…article continued:
Perry Perretz, DO: A patient in my practice was infected with Chikungunya virus that presented as a painful frozen left shoulder. It persisted weeks longer than would be expected from such an infection. This was relieved with a combination of local procaine injection to the site of the bite, and a “segmental” injection over the C6 nerve root.
Another patient had erroneously been diagnosed with rheumatoid arthritis, despite negative CCP and RF labs. He had swelling of knees, ankles, elbows, and wrists that added almost fifty pounds of weight to his body. An interference field in a root canal tooth was identified. I considered giving him a diagnostic injection of procaine to determine its importance, but he was already motivated to get rid of the tooth. Once the tooth was extracted his rheumatoid symptoms disappeared overnight, and he lost almost forty pounds within the week.
Emotions create powerful interference fields. In the October 2017 issue of the Townsend Letter, our colleague Michael Gurevich, MD, wrote an excellent article on the use of neural therapy in psychiatry. Clearly, we have begun to understand more about the effects of trauma upon the central nervous system. Other avenues of study have helped us understand more about post-traumatic stress and the induction of autonomic responses that are triggered by the engagement of a traumatic memory.
Jeff Harris, ND: I have worked with many soldiers who have had very severe pain and PTSD. Their pain medications weren’t helping. They were losing their relationships, or already had lost them. They hadn’t been able to sleep for days on end and they were desperate for help, knowing that many of their friends in the same situation had committed suicide. At first, I was nervous to treat them, but neural therapy has been almost magical for them. The very first one I saw had a bomb go off right in front of him while wearing an ordinance disposal suit. He was a star on a military athletic team, a family man with children. He suffered with chest pain and high blood pressure. I first treated the circumference of his head and the area over the left side of his chest, where most of the explosive impact had been absorbed. Immediately following this treatment, he asked if he could leave the office to sleep in his truck. I asked him to come back before he drove off so I could evaluate him. Four hours later, he came back and hugged me! He hadn’t slept for many days before, but he reported that he felt normal for the first time since the explosion. More importantly, he had hope for his future. He has seen me a number of times over the last few years, as he has needed additional treatment, but he says that the PTSD and pain have never returned to the level he felt prior to our first office visit. He has told his medical team on the military base about the treatments he received. He asked them to have me come and talk with them, but so far, they haven’t invited me.
COVID-19 and the “Long-Haulers”
Extreme stress can bring back the memory of trauma. The COVID-19 pandemic represents just such a trauma for some of those who have been infected. As this is a novel coronavirus, we are still struggling to understand the severity of its course for many different populations. We know that it is extremely contagious and that no one is naturally immune. Those infected have been forced to confront their diagnoses much the same as any terminally ill patient. Is this going to kill me? How badly will I suffer? Do I need to say good-bye to my kids? Change my will? Change my medical directives? Will I die alone? There is a subset of COVID-19 survivors who have endured the acute infection, only to find themselves exhibiting symptoms far beyond their “recovery.” They are referred to as “long-haulers.”
Perretz: Recently, I evaluated a long-hauler, infected in March 2020, still suffering symptoms of her viral illness in July, though she had tested negative since April. Her symptoms were pain, heaviness, and tightness in the chest, shortness of breath, and heart palpitations. X-rays, ECG, and labs were all negative. Surgical history included appendectomy, C-section, and breast implants. On physical exam, the lung reflexes were dysfunctional bilaterally, and the heart rhythm reflex was found to be positive. There were trigger points in the bilateral infraspinatus muscles known as the Infraspinatus Respiratory Reflex (IRR), the discovery of which is attributed to the late Dr. Henry Philibert, MD. Scars, in this situation, were not found to be neurologically active. Treatment was delivered with intradermal injections of procaine to the acupuncture points, Lung 1, bilaterally, CV15, for the heart reflex, and Governing Vessel 18. The IRR was injected with procaine, and a touch of Kenalog to increase respiratory ease. Osteopathic manipulation was employed to release the ribs, which had been restricted by coughing. Emotional Freedom Technique was also employed to address trauma. Immediate ease came to her breathing, and by the next day she was symptom-free.
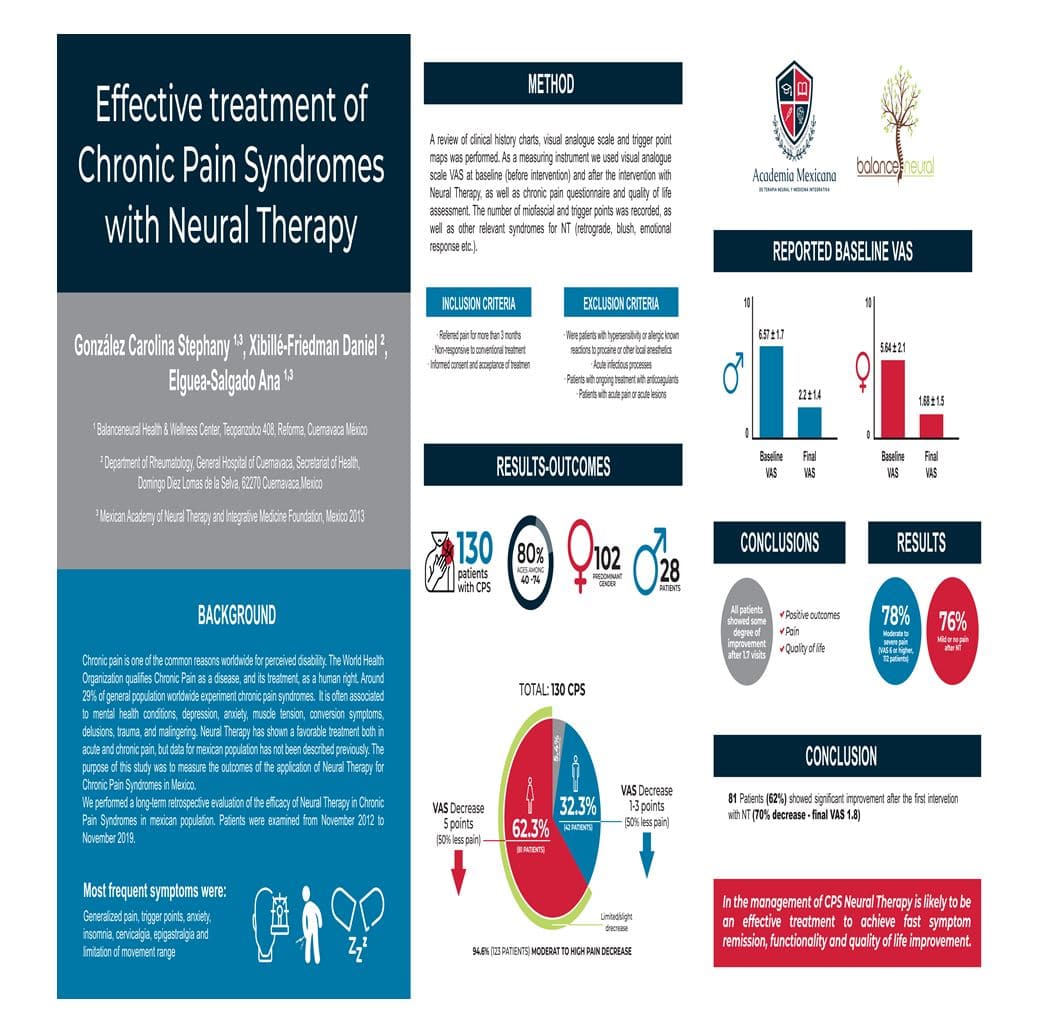
Our colleague, Dr. Stephany Gonzalez, performed a seven-year (2012-2019) retrospective evaluation of neural therapy’s efficacy for chronic pain syndromes in 130 patients. All patients in the study reported pain greater than three months’ duration that had failed to respond to conventional treatment.
Results showed that ALL patients receiving neural therapy treatment reported some improvement after an average of 1.7 visits. Ninety-four point six percent (94.6%) reported decreases in pain by Visual Analog Scale. Sixty-two point three percent (62.3%)reported VAS decreases of 5 levels, or greater. In total, 76% of surveyed patients achieved remission or near-remission of chronic pain with neural therapy treatment.
In summary, neural therapy’s chief application has come as a treatment for chronic pain and illness, and one of its greatest values is that it represents a comprehensive approach to physiology, avoiding some of the reductionistic traps of Western diagnosis. An aspect of its attractiveness is that it can be appreciated by professionals from a wide range of trainings, and it provides the perfect blend of Eastern and Western medicine. A typical Western-trained medical doctor can easily understand the use of anesthetics to neutralize dysfunctions of the autonomic nervous system, but might be surprised at how the application of this model tends to “teach” us how a patient compensates, as an individual, to the experiences of life. A naturopath might be excited to exploit neural therapy’s ability to determine root causes of illness and pain and treat them using the least possible force. An acupuncturist might see neural therapy as a form of medically applied acupuncture, and the dentists will be pleased to see how neural therapy recognizes the influence of the teeth and oral cavity on the health of the entire individual.
Neural therapy is practiced more in Europe and South America than in North America, but it is gaining traction here. Much of the earlier literature is in German, but translations in English and Spanish have been available for years now. Many of us in North America owe a great debt to Dr. Dietrich Klinghardt for his teaching. Within the last three years, a North American Academy of Neural Therapy has been created to encourage leadership and training for professionals of various disciplines. Membership and continuing education opportunities are available through its website, www.NAANT.org.
Resources
Klinghardt DK. Neural Therapy. J Neurol Orthop Med Surg. 1993;14: 109-114.
Kidd RF. Neural Therapy: Applied Neurophysiology and Other Topics. Renfrew, Ontario, K7V 1T6. Self-published rfkidd@onn.aib.com 2005.
Gurevich M. Innovative Approach to Psychiatry: Treating Incurable Psychiatric Patients with neural Therapy. Townsend Letter. October 2017; pp 51-54.
Gonzalez CS, et al. Effective Treatment of Chronic Pain Syndromes Using Neural Therapy. Poster presentation at First Congress of the North American Academy of Neural Therapy, Orlando, FL; Feb 27-Mar 1, 2020.






