By Trevor Cates, ND
While leaky gut is now a common term, leaky skin is worthy of attention, especially during these times of widespread use of hand sanitizers and increased hand washing. Leaky skin (the external epithelium) is connected to leaky gut (the internal epithelium). Often times, leaky gut first presents as skin issues, and the most common example of this in clinical practice is atopic dermatitis (AD).
In a healthy state, our skin provides protection, temperature regulation, and maintains hydration. It is constantly renewing and regenerating itself with epidermal turnover. Genetic, immunologic, microbial and mechanical factors contribute to skin barrier function. When the skin’s barrier is damaged or out of homeostasis, it no longer is able to function as designed, leading to leaky skin and appearance of a number of diseases, including acne, psoriasis, ichthyosis, and AD.
Leaky gut and leaky skin share some key similarities that impact overall health. Leaky skin is not as efficient as healthy skin at keeping allergens out, so they cross the epithelial barrier and trigger a systemic immune response.1 An impaired epidermal barrier also makes it more likely to absorb potentially hazardous chemicals, which might cause reactions in the skin (contact dermatitis) or systemic toxicity.2
Skin forms a protective barrier that limits external invasion and provides a natural habitat for a multitude of microbes (bacteria, fungi, viruses), called the skin microbiota. Microbes colonizing the skin support the skin’s barrier function. There is diminished bacterial diversity in AD and elevated amounts of Staphylococcus aureus (S. aureus) are detectable on AD skin, which negatively impacts the skin barrier function.3
The skin’s barrier function is dependent upon the structure and composition of the uppermost layer of the epidermis, the stratum corneum (SC). Lipid organization and lipid metabolism in the SC requires an acidic pH, and when this is out of balance it can contribute to the issues of skin barrier function seen in atopic dermatitis. And growth and virulence of S. aureus is pH dependent, which can further contribute to atopic dermatitis.4
Use of harsh alkaline detergents in skincare products may increase the skin’s natural pH and trigger inflammation.5 A leaky epidermal barrier, causing water loss from the skin and causing dry skin, further predisposes skin to microbial imbalances. Achieving a well-balanced skin microbiota protects skin from harmful pathogens and promotes the natural lipid barrier and skin’s immune system. Ultimately, this function helps prevent AD and other skin conditions.
Conventional treatments for AD often miss addressing the underlying causes, and overzealous hygiene routines worsen the issue. Antibiotic prescriptions are common in dermatology, and excessive use of antibiotics has created an emergence of “superbugs.”6 With a naturopathic approach to AD, we want to support a healthy microbiome and restore the skin’s hydration and pH to improve skin barrier function. The most effective approach occurs when we address these both internally and externally.
Internally
Improvements to the internal epithelium often lead to improvements on the external epithelium, so it’s important to address leaky gut. The supplement that I have been using in clinical practice for twenty years to help support my patients with leaky gut is GI Revive (Designs For Health), which contains a combination that includes L-glutamine, N-acetyl-D-glucosamine, aloe vera extract, deglycyrrhizinated licorice, slippery elm, mucin, chamomile, marshmallow, MSM, and quercetin. I have found using this along with certain probiotic supplements plus addressing food allergies and intolerances are fundamental in supporting patients with AD.
Of course, there is more to treating leaky gut, depending upon the patient’s individual needs. Testing can help determine specific dysbiosis issues, but overall probiotics have shown to be beneficial. Probiotics are known to enhance positive gut microbiota changes, and a great place to start is the diet, with fermented foods, such as kimchi, sauerkraut, pickled produce, yogurt, and kefir.7 Fiber-rich and prebiotic foods can help promote the growth of probiotics—dandelion greens, garlic, onions, leeks, and chicory.

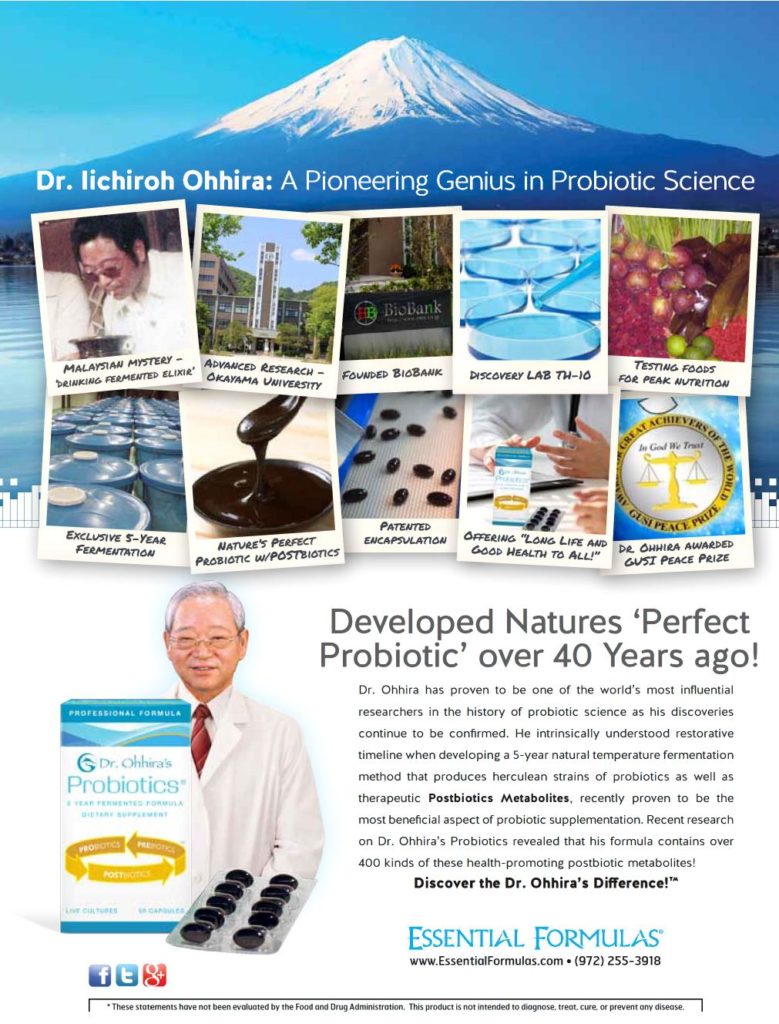
Probiotic supplementation has been shown to help prevent and treat AD.8 In the research, species of Lactobacillus and Bifidobacterium are the probiotics showing the highest potential for the treatment of AD.9 It is important to consider the strength, quality, and duration of probiotic supplementation and that an individualized approach works best.
Other supplements I often recommend to patients with AD that are also supported by the research include vitamin D3 and vitamin E. Vitamin D deficiency appears to be related to the severity of AD.10 Vitamin E of up to 600 IU daily has been shown to be an effective adjunctive treatment for AD.11
Externally
With AD comes an impaired barrier and inflammation of the skin plus an increase in the pH of the epidermal surface. This elevated pH further triggers inflammatory cytokines and comprises the barrier function and increases the chances of infection. The mildly acidic normal SC (4.5–5) inhibits the growth of S. aureus and Streptococcus pyogenes, so that the normal flora can thrive, like Staphylococcus epidermidis and Corynebacterium.12 So, the pH of routine skincare products as well as topical treatments should be in this 4.5 to 5 pH range. If you do not know the pH of a product, it can easily be tested with pH strips (unless it is 100% oil).
Restoring optimal pH helps support the skin’s hydration. In addition, certain topical ingredients can help restore water loss. However, common moisturizers are known to worsen AD since the skin barrier is already compromised, and with leaky skin it is important to avoid toxic chemicals that can more easily find their way into the bloodstream.
What is applied to the skin can impact the skin microbiota, which is essential in addressing AD. Topicals commonly known to create imbalances include antibiotics and antimicrobial ingredients like triclosan. Occlusives (such as dimethicone, petrolatum or lanolin) are commonly used in AD, but since they are trapping moisture in, they do not allow the skin to breathe. The concern is that when moisture is trapped in, especially when the person perspires, it can potentially disrupt the skin microbiota.