture. Evaluating skeletal health should be a skill set of all primary health care providers, especially those who offer primary care to postmenopausal women.
Osteoporosis is determined by bone densitometry and, according to the World Health Organization (WHO), is defined by a bone mineral density (BMD) T-score less than or equal to -2.5 at the total hip, femoral neck, or lumbar spine (with at least two vertebral levels in the posteroanterior position) in a postmenopausal woman or a man over age 50.1,2 Most other organizations support this description. The presence of a fragility fracture also justifies a clinical diagnosis of osteoporosis.
There has been a shift in the thinking about the term “osteopenia.” The diagnosis of osteopenia, or low BMD does not necessarily mean that she has experienced bone loss. The term is now thought to have limited clinical value because it includes young postmenopausal women without other risk factors who are actually at low risk of fracture while also including older women with other risk factors who are at very high risk of fracture.
In addition to BMD, a clinical diagnosis of osteoporosis can be made in postmenopausal women who have a fracture of their spine or hip or who have other factors that result in a high risk of fracture.
Osteoporosis is also categorized as either primary or secondary. Primary osteoporosis is related to bone loss that occurs after menopause as women age. Secondary osteoporosis is diagnosed when it is secondary to issues such as glucocorticoids, vitamin D deficiency, hyperthyroidism, hyperparathyroidism, renal calcium leak or other diseases that contribute to bone loss. It is important that clinicians learn to evaluate for secondary causes of bone loss to rule out these other causes.
Prevalence, Morbidity, and Mortality
In the National Health and Nutrition Examination Survey of 2013-2014, 16.5% of American women aged 50 years or older had osteoporosis at either the femoral neck or lumbar spine.3 The prevalence of osteoporosis of the femoral neck increases with age from 6.8% in women aged 50-59 to a striking 34.9% in women aged 80 years and older.4 Black American women have the highest BMD and Asian American women have the lowest.5 Most osteoporosis fractures occur in postmenopausal women, with two-thirds of them after age 75.6 For a white American woman aged 50 years, her risk of having an osteoporotic fracture in her remaining years is about 40%; and if you break it down, it’s 17.5% for the hip, 16.0% forearm, and 15.6% for a symptomatic vertebral fracture.7
Hip fractures after age 82 are the most life altering and up to a 25% increase in mortality within one year of the fracture.8; And it’s not just mortality—up to 25% of women require long-term care after a hip fracture and 50% will have some long-term loss of their mobility.9
Risk Factors and Risk Assessment
Risk factors for low BMD include advanced age, thinness (<127 lb), genetics, and smoking. Numerous diseases and medications have negative impact on bone, including eating disorders, rheumatoid arthritis, celiac disease, hyperparathyroidism, Cushing’s syndrome, aromatase inhibitors, glucocorticoids and gastric bypass surgery. Proton pump inhibitors are associated with increased fracture risk without causing bone loss. Counterintuitive to many, It turns out lifetime intake of calcium or vitamin D, alcohol, caffeine, or current or past physical activity are not predictors of low BMD. In addition, disorders and drugs that affect muscle strength, balance, and eyesight increase the risks of falls and fracture.
The tools to evaluate risk include a comprehensive history and physical exam with an eye towards yellow and red flags. These include surgical menopause and not on extended menopause hormone therapy, premature ovarian insufficiency and not on menopausal hormone therapy until at least age 51, and early menopause (onset between 40-45) and not on menopausal hormone therapy until at least age 51. Other key historical findings are a parent with a history of hip fracture, being a current smoker, consuming more than three servings of alcohol daily, and the diseases and medications mentioned earlier. Other known risk factors for fracture include dementia, low physical activity, thoracic kyphosis, rates of bone loss, weight loss, and loss of height.10
The primary objective tool for assessing bone density is a DXA scan, but ultrasound and quantitative computed tomography (CT) can also be used—although they should not be substitutes for DXA and the T-scores of the hip or spine obtained with DXA scans.
The most important risk factors for fracture in postmenopausal women are a history of a previous fracture or falls, older age, and low BMD. Combining these and other independent risk factors improves the clinician’s ability to identify women at high fracture risk. The computer-based algorithm, FRAX is a tool that can easily be learned to determine risk and is available online at www.sheffield.ac.uk/FRAX/. The FRAX calculation is now often reported in DXA reports.
Indications for Bone Density Testing
Bone density testing should be done in postmenopausal women with risk factors for low bone density and where knowing that will influence the clinical management:
- Women with a history of postmenopausal fracture
- Women with known medical causes of bone loss or fracture
- Women 65 and older
- Women 50 and older and with one or more additional risk factors of
- Weight less than 127 lb
- Family history of hip fracture in a mother or father
- Currently a smoker
- Discontinuing her systemic menopausal hormone therapy with additional risk factors for fracture.
For postmenopausal women aged 50 to 64 years with baseline T-scores greater than -1.5, retesting can wait until age 65. Age 65 is the age at which routine BMD screening is recommended for all women. Retesting earlier can be considered in women within five years of menopause whose initial BMD T score was worse than -1.5 or in those with other risk factures such as a prior postmenopausal fracture or if they have medical problems or medications associated with bone loss.
A comprehensive physical exam for osteoporosis evaluation should include an assessment of kyphosis, muscle strength, balance, height, weight, oral health (gum disease, tooth loss, tooth fractures), bone tenderness of thoracic vertebrae and anterior tibia and joint laxity.
Laboratory testing should be done prior to any intervention for women with osteoporosis, to evaluate for secondary causes of bone loss. Routine tests include CBC, general serum chemistry (especially serum calcium, creatinine, alkaline phosphatase, albumin, serum phosphate), and serum vitamin D. A 24-hour urinary calcium excretion test is used to test for poor calcium absorption and hypercalciuria. Other special tests can be considered based on abnormal values of any of the above, other special cases of osteoporosis, or clinical indications of other diseases that affect bone loss. Serum markers of bone turnover, while popular amongst integrative, functional medicine, and alternative-minded practitioners, cannot diagnosis osteoporosis and have unpredictable ability in assessing fracture risk. Their primary value has been in clinical trials where large groups of women are studied and group responses to treatment are assessed. For individual patient evaluation of women with osteoporosis, it is not recommended.
Nonpharmacologic Treatments and Lifestyle Modifications
The whole point of management of bone health in postmenopausal women is to minimize bone loss and reduce the likelihood of fractures. All postmenopausal women, whether they have low bone density, osteoporosis or already have had a postmenopausal osteoporosis-related fracture, should be educated and urged to make lifestyle modifications to support general health and bone health. Examples include a balanced, whole foods-oriented diet with adequate intakes of calcium, vitamin D, adequate physical activity and to avoid smoking and excess alcohol. However, it is important to appreciate that these efforts will not prevent bone loss in early menopause, will not significantly increase BMD in postmenopausal women, and are not adequate treatment interventions for women with osteoporosis.
Most of the research studies that have been done to evaluate non-pharmacologic treatments and lifestyle changes are small and short and as such, recommendations are usually based on systematic reviews, meta-analysis and opinions of expert committees. While it is true that intakes of calcium and vitamin D are required for normal skeletal growth in childhood, the data is less clear for healthy postmenopausal women. The Institute of Medicine (IOM) committee proposed daily intakes of calcium for postmenopausal women of 1,000-1,200 mg/day with an upper limit of 2,000 mg/day but note that these recommendations are based on uncertain and even inconsistent data. It is important to note that the average daily dietary intake of calcium for women in the US and Canada is 700 mg-800 mg daily. About one third of that comes from dairy products which would mean if a woman consumed an average dairy-free diet, her diet would contain only amount 500 mg/day of calcium. That leaves us with women consuming daily dairy of about 250 mg; and assuming the other 500 mg comes from non-dairy sources, she would need to add 250 mg to 450 mg/daily of supplemental calcium. For most dairy-free women, they would need to add 500 mg to 700 mg daily. When I review a woman’s dietary calcium intake, I use a simple list of calcium content foods to estimate her dietary daily calcium. The National Institute of Health Osteoporosis and Related Bone Diseases National Resource Center has a simple list.
To highlight the importance of estimating dietary calcium, and then recommending women supplement the difference to get up to the total of 1,000-1,200 mg/day, in the Women’s Health Initiative (WHI) calcium and vitamin D study, the average calcium intake was about 1,100 mg daily. In the group that added another 1,000 mg of daily calcium supplement, the risk of kidney stones was increased by 17%.11; There have been reports of the possibility that a calcium supplement of 1,000 mg/day with a total diet plus supplement of 2,000 mg/day is associated with increased cardiovascular risk.12,13 Any association of total calcium intake with cardiovascular risk was not seen in the WHI.14; An analysis published in 2016 found that a calcium intake of 2,000 mg-2,500 mg/day was not associated with cardiovascular risk in health adults.15 Due to any lack of benefit for a total of more than 1,200 mg/day of dietary plus supplemental calcium, the recommendation of about 1,200 mg/day total is still given for postmenopausal women with or without osteoporosis and for women of any age with osteoporosis.
The IOM recommends 600 IU/day of vitamin D for women between 50 and 70 years of age and 800 IU daily for women older than 70. However, the recommendations were based on the fact that these doses were sufficient to achieve a serum 25-OHD level of at least 20 ng/mL in most postmenopausal women. Not all are happy with this threshold and cite that it should be at least 30 ng/mL. While surprising, most studies report no benefit of calcium and/or vitamin D on fracture risk. This inability might be related to calcium and vitamin D being threshold nutrients, with severe deficiencies being harmful, but intakes more than the threshold to avoid deficiency does not really provide additional benefit. The effects of vitamin D with calcium on fracture risk have been mostly observed in women who are institutionalized or in older women with vitamin D deficiency.16; Even the US Preventive Services Task Force (USPSTF) has chimed in concluding that there was insufficient evidence to assess the balance of the benefits and harms of a daily supplementation of vitamin D 400 IU or more and calcium of 1,000 mg or more for primary prevention of osteoporosis in non-institutionalized postmenopausal women.17
Even women with osteoporosis do not require more calcium or vitamin D than women with normal BMD unless they have what is defined as a deficiency.
A few other supplements of note. Strontium has received some attention, but it is important to realized that the drug, strontium ranelate, a strontium salt was never approved in the US or Canada and even now is not available in other countries due to concerns about increased cardiovascular risk. There is no evidence for other strontium salts sold as dietary supplements when it comes to support for bone health. Magnesium, manganese, copper, zinc, folic acid, boron, vitamin C and more have scant data but are often included in multi-ingredient bone health supplements to support the potential benefits on bone metabolism, bone strength, bone architecture, but doubtful for bone density.
Vitamin K is more interesting and does have individual study data of some compelling importance. I go into some detail here, as it is the one supplement I feel may have some hope for my patients who have osteoporosis and decline drug therapy. Vitamin K is required for the production of the bone protein osteocalcin. Osteocalcin draws calcium to bone tissue, enabling calcium crystal formation. Osteocalcin provides the protein matrix for mineralization and is thought to act as a regulator of bone mineralization.18 Vitamin K plays a key role in the formation, remodeling, and repair of bone by attracting calcium to the site of this protein matrix.19 A low dietary intake of vitamin K seems to increase the risk of osteoporotic hip fractures in women, according to data from the Nurses’ Health Study.20
There are various forms of vitamin K, but the human trials have been done on vitamin K1(phylloquinone), MK4, (MK4, a form of vitamin K2) and menaquinone-7 (longer-chain MK7).
In a double-blind study, 452 men and women (ages 60-80 years) received a multiple vitamin/multimineral supplement providing 600 mg/day of calcium and 400 IU/day of vitamin D, plus either 500 mcg/day of vitamin K1 or no vitamin K1.21 BMD (determined by DEXA) and bone turnover were measured at 6, 12, 24, and 36 months. There were no differences in BMD at the femoral neck, lumbar spine, or total body between the two treatment groups, indicating that vitamin K1 did not enhance the effects of calcium, vitamin D, or other nutrients in this patient population. In the double-blind ECKO trial,22 a daily 5-mg supplement of vitamin K1 for two to four years did not protect against an age-related decline in BMD in postmenopausal women with osteopenia, but significantly fewer women in the vitamin K1 group than in the placebo group had fractures.
Epidemiologic evidence has shown associations between low dietary intake of vitamin K and increased bone loss in elderly men and women. A 2006 meta-analysis of 13 randomized controlled trials23 that gave vitamin K1 or MK4 (a form of vitamin K2) supplements for longer than six months reported data on bone loss and fracture rates. All but one study showed a reduction in bone loss with supplemental vitamin K. All seven of the 13 studies that reported fracture data were in Japanese individuals and used MK4. Most of these trials used a high dose, 45 mg/day.
Although the recommended dietary intake of vitamin K is 90 to 120 mcg/day, the optimal dose and form of vitamin K supplementation to achieve a protective effect on bone loss and fracture reduction is not known. The majority of studies used MK4 at doses approximately 400-fold higher than dietary recommendations for vitamin K1. An additional issue is that these studies have been conducted almost exclusively in Japanese postmenopausal women. This population group may be influenced by unique dietary, environmental, and/or genetic factors, so it is not clear whether the findings from these studies can be generalized to other populations. In contrast to the seven positive Japanese studies, in a double-blind trial, 381 postmenopausal women received either phylloquinone (1 mg/day), MK4 (45 mg/day), or placebo for 12 months.24 No effect of phylloquinone or MK4 on the bone density of the lumbar spine or proximal femur was observed.
Two long-term trials have previously been done evaluating the effect of vitamin K1 supplementation on bone loss. In one study using 1 mg/day of vitamin K1 plus calcium and vitamin D for 3 years in postmenopausal women aged 50 to 60 years,25 bone loss was reduced at the femoral neck, but there was no beneficial effect on spinal bone density. In a second study,26 200 mcg/day of vitamin K1 plus calcium and vitamin D given for two years to nonosteoporotic women aged 60 years or above resulted in a modest increase in BMD of the radius but not the femoral neck.
Menaquinone-7, or MK-7 (a longer-chain form of vitamin K2), is found in natto (highest concentration in fermented soybeans) and cheese and in lower concentrations in meat and other dairy products; a very small amount is produced by gut bacteria from dietary vitamin K1.27 MK-7 has been found in animal studies to be more potent and more bioavailable as well as to have a longer half-life than MK4. When taken as a daily supplement ( 0.22 μmol/day), MK-7 is more effective than K1 in carboxylating osteocalcin This is thought to be due to MK-7’s much longer residence time and the higher serum concentrations of MK-7 achieved during its prolonged intake.28 The longer-chain menaquinones such as MK-7 are much more hydrophobic, which contributes to their much longer half-lives (8 hours for K1 and MK-4 vs. 96 hours for MK-7).29 In a study of Japanese postmenopausal women, a significant inverse association was found between natto consumption and the incidence of hip fractures.30 In a study of osteoporosis after organ transplantation, one year of MK-7 supplementation (180 mcg/day) resulted in increased bone mineralization compared with placebo.31 However, a study of early menopausal women given one year of supplementation of 360 mcg/day of MK-7 in the form of natto capsules did not show a significant improvement in bone density despite a reduction in uncarboxylated osteocalcin.32 A likely reason for these inconsistent results is the confounding effect of vitamin D status. The study in post-transplant patients noted a high incidence of vitamin D deficiency, which was found to affect the results.
Lastly, a meta-analysis published in 2019 found no evidence that vitamin K affects bone density or vertebral fracture risk in postmenopausal women and the evidence confirming a reduction in clinical fractures was insufficient.33
Too much dietary protein or protein deficiency can be problematic for bone. In older women who are prone to falling and losing weight, a higher protein intake has been associated with reduced frequency of falling.34
Phytoestrogens, namely isoflavones have moderately beneficial effects in slowing the bone loss associated with menopause in a systematic review.35
We know that bone mass is impacted by impact loading exercise during childhood and that immobilization is associated with low bone mass. But, a Cochrane review and several meta-analyses are sobering in that they found relatively small, statistically significant effects of exercise on BMD in postmenopausal women.36-38
Most fractures occur as a result of a fall and exercise programs that emphasize balance, gait, and muscle strength are very effective ways to prevent falls and perhaps fractures. In women aged 65 years and older, at least one-third of these women experience one or more falls each year. This risk only increases with age, as does the risk of fracture. Assuring adequate vision, a safe home, and attention to medications are important. Tapering the use of benzodiazepines, neuroleptic agents, and antidepressants can reduce the risk of falling by more than 60%.
Pharmacologic Therapy to Prevent Bone Loss and to Treat Osteoporosis in Postmenopausal Women
This section will be brief and only key points summarized. Much data is available for your perusal should you be interested. Benefits and risks are specific to each agent, dose and duration.
Current drugs and doses approved in North America for preventing osteoporosis
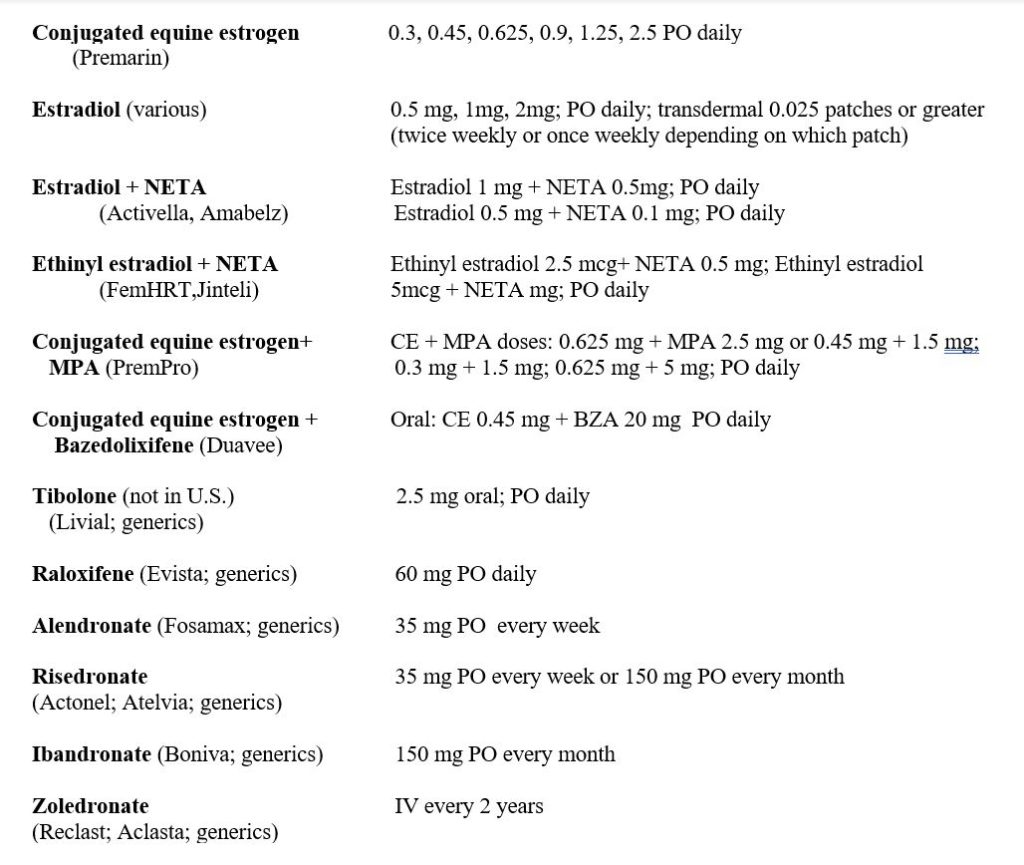
Prevention of Bone Loss. The mechanisms of action of all osteoporosis pharmacologic agents are to either inhibit or to activate bone metabolism. The anti-remodeling agents, also called antiresorptive drugs, include systemic estrogen, estrogen agonists/antagonists, bisphosphonates, and denosumab. They all inhibit bone resorption and to a lesser extent, bone formation. These medications maintain or improve BMD and reduce the risk of fracture but do not improve or repair trabecular bone structure.
Treatment. The primary objective of treating women with osteoporosis is to reduce the risk of fracture. All the approved drugs for treatment have been shown in randomized controlled trials to reduce the risk of fracture. Anti-remodeling drugs inhibit bone resorption by osteoclasts and, to a lesser degree, inhibit bone formation. Treatment with these agents fills in remodeling spaces in bone that are present before treatment starts and also results in opening of fewer new remodeling spaces. This results in an increase in BMD, bone strength, and decreased fracture risk.
Some of the newest bone drugs in use are actually bone-building drugs that stimulate bone formation and restore the trabecular bone structure while these bone-forming properties decline over time. For these reasons, these drugs are to be limited to treatment intervals of 12 to 24 months. When the osteoanabolic agents are discontinued, bone mineral density is rapidly lost, and these therapies are then followed by an anti-remodeling drug.
BMD testing is likely repeated one to two years after beginning osteoporosis drug treatment. For those women on bisphosphonates, the BMD test is done again at five years to consider the option of taking a bisphosphonate holiday.
| (Fracture Risk Reduction) | Vertebral | Nonvertebral | Hip | |
| Raloxifene (Evista; generics) | 60 mg/day PO | X | ||
| Alendronate (Fosamax; generics) | 70 mg q wk PO | X | X | |
| Risedronate (Actonel; generics) | 35 mg q wk PO Or 150 mg q mo PO | X | X | X |
| Ibandronate (Boniva; generics) | 150 mg PO q mo Or 3 mg IV q 3 mo | X | ||
| Zoledronate (Reclast; generics) | 5 mg IV q year | X | X | X |
| Denosumab (Prolia) | 60 mg AQ q 6 mo | X | X | X |
| Teriparatide (Forteo) | 20 mcg SQ daily | X | X | |
| Baloparatide (Tymlos=US only) | 80 mcg SQ daily | X | X | |
| Romosozumab (Evinity) | 210 mg SQ q mo | X | X | X |
| Calcitonin-salmon (Calcimar;(or generics) | 200 USP units; nasal spray daily | X |
Current Drugs Approved in North America for Treatment of Postmenopausal Osteoporosis
The prescribing of these prevention and treatment drugs are likely best done by osteoporosis experts, most often an endocrinologist or rheumatologist.
The role of the integrative, natural medicine or functional medicine clinician is to know the benefits and risks of all treatment options, non-pharmacologic and pharmacologic, and then to integrative strategies in the safest way possible.
Conclusion
At the forefront of our minds, it should be known that osteoporosis is a chronic, progressive condition; and it affects a large percentage of postmenopausal women. Women’s health care practitioners and especially menopause practitioners should be familiar and comfortable with assessment and management, or refer to those that are. A naïve and uninformed clinician can miss the opportunity to accurately diagnose, individually assess fracture risk, individualize treatment approaches and truly present women with options that include the whole spectrum of prevention and treatments. Under treatment is just as harmful or perhaps more so, than over treatment. In the end, educating women with accurate studious information and the tools to make informed decisions that they feel the most comfortable with and realistically confident in, is a critical aspect of offering good, respectful medical care.
References
- Riggs BL, Melton LH III . The worldwide problem of osteoporosis: insights afforded by epidemiology. Bone 1995;17(suppl 5):505S-511S.
- Kanis J. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO sStudy Group. Osteoporos Int. 1994;4:368-381.
- Looker A, Sarafrazi Isfahani N, Fan B, Shepherd J. Trends in osteoporosis and low bone mass in older US adults, 2005-2006 through 2013-2014. Osteoporos Int 2017; 28:1979-1988.
- Wright N, Looker A, Saag K, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res 2014;29:2520-2526.
- Barrett-Connor E, et al. Osteoporosis and fracture risk in women of different ethnic groups. J Bone Miner Res 2005;20:185-194.
- Hernlund E, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation and the European Federation of Pharmaceutical Industry Associations. Arch Osteoporosis 2013;8:136.
- Cummmings S, Melton L. Epidemiology and outcomes of osteoporotic fractures. Lancet 2002;359:1761-1767.
- Brauer C, Coca-Perraillon M, Cutler D, Rosen A. Incidence and mortality of hip fractures in the United States. JAMA 2009;302:1573-1579.
- Ferrari S, et al. Unmet needs and current and future approaches for osteoporotic patients at high risk of hip fracture. Arch Osteoporos 2016;11:37.
- Ambrose A, Paul G, Hausdorff J. Risk factors for falls among older adults. A review of the literature. Maturitas 2013;75:51-61.
- Wallace R, et al. Urinary tract stone occurrence in the WHI randomized clinical trial of calcium and vitamin D supplements. Am J Clin Nutr 2011;94:270-277.
- Bolland M, et al. Vascular events in healthy older women receiving calcium supplementation: randomised controlled trial. BMJ 2008;336:262-266.
- Bolland M, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ 2010; 341:c3691.
- Prentice R, et al. Health risks and benefits from calcium and vicamint D supplementation: Women’s Health Initiative clinical trial and cohort study. Osteoporos Int 2013; 24:567-580.
- Chung M, et al. Calcium intake and cardiovascular disease risk: an updated systematic review and meta-analysis. Ann Intern Med 2016;165:865-866.
- Bouillon R, Lips P. Bilezikizn J. Vitamin D supplementation and musculoskeletal health. Lancet Diabetes Endocrinol. 2019;7:85-86.
- Preventive Services Task Force US, Grossman D, Curry S, Owens D, et al. Interventions to prevent falls in community-dwelling older adults: USPSTF Recommendation Statement. JAMA 2018;319:1696-1704.
- Ducy, P, et al. Increased bone formation in osteocalcin-deficient mice. Nature. 1996;382(6590):448-452.
- Booth SL, et al. Dietary vitamin K intakes are associated with hip fracture but not with bone mineral density in elderly men and women. Am J Clin Nutr 2000;71:1201-1208.
- Feskanich D, et al. Vitamin K intake and hip fractures in women: a prospective study. Am J Clin Nutr 1999;69:74-79.
- Booth S, et al. Effect of vitamin K supplementation on bone loss in elderly men and women. J Clin Endocrinol Metab 2008;93:1217-1223.
- Cheung A, et al. Vitamin K supplementation in postmenopausal women with osteopenia (ECKO Trial): A randomized controlled trial. PLoS Med. 2008 Oct 14;5(10):e196.
- Cockayne S, et al. Vitamin K and prevention of fractures. Systematic review and meta-analysis of randomized controlled trials. Arch Intern Med 2006;166:1256-1261.
- Binkley N, et al. Vitamin K treatment reduces undercarboxylated osteocalcin but does not alter bone turnover, density or geometry in healthy postmenopausal, North American women. J Bone and Mineral Research. 2009;24(6):983-991.
- Braam L, et al. Vitamin K1 supplementation retards bone loss in postmenopa-usal women between 50 and 60 years of age. Calcif Tissue Int. 2003;73:21-26.
- Bolton-Smith C, et al. Two-year randomized controlled trial of vitamin K1(phylloquinone) and vitamin D3 plus calcium on the bone health of older women. J Bone Miner Res. 2007;22:509-519.
- Schurgers LJ, et al. (June 1999) Nutritional intake of vitamins K1 (phylloquinone) and K2 (menaquinone) in the Netherlands. J,Nutr. Environ. Med. June 1999;9(2):115–122.
- Schurgers LJ, et al. Vitamin K-containing dietary supplements: comparison of synthetic vitamin K1 and natto-derived menaquinone-7. Blood 2007 Apr 15;109(8):3279-3283.
- Schurgers LJ, Vermeer C. Differential lipoprotein transport pathways of K-vitamins in healthy subjects. Biochim Biophys Acta. 2002 Feb 15;1570(1):27-32.
- Kaneki M, et al. Japanese fermented soybean food as the major determinant of the large geographic difference in circulating levels of vitamin K2: possible implications for hip-fracture risk. Nutrition 2001;17:315-321.
- Forli L, et al. Dietary vitamin K2 supplement improves bone status after lung and heart transplantation. Transplantation. 2010 Feb 27;89(4):458-464.
- Emaus N, et al. Vitamin K2 supplementation does not influence bone loss in early menopausal women: a randomised double-blind placebo-controlled trial. Osteoporosis Int. 2010 Oct;21(10):1731-1740.
- Mott A, et al. Effect of vitamin K on bone mineral density and fractures in adults: an updated systematic review and meta-analysis of randomised controlled trials. Osteoporos Int 2019;30:1543-1559.
- Zoltick E, et al. Dietary protein intake and subsequent falls in older men and women: the Framingham Study. J Nutr Heatlh Aging 2011; 15:147-152.
- The role of soy isoflavones in menopausal health: report of the NAMS/Wulf Utian Translational Science Symposium in Chicago, Il (October 2010). Menopause 2011; 18:732-753.
- Howe T, et al. exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev 2011;CD000333.
- Kistler-Fischbacher M, Weeks B, Beck B. The effect of exercise intensity on bone in postmenopausal women (part 1): a systematic review. Bone 2021;143:115696.
- Kistler-Fischbacher M, Weeks B, Beck B. The effect of exercise intensity on bone in postmenopausal women (part 2): a meta-analysis. Bone 2021; 143:115696.