By Leigh Erin Connealy, MD,
and Bita Badakhshan, MD
ABSTRACT
Melanoma accounts for just 1% of all skin cancers but is responsible for the majority of skin cancer deaths.1 Although surgical removal is often curative in early-stage melanoma, the risk of recurrence increases and prognosis worsens in advanced disease. We report on the case of a patient with recurrent stage 4 melanoma with metastasis to the liver. Early detection of recurrence with specialized blood tests of cancer biomarkers and treatment with integrative therapies led to an excellent response, and the patient is now in remission.
Introduction
Melanoma incidence is increasing in the US, with a 1.4% rise in new cases per year from 2009 through 2018.2 The prognosis for localized early-stage melanoma is excellent, but the five-year survival rate for metastatic melanoma is just 27%.3 Therefore, investigation into novel blood tests and effective therapies is needed to improve early detection and outcomes in melanoma and other cancers.
Several specialized blood tests are excellent adjuncts for early detection of cancer.4 Although these tests are underutilized in conventional oncology, they identify biomarkers indicative of cancer activity before signs and symptoms are evident on physical exam, routine blood tests, and imaging scans. They include the following:
- Phosphohexose isomerase (PHI), also called autocrine motility factor, is an enzyme involved in anaerobic metabolism. Elevations have been linked with increased tumor activity in cancers of the skin, liver, and other sites.5 Normal range: 15.6–31.4 U/L
- Circulating tumor cells (CTC)arecancer cells that are sloughed off from tumors and released into the bloodstream. Recurrence or metastasis occurs when these circulating cells take up residence in the initial tumor site or in other organs.6 CTCs can be detected by RGCC’s “liquid biopsy.” Normal range: 0 cells/mL
- Nagalase,oralpha-N-acetylgalactosaminidase, is an enzyme that inhibits Gc macrophage-activating factor (GcMAF) and interferes with the production of macrophages. Patients with cancer have elevated levels of nagalase, and the higher the level, the greater the tumor burden and the more aggressive the cancer.7 Normal range: below 0.95 nmol/min/mg
These tests are also useful for monitoring the effectiveness of therapeutic interventions and guiding treatment protocols, both conventional and integrative. (See sidebar for a brief description of integrative cancer therapies.) Here, we discuss a patient with MRI-documented recurrence of melanoma, diagnosed as stage 4 with metastasis to the liver, that was initially suspected based on PHI, CTC, and nagalase test results. Early detection of cancer activity plus a comprehensive integrative treatment program with a number of anti-cancer and supportive therapies resulted in regression and ultimate disease remission.
Case Description
A 50-year-old male consulted us in January 2016 for monitoring and treatment. He had been diagnosed with stage 3 melanoma in June 2014, with surgical removal of lesions on his back and left shin. Twelve lymph nodes were also removed, and one had microscopic metastasis. A PET scan in September 2014 was clear, and no further treatment was recommended. He was monitored by his oncologist with blood work every three to six months and had a CT scan at the end of 2015 that was negative. The patient also has a history of thyroid cancer, diagnosed and treated in 2014, and is status post radiation and thyroidectomy.
When we first saw the patient in January 2016, he had no complaints but, given his history of cancer, wanted to enhance his immune function and overall health. Blood work at the patient’s initial exam revealed that complete blood count (CBC), comprehensive metabolic panel (CMP), and high-sensitivity C-reactive protein (hs-CRP) were within the normal range and, in fact, remained so throughout his treatment course. However, his PHI and CTC were high at 60 U/L and 9.3 cells/mL, respectively, suggestive of ongoing cancer activity.
Therefore, we started the patient on a three-month protocol consisting of hyperbaric oxygen therapy (HBOT) three times a week, intravenous vitamin C and dichloroacetate sodium (DCA) plus pulsed electromagnetic field therapy (PEMF) twice a week, and Light Beam Generator (LBG) and ozone therapy once a week. We also recommended four Supportive Oligonucleotide Therapy (SOT) treatments, spaced out several months apart, beginning in October 2016.
Although his PHI and CTC levels initially declined, by late 2016 his PHI spiked up to a very high 92.9 U/L, his CTC was 9.5, and his nagalase was elevated at 1.97 nmol/min/mg, so scans were ordered in December 2016. CT of the lungs was negative, but abdominal CT revealed two adjacent hypodense lesions in the left lobe of the liver measuring 10 mm and 11 mm, an increase from 3 mm each previously. A contrast-enhanced MRI of the abdomen was positive for two lesions on left hepatic lobe measuring 10.8 mm and 6.4 mm consistent with metastasis to liver. There were also several cystic lesions.
Following his diagnosis of metastatic melanoma, the patient resumed HBOT three times a week plus PEMF and IV therapies (vitamin C, DCA, poly MVA, selenium, and artesunate) twice a week. He also began weekly LBG and hyperthermia treatments twice a week and started taking metformin 500 mg twice a day. He had a second SOT treatment in March 2017. Abdominal MRI in April 2017 showed that the larger lesion had shrunk to 9.6 mm compared to the previous 10.8 mm, and the second lesion was stable at 6.4 mm. Small cystic lesions were noted, but no new lesions were present. MRI of the pelvis and CT of the chest were negative. CTC levels in April dropped to 7.9 cells/mL, and PHI was in the normal range at 30.7 U/L. Nagalase also declined to a high-normal level of 0.94 nmol/min/mg.
Over the next few months, the patient continued IV vitamin C plus IV selenium and artesunate weekly. He received his third SOT treatment in August 2017 and continued to do well. MRI that month showed further shrinkage of the two lesions to 4 mm and 6 mm, with small cystic lesions but nothing new. He had a fourth SOT treatment in January 2018 and HBOT two or three times a week. Blood tests in February 2018 revealed that his PHI had dropped to 31.5 U/L and his nagalase to 0.66 nmol/min/mg, both within the normal range. Abdominal MRI in April 2018 showed stable lesions measuring 4 mm and 6 mm with small cystic lesions and no new lesions.
We continued to follow the patient with regular treatments and blood tests throughout 2018. His CTC further declined to 7.0 cells/ml in June. PHI also gradually declined. Interestingly, when the patient decreased his treatments, his PHI crept up. When he resumed IVs and HBOT, it normalized. By December 2018, MRI of the abdomen showed further decrease in the two liver lesions, now measuring 2 mm and 4 mm with small cystic lesions that were unchanged.
We stepped up his IV therapies in 2019, and in June his PHI and nagalase levels were in the normal range at 28.1 U/L and 0.75 nmol/min/mg, respectively. MRI of the abdomen in June 2019 showed calcification of the liver lesions with no additional lesions except for the cystic lesions and no evidence of metastatic disease. MRI of the pelvis was also negative for metastasis. The patient’s stage 4 melanoma has been in remission since June 2019. Abdominal MRI with and without contrast in December 2019 noted the presence of tiny stable hepatic cysts and no evidence of abdominal neoplasm.
The patient returns for follow up with periodic testing and supportive treatments. His most recent CTC test was 5.2 cells/mL, a significant improvement from his initial 2016 test result of 9.3 cells/mL. His PHI levels have also been in the normal range except for a spike in January 2021, which rapidly returned to normal. This could be due to high levels of palladium, a toxic heavy metal that suppresses immune function. He has received multiple EDTA chelation treatments with significant improvements in previously high levels of lead, gadolinium, platinum, uranium, and other metals, and his palladium level is slowly decreasing.
Discussion
This patient has been in remission with stage 4 melanoma since June 2019. Initially diagnosed with stage 3 melanoma in June 2014, he was treated with surgical excision of lesions on his back and left shin plus removal of 12 lymph nodes. He had a normal PET scan in late 2015 with no further treatment recommendations.
After consulting us for monitoring in early 2016, we suspected a recurrence based on elevated PHI, CTC, and nagalase levels suggestive of tumor activity. We started him on a comprehensive treatment program consisting of HBOT, IV vitamin C and DCA, PEMF, LBG, and ozone therapy, with the later addition of SOT. An MRI in December 2016 confirmed recurrence, with metastasis to the liver (two lesions and multiple liver cysts) and a diagnosis of stage 4 melanoma.
Given that the patient’s recommended follow up by his oncologist was blood work every three to six months, it is possible that this recurrence would have gone unnoticed, had active cancer biomarkers not been detected by PHI, CTC, and nagalase tests. Early indications of cancer activity enabled us to begin treatment months before the December 2016 MRI confirmation of metastatic melanoma.
Over the next five years, we treated the patient with a comprehensive treatment program, making periodic additions and adjustments to include additional IV therapies (Poly MVA, selenium, curcumin, and artesunate), hyperthermia, nutritional support, and EDTA chelation. During that time, his PHI, CTC, and nagalase slowly returned to normal levels, indicative of a reduction in cancer activity. This mirrored findings on CT and MRI scans, as the two liver lesions slowly regressed from an initial 10.8 and 6.4 mm, to 2 and 4 mm a year later, and, in June 2019, to calcification of the two liver lesions, no additional lesions, and “no evidence of metastatic disease.”
This is a remarkable recovery, given the aggressiveness and mortality risk of metastatic melanoma. Over the past decade, significant progress has been made in the treatment of stage 4 melanoma, which historically had a five-year survival rate of less than 10%. Newer immunotherapy regimens, which help the patient’s immune system identify and fight cancer, are a promising and welcomed treatment option with lasting remission for some patients with advanced melanoma17. However, immunotherapy does not work for everyone, and many patients still face a challenging prognosis.
Nearly 1.9 million new cancer cases are predicted in the U.S. in 2021, along with an estimated 608,507 cancer deaths. Approximately 39% of Americans will be diagnosed with cancer of some kind during their lifetime18. The outcomes this patient and many other patients with a variety of cancers have experienced attest to the efficacy of these and other integrative cancer treatments—not only for melanoma but most types of cancers.
The underutilized cancer biomarkers (PHI, CTC, and nagalase) and integrative therapies we have presented merit broader use as well as future research, including randomized clinical trials, to elucidate their mode of action, safety, and ability to increase long-term survival.
Note: The patient has provided informed consent to use his information for educational purposes.
1. American Cancer Society. Key statistics for melanoma skin cancer. Available at: https://www.cancer.org/cancer/melanoma-skin-cancer/about/key-statistics.html. Accessed May 13, 2021.
2. National Cancer Institute. Cancer Stat Facts: Cancer of any site. Available at: https://seer.cancer.gov/statfacts/html/all.html. Accessed May 13, 2021.
3. American Cancer Society. Survival rates for melanoma skin cancer. Available at: https://www.cancer.org/cancer/melanoma-skin-cancer/detection-diagnosis-staging/survival-rates-for-melanoma-skin-cancer-by-stage.html. Accessed May 13, 2021.
4. Connealy, LE. Diagnostic tests for early detection of cancer: an integrative approach. Townsend Letter. 2020 Aug/Sept. Available at: https://www.townsendletter.com/article/445-6-early-cancer-detection-diagnostic-tests/ Accessed May 13, 2021.
5. Araki K, et al. Phosphoglucose isomerase/autocrine motility factor promotes melanoma cell migration through ERK activation dependent on autocrine production of interleukin-8. J Biol Chem. 2009 Nov 20;284(47):32305-11.
6. Alix-Panabieres C, et al. Detection of cancer metastasis: past, present and future. Clin Exp Metastasis. 2021 May 7.
7. Thyer L, et al. GC protein-derived macrophage-activating factor decreases α-N-acetylgalactosaminidase levels in advanced cancer patients. Oncoimmunology. 2013 Aug 1;2(8):e25769.
8. Nauman G, et al. Systematic Review of Intravenous Ascorbate in Cancer Clinical Trials. Antioxidants (Basel). 2018 Jul 12;7(7):89.
9.Tataranni T, Piccoli C. Dichloroacetate (DCA) and Cancer: An Overview towards Clinical Applications. Oxid Med Cell Longev. 2019 Nov 14;2019:8201079.
10. Augustin Y, Staines HM, Krishna S. Artemisinins as a novel anti-cancer therapy: Targeting a global cancer pandemic through drug repurposing. Pharmacol Ther. 2020;216:107706.
11. Jones MW, et al. Hyperbaric Physics. 2020 Oct 27. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan.
12. Vadalà M, et al. Mechanisms and therapeutic effectiveness of pulsed electromagnetic field therapy in oncology. Cancer Med. 2016 Nov;5(11):3128-3139.
13. Le BT, et al. Antisense Oligonucleotides Targeting Angiogenic Factors as Potential Cancer Therapeutics. Mol Ther Nucleic Acids. 2019 Mar 1;14:142-157.
14. Clavo B, et al. Ozone Therapy as Adjuvant for Cancer Treatment: Is Further Research Warranted? Evid Based Complement Alternat Med. 2018 Sep 9;2018:7931849.
15. Scutigliani EM, et al. Modulating the Heat Stress Response to Improve Hyperthermia-Based Anticancer Treatments. Cancers (Basel). 2021 Mar 12;13(6):1243.
16. Ferrero ME. Rationale for the Successful Management of EDTA Chelation Therapy in Human Burden by Toxic Metals. Biomed Res Int. 2016;2016:8274504.
17. Kuryk L, et al. From Conventional Therapies to Immunotherapy: Melanoma Treatment in Review. Cancers (Basel). 2020;12(10):3057.
18. National Cancer Institute. Cancer Stat Facts: Melanoma of the skin. Available at: https://seer.cancer.gov/statfacts/html/melan.html. Accessed May 13, 2021.
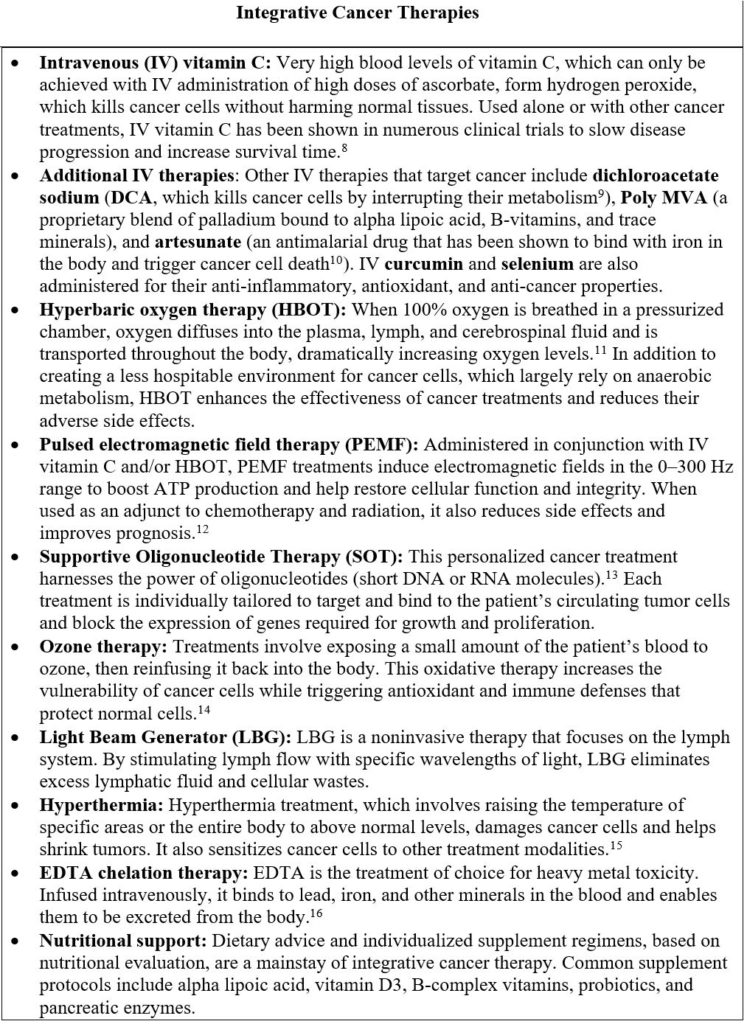
Integrative Cancer Therapies (Sidebar)
- Intravenous (IV) vitamin C: Very high blood levels of vitamin C, which can only be achieved with IV administration of high doses of ascorbate, form hydrogen peroxide, which kills cancer cells without harming normal tissues. Used alone or with other cancer treatments, IV vitamin C has been shown in numerous clinical trials to slow disease progression and increase survival time.8
- Additional IV therapies: Other IV therapies that target cancer include dichloroacetate sodium (DCA,which kills cancer cells by interrupting their metabolism9), Poly MVA (a proprietary blend of palladium bound to alpha lipoic acid, B-vitamins, and trace minerals), and artesunate (an antimalarial drug that has been shown to bind with iron in the body and trigger cancer cell death10). IV curcumin and selenium are also administered for their anti-inflammatory, antioxidant, and anti-cancer properties.
- Hyperbaric oxygen therapy (HBOT): When 100% oxygen is breathed in a pressurized chamber, oxygen diffuses into the plasma, lymph, and cerebrospinal fluid and is transported throughout the body, dramatically increasing oxygen levels.11 In addition to creating a less hospitable environment for cancer cells, which largely rely on anaerobic metabolism, HBOT enhances the effectiveness of cancer treatments and reduces their adverse side effects.
- Pulsed electromagnetic field therapy (PEMF): Administered in conjunction with IV vitamin C and/or HBOT, PEMF treatments induce electromagnetic fields in the 0–300 Hz range to boost ATP production and help restore cellular function and integrity. When used as an adjunct to chemotherapy and radiation, it also reduces side effects and improves prognosis.12
- Supportive Oligonucleotide Therapy (SOT): This personalized cancer treatment harnesses the power of oligonucleotides (short DNA or RNA molecules).13 Each treatment is individually tailored to target and bind to the patient’s circulating tumor cells and block the expression of genes required for growth and proliferation.
- Ozone therapy: Treatments involve exposing a small amount of the patient’s blood to ozone, then reinfusing it back into the body. This oxidative therapy increases the vulnerability of cancer cells while triggering antioxidant and immune defenses that protect normal cells.14
- Light Beam Generator (LBG): LBG is a noninvasive therapy that focuses on the lymph system. By stimulating lymph flow with specific wavelengths of light, LBG eliminates excess lymphatic fluid and cellular wastes.
- Hyperthermia: Hyperthermia treatment, which involves raising the temperature of specific areas or the entire body to above normal levels, damages cancer cells and helps shrink tumors. It also sensitizes cancer cells to other treatment modalities.15
- EDTA chelation therapy: EDTA is the treatment of choice for heavy metal toxicity. Infused intravenously, it binds to lead, iron, and other minerals in the blood and enables them to be excreted from the body.16
- Nutritional support: Dietary advice and individualized supplement regimens, based on nutritional evaluation, are a mainstay of integrative cancer therapy. Common supplement protocols include alpha lipoic acid, vitamin D3, B-complex vitamins, probiotics, and pancreatic enzymes.