By Carolyn McMakin, MA, DC
Most of us think of the brain as the structure inside our skull with which we think. But the brain does not just think, and it is more important to know how the brain works and “why” it creates your behavior and body functions than what you think it thinks.
The first thing you need to know about this article is that it is impossible to describe the brain, the glial cells, the blood brain barrier, the relationship of the brain to the gut, the immune system, and fibromyalgia in 2,500 words. The intention here is to provide a framework that will lead you to further study and understanding.
The brain starts wiring itself in utero. Let’s assume nothing goes wrong there, and the wiring and cells are all correct. There are 171 billion cells in the brain. About half of those are glial cells, which provide structural and immune support. The neurons communicate with each other, with the body and all of its organs, and the immune and endocrine systems with small peptides called neurotransmitters. Each neurotransmitter does a different thing in a different part of the brain and in different neurons. Each part of the brain does a different thing, but every part of the brain is connected to every other part of the brain and communicates instantaneously with every other part of the brain.
Every immune system cell, every white blood cell, and every cell in your intestines have receptors for every neurotransmitter. The peptides that make up every neurotransmitter are absorbed through the gut and modified either in the brain or in some organ. In other words, the brain and everything is connected to everything by these neurotransmitters. For this discussion, we will look at the neurons and neural pathways rather than the glial cells or neurotransmitters, but there is no way to do that without talking about the gut and we will get to that eventually.
The following example doesn’t have anything to do with fibromyalgia, but it demonstrates how a simple action like scratching your nose depends on virtually every part of the brain and how every part of the brain communicates with every other part of the brain and influences behavior, pleasure and pain.
There are special nerves that sense when something irritates the skin. Those nerves send signals through a nerve to the spinal cord. The signals travel up the spinal cord through the medulla and send a little signal to the cerebellum that tells your muscles where the itch is and how to coordinate the movement that will allow you to scratch it, if and when you decide to scratch it. But in the millisecond that passes before you scratch, the signal goes to the periaqueductal gray (PAG) shown in the small blue circle just above the medulla. The PAG plays a critical role in motivated behavior and in behavioral responses to threatening stimuli. The PAG “decides” if the itch is threatening or dangerous. If the itch is caused by an insect bite, the PAG determines threat immediately, overrides any input that suggests you should not scratch, and the bite is scratched immediately and vigorously. But if the itch is just a small random signal from the dry skin the PAG won’t detect it as a threat.1,2

The PAG is the primary control center for descending pain modulation. It has cells that suppress pain by producing small peptides called enkephalins that bind to the morphine receptors in the brain. These enkephalins suppress pain, and they are why the signal from the nerve is perceived as an itch rather than pain and a threat. The secretions of the PAG allow you to suppress the itch when the rest of the circuit decides you should not scratch it.
From there the signal goes to the thalamus, which serves as a switching center that takes incoming signals from the spinal cord, medulla, and PAG and sends them to different parts of the brain. First the thalamus sends the “itch” signal from the PAG to the insula. The insula senses the internal state of the body, decides whether the input is important and whether the input is painful. The insula assesses and determines the intensity of incoming pain signals.
The thalamus sends the “itch” signal to the anterior cingulate cortex, ACC in the illustration. The ACC “decides” how much attention to devote to this itch, how good it Is going to feel to scratch it; and it also “decides” whether scratching this itch in this moment is a good idea. When you’re speaking in front of an audience, the ACC decides whether it is appropriate or OK to scratch your nose or your backside while you’re speaking. The ACC helps you suppress the itch and allows you to deliver your speech or perform whatever action you’re doing even though your nose itches based on the input from the other parts of the brain in this pathway. Everything is connected to everything.3
Then the signal goes to the prefrontal cortex (PF) that “knows” or signals how good it is going to feel when you scratch the itch, and it also decides whether it is appropriate to scratch the itch during your speech or whether it is going to hurt when you scratch that spot if it itches a lot and is already raw. The PF interprets the urge to scratch and has the cortex think about it and decide whether it is OK to scratch.4
At the same time, the signal goes to the sensory motor cortex that tells your hand where to go to scratch that spot and then initiates the movement that will turn into scratching. The primary somatosensory cortex, SI in the diagram, tells you what muscles to move and where to move them and the secondary somatosensory cortex (SII), tells you exactly where to scratch what itches.
All of this happens in a millisecond. Each neuron in the pathway from the nose back to your fingers contributes to the “scratch” or “don’t scratch” decision instantaneously. If the “yes do scratch now” signals override the “no don’t scratch now” signals in the pathway, the motor cortex sends signals back down through the basal ganglia and the cerebellum to coordinate the movement; and you scratch exactly the spot that itches, for exactly the time that it takes to turn off the signals coming from the dry itchy spot. The neurology is intricate, complex, coordinated, instantaneous, and stimulated by a tiny bit of histamine and inflammation in the skin at the tip of one tiny neuron on your nose.
What does this have to do with fibromyalgia?
First you need to know that fibromyalgia is a neuro-endocrine chronic pain condition that affects the immune system, the endocrine system, the thalamus, the PAG, the insula, and the cortex; and fibromyalgia affects the gut and the brain and influences everything the patient thinks, feels, and does. You need to know that fibromyalgia has at least five different causes. Fibromyalgia patients all look the same when they arrive in your office, but they get there by different routes.
Twenty-seven percent to 40% of fibromyalgia starts with some sort of spine trauma.5 Spine trauma causes disc bulges that secrete a very inflammatory something called phospholipase A2 (PLA2) that can strip the myelin off of nerves and the anterolateral pain pathways in the spinal cord in 28 days.6-10 This interferes with the ascending spinal cord pain pathways that go up the cord to the brain and leads to something called thalamic pain syndrome or central pain.11 If the pain pathways in the spinal cord are interrupted, this creates constant pain signals for the whole body in the thalamus and insula. This strong, body wide, intense constant pain causes incredible stress perceived as threat that elevates cortisol and a neurotransmitter in the brain called corticotrophin releasing factor (CRF). CRF has effects that we’ll talk about shortly.
The other causes of fibromyalgia include severe prolonged stress that leads to increases in cortisol and, eventually, that increases CRF. CRF increases cortisol, and increased cortisol leads to thinning of the gut wall, and that leads to difficulty in transporting branch chain amino acids across the gut wall.12 The leaks in the small intestine allow small food peptides across the gut and that activates the immune system, 85% of which is clustered around the digestive system.13 Increases in cortisol eventually lead to further increases in CRF, and we’ll talk about that shortly.
Why are branch chain amino acids important? Tryptophan is the branch chain amino acid that builds serotonin. Serotonin is the neurotransmitter used by the periaqueductal gray to suppress pain, and it also helps you sleep. If your gut is thin and you cannot transport the bulky amino acid tryptophan, you can’t make serotonin; and you can’t suppress pain, or avoid depression, or enhance sleep.14, 15
Tyrosine is a bulky branch chain amino acid that makes dopamine. Dopamine creates sensations of pleasure and happiness and allows you to move in a coordinated way depending on what part of the brain is using it. Reduced dopamine means reduced feelings of pleasure.16
Leucine and isoleucine are branched chain amino acids that make the thyroid hormone receptors. If leucine and isoleucine are not available, the thyroid hormone receptors may not be made correctly; and even if the patient has enough thyroid, they may feel and act as if they are hypo-thyroid because the receptors can’t detect and react properly to the thyroid hormone. Most fibromyalgia patients feel as if they are thyroid deficient.17 Fibromyalgia patients have been found to be deficient in branch chain amino acids. Clearly, branch chain amino acids are important,
Some patients get fibromyalgia from toxic chemical exposures that change firing thresholds in nerves and the brain and can create body pain, which is perceived by the brain as a threat. The constant pain causes CRF to increase; we’ll talk about that shortly.
Some patients get fibromyalgia after a viral infection, live virus vaccine, or any infection such as Lyme, parasites or mold. The chronic infection turns the vagus nerve down or off. The vagus nerve has many functions, but in this case the most important function is that it suppresses T-cells and macrophages from the immune system and regulates digestion by increasing stomach acid and enzymes from the pancreas. Without enough stomach acid, the pH in the gut is alkaline and the good, healthy, acid-loving bacteria aren’t supported. Good bacteria in the gut digest your food, provide nutrients to every part of your body, and produce products that repair the gut wall. If the gut wall is not repaired, the gut leaks; and the immune system becomes hypervigilant because it picks up the small peptides that leak across the gut wall. Patients develop food sensitivities and allergies that increase histamine. Histamine acts as a neurotransmitter that keeps you awake and interferes with sleep. It doesn’t help that the vagus nerve isn’t doing its job of suppressing the immune system because it has been turned down or off by the infection.
Some patients have food allergies or sensitivities that lead to immune system activation and the production of histamine by an immune system cell called a macrophage. Macrophages eat the antigen/antibody complexes created by the food sensitivity and the macrophages literally explode releasing histamine.13 Histamine stimulates a slow unmyelinated Class-C pain fiber that creates full body aching pain.11 Full body aching pain creates stress and increases CRF, which we will talk about next.
Corticotrophin releasing factor (CRF) is produced in the hypothalamus in response to stress. CRF increases in your brain in response to pain when the stress response tells your system that you’re being dragged through the jungle by a tiger and you probably have 30 minutes to live. If you have only 30 minutes to live, there is no need for anything the vagus nerve does so it is just fine that the vagus is turned down or off.
CRF increases cortisol to help combat the inflammation created by the anticipated tiger bite, which further leads to thinning of the gut wall, which leads to increased leaking of peptides across the gut wall, which leads to further activation of the immune system by the increased food sensitivities and macrophage explosions, which leads to increased releases of histamine and increased body pain.
CRF acts centrally in the brain to suppress the critical endocrine hormones that help us feel healthy and normal. The brain assumes you don’t need these hormones because you have only 30 minutes to live.
CRF suppresses follicle stimulating hormone and luteinizing hormone that produce progesterone in females and sperm production and testosterone production in males. Progesterone helps a woman become pregnant and stay pregnant. If you have 30 minutes to live, why would you need progesterone? Women who are progesterone deficient are estrogen dominant. Excess estrogen competes with B6 for receptor sites in the anti-inflammatory prostaglandin pathway. This creates inflammation and literal brain and nervous system irritability, which increases the stress response and all that comes with it. Men who are testosterone deficient are depressed, have disturbed sleep, and don’t have good muscle repair.
CRF reduces thyroid stimulating hormone (TSH), centrally and prevents TSH from rising even though the patient is functionally hypothyroid because increased cortisol interferes with the conversion of the less active storage form of thyroid, T4, into T3 the active form of thyroid. The lack of leucine and isoleucine that make up the binding pocket on cells for thyroid hormone is caused by the thinning gut wall. This makes the thyroid hormone receptors less receptive to thyroid which compounds the situation.
CRF suppresses growth hormone centrally by reducing growth hormone releasing hormone (GHRH) in the brain. Fibromyalgia patients are growth hormone deficient. In an adult, growth hormone helps amino acids to cross muscle cell membranes and create muscle repair. If you don’t have growth hormone, you don’t have the muscle repair that happens every night to repair your muscles from the normal wear and tear of daily activities. CRF reduces growth hormone in the brain directly, and growth hormone is additionally reduced because 85% of growth hormone is made during deep sleep; fibromyalgia patients have an alpha wave that comes through and disrupts deep sleep. If you have 30 minutes to live, why would you need muscle repair or deep sleep?18-25
CRF reduces vagus activity because if you’re under stress and have 30 minutes to live you have no need for any of the things the vagus does. This interferes with digestive function, further increases immune system activation and inflammation, which exacerbates pain and stress. But since the vagus controls every muscle in the vocal cords except the vocal cord that creates high-pitched tones, turning off the vagus does allow you to scream. And screaming is important if you’re being dragged through the jungle by a tiger and you have 30 minutes to live.
CRF acts as a neurotransmitter in the brain, interfering with short-term memory and creating long-term memory biased to remember every bad thing that has ever happened to you. If you’re running away from a tiger in the woods and you have 30 minutes to live, you don’t need to know anything that happened recently, and you don’t need to do any complex cognitive activity. The only thing you need to remember is how you got away from the tiger the last time.
The thalamus and the insula, which normally suppress pain, begin to amplify pain since there is so much body pain and stress. No one knows why the thalamus/insula amplifies pain in fibromyalgia patients.26
All of this creates the neuro endocrine depressed, cognitively impaired, sleep-deprived, exercise intolerant, negative, irritable, focused on every bad thing that ever happened to them patient who walks into your office.
The most important thing you need to know about fibromyalgia is that it can be cured.
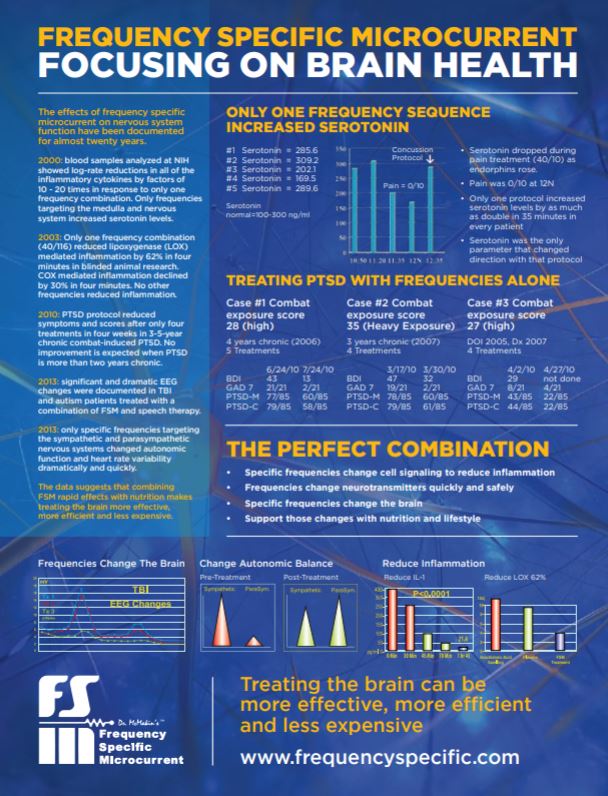
Fibromyalgia can be cured not in every patient or in every case, but it can be cured often enough that a cure should be the intention of treatment. It is cured by addressing what caused the fibromyalgia to begin with; but that is a topic for another article. I reduce the pain, quiet the thalamus and brain, repair the gut wall, and improve function of the vagus nerve with frequency specific microcurrent (FSM) as an adjunct. FSM is the primary treatment for fibromyalgia caused by spine trauma because it is the only thing that will relieve the inflammation and repair the spinal cord and reduce that particular pain. And reducing the pain is the only way to stop the neuro endocrine cycle that starts in the brain.27
The brain is intimately and instantly involved in everything we feel and do; it doesn’t just think or do what we think it does. And everything is connected to everything. It’s important to think about that because you have to address everything at the same time so you can break the cycle and return everything to normal so the patient can be and feel healthy again.
References
- Faull OK, et al. The midbrain periaqueductal gray as an integrative and interoceptive neural structure for breathing. Neuroscience and Biobehavioral Reviews. 2019; 98: 135–144.
- Silva C, McNaughton N. Are periaqueductal grey and dorsal raphe the foundation of appetitive and aversive control? A comprehensive review. Progress in Neurobiology. February 17, 2019;177: 33–72.
- Botvinick M, Cohen J, Carter C. Conflict monitoring and anterior cingulate cortex: an update. Trends in Cognitive Sciences. December 2008;8 (12): 539-546
- Arnsten A, Stress signaling pathways that impair prefrontal cortex structure and function. Nature Reviews Neuroscience. 2009, Jun;10(6): 410-422
- Buskilla D, et al. Increased rates of fibromyalgia following cervical spine injury: a controlled study of 161 cases of traumatic injury. Arthritis and Rheumatism. 1997; 40: 446-452.
- Olmarker K, Rydevik B, Nordberg C. Autologous nucleus pulposus induces neurophysiologic and histologic changes in porcine cauda equina nerve roots. SPINE. 1993; 18: 1425-32.
- Olmarker K, et al. Inflammatogenic properties of nucleus pulposus. SPINE. 1995; 20: 665-669.
- Ozaktay AC, Cavanaugh JM, Blagoev DC: Phospholipase A2-induced electrophysiologic and histologic changes in rabbit dorsal lumbar spine tissues. SPINE. 1995; 20: 2659-68.
- Ozaktay AC, Kallakuri S, Cavanaugh JM. Phospholipase A2 sensitivity of the dorsal root and dorsal root ganglion. SPINE. 1998; 23(12):1297-1306.
- Chen C, et al. Effects of phospholipase A2 on lumbar nerve root structure and function. SPINE. 1997; 22: 1057-64.
- Kandel E, Schwartz J: Principles of Neural Science, second edition. Elsevier Science Publishing Co., Inc., New York, 1985: pp. 331-336
- Maes M, et al, Serotonergic markers and lowered plasma branched-chain-amino acid concentrations in fibromyalgia, Psychiatry Research. December 2000; 97 (1):11-20.
- Baker, S, Bennet, P, Bland, J, et al, Textbook of Functional Medicine, Institute of Functional Medicine, 2005
- Moldofsky H. Rheumatic Pain Modulation Syndrome: The Interrelationship Between Sleep, Central Nervous System Serotonin, and Pain. Advancements in Neurology. 1982; 33:51-57.
- Juhl DO, John Fibromyalgia and the Serotonin Pathway. Alternative Medicine Review. 1998; 3 (5).
- Daubner S, Le, T, Wang, S, Tyrosine Hydroxylase and Regulation of Dopamine Synthesis, Arch Biochem Biophys, 2011, Apr 1: 508(1) 1-12
- Wejaphikul K, et al, Role of Leucine 341 in Thyroid Hormone Receptor Beta Revealed by a Novel Mutation Causing Thyroid Hormone Resistance. Thyroid. 2018, Nov 27
- Crawford LJ. Neuroendocrine Abnormalities in Fibromyalgia. American Journal of the Medical Sciences. 1998; 315(6): 359-366.
- Crawford LJ, Engleberg NC, and Demitrack MA. Neurohormonal Perturbations in Fibromyalgia. Rheumatic Disease Clinics of North America. 1996; 22(2): 267-284.
- Crawford LJ, et al. Hypothalamic-Pituitary-Adrenal Axis Perturbations in Patients with Fibromyalgia. Arthritis and Rheumatism. 1994; 37(11):1583-1592.
- Neeck G, Riedel W. Hormonal Perturbations in Fibromyalgia Syndrome. Annals of the New York Academy of Sciences. 1999; 876: 325-338.
- Maes M, et al. Increased 24-Hour Urinary Cortisol Excretion in Patients With Post-Traumatic Stress. Acta Psychiatrica Scandinavica. 1998;98(4): 328-335.
- Dessein PH, et al. Hyposecretion of Adrenal Androgens and the R elation of Serum Adrenal Steroids, Serotonin *** Pain. 1999; 83(2): 313-319.
- Dessein PH, et al. Neuroendocrine Deficiency-Mediated Development and Persistence of Pain in Fibromyalgia. Pain. 2000; 86(3): 213-215.
- Neeck G, Riedel W. Hormonal Perturbations in Fibromyalgia Syndrome. Annals of the New York Academy of Sciences. 1999; 876: 325-338.
- Mountz JM, et al. Fibromyalgia in women: abnormalities of regional cerebral blood flow in the thalamus and the caudate nucleus are associated with low pain thresholds levels. Arthritis Rheum. 38: 926-938, 1995
- McMakin C, Gregory W, Phillips T, Cytokine changes with microcurrent therapy of fibromyalgia associated with cervical trauma.” Journal of Bodywork and Movement Therapies. July 2005