By Carolyn McMakin, MA, DC
When they arrive in your office, they all look the same with minor variations, rather like identical suburban tract houses with different floor plans and exterior colors.
They have body pain that varies between a 4-5/10 and a 6-8/10. They don’t sleep. They report being fatigued and depressed and say that walking down the soap aisle in the grocery store or standing next to someone who wears perfume gives them a headache or makes them sick for days. They seem to react to so many foods and are allergic to everything. Medications might reduce the pain a little and create side effects like fatigue and slow thinking, but it’s all their doctor can do.
It doesn’t matter how many doctors of what type they have seen, they get one or more of these diagnoses: fibromyalgia, chronic fatigue, multiple chemical sensitivities and recently they are often told they have mast cell activation syndrome (MCAS) or small intestine bacterial overgrowth (SIBO), gastroparesis, leaky gut, mold toxins, Epstein-Barr (EBV) or maybe Lyme (even though the Lyme tests have been negative or show only 1 band). Or they are told they really just have depression even though they are already on an antidepressant and they are prescribed an additional antidepressant or a stronger dose of the one they are already on. Or, worse yet, they are put on a “mood stabilizer” that turns out to be an “atypical antipsychotic” with severe long-term side effects we won’t have time to cover in this article.
In general, no one asks them, “What happened immediately before the onset?” If the answer is, “Nothing happened, it just started,” the doctor usually moves on to the next questions instead of drilling deeper. If the patient is lucky, the next question might be, “When was the last time you felt well?” And the answer is often, “I’ve always been sick. I think I’ve been like this since childhood.” The next question should be but isn’t usually, “What did you do for fun in grade school or high school?” That answer is often, “I played soccer, rode horses or did gymnastics or theater.” Replies the doctor, “So up until that year you were fine. Then what? When exactly did the symptoms get this bad?” After that the answers might be relevant. But few doctors ask the set of questions that should come next.
My entire practice since 1998 has been the 10% of patients no one else could help, and I failed a number of them myself. But eventually through trial and error and being sick and recovering myself through the help of brilliant colleagues, I learned what I am about to tell you in this article.
In general, there is either the most basic medical blood work ordered, which will turn out normal or there may be up to $3,000 to $4,000 worth of exotic complex blood work ordered, which will show all sorts of items out of range. But the exotic blood work doesn’t ever say how the analysis is done, where and on whom the normal levels were determined or published and gives very little guidance about what to do to correct the abnormal results. Patients either leave with a prescription for something that might not help much or $500-$1,000 worth of supplements to take three to four times a day that might help in a few months after they have been on an incredibly restrictive diet.
If they look on the internet, they will be even more frightened and hopeless but will feel, at least, that there are many other people who have what they have so they know now that they are not crazy. And then they come to you, for one last chance, that you might be able to help.
If you’re like most practitioners, you swallow the rising panic and desperation and apply the latest thing you read or the technique you’ve learned that helps most patients and hope it will help this patient.
If you’re the patient, you hope that this person might be the one with a solution to this thing that has made your life miserable for the last two, five, 10, or 20 years. You hope that the little glimmer of hope you have will turn desperation into a solution that makes the trip and the office visit worthwhile as you tell the story for the tenth time to the tenth doctor.
And, the truth of the matter that gives rise to this unified theory, is that these conditions and these symptoms have one thing in common that no one thinks of because they don’t have a way to treat that one thing. I propose that this thing they all have in common is the vagus nerve through its role of suppressing the immune system, regulating gut motility and gut pH and therefore gut bacterial flora, and the connection of the vagus to the brain and limbic system. Once you have a way to treat the vagus fairly quickly and you can see the results and improvement fairly quickly, then the connections begin to be obvious and the patients improve.
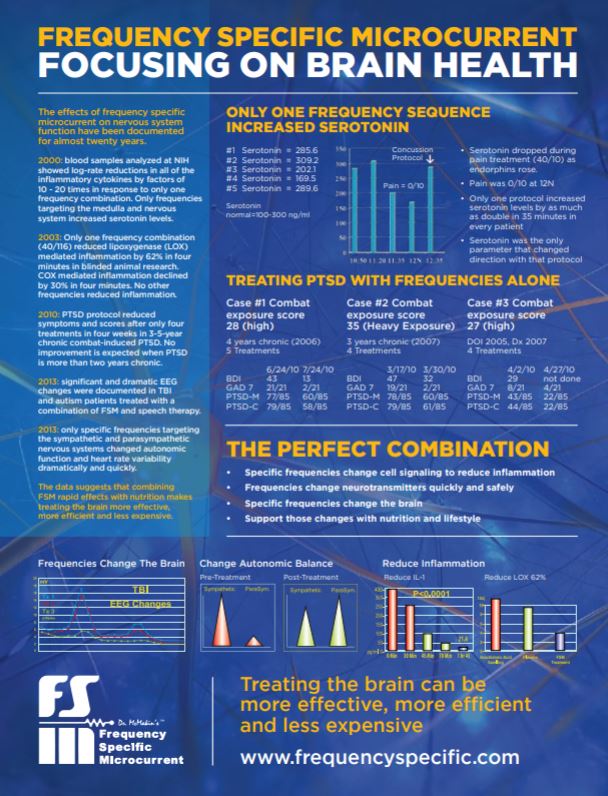
It should be said up front that I developed Frequency Specific Microcurrent™ (FSM) in 1996, and FSM is what I add to treat all of these patients as an adjunct to what most practitioners already do. It has to be said that I don’t know how I would treat any of these conditions without FSM, so this article can only tell you the unified theory based on treatment experience; it won’t teach you how to use FSM, but it might give you a reason to look into it. It is hoped that the theory will be interesting whether FSM appeals to you or not.
Fibromyalgia (FMS) is a neuroendocrine condition characterized by chronic full body pain in all four quadrants, chronic non-restorative sleep, and central pain sensitization lasting more than three months. Fibromyalgia patients have reduced levels of growth hormone due to reduced levels of growth hormone releasing hormone (GHRH) in the brain and loss of stage 4 sleep during which 85% of growth hormone is generated. Growth hormone in an adult facilitates transport of amino acids into muscle cells for repair. Fibromyalgia patients do not tolerate exercise because they don’t have enough growth hormone and can’t repair the normal wear and tear produced by even minor exercise. They have reduced levels of branch chain amino acids, and there are consistent hormone and neurotransmitter abnormalities across all fibromyalgia patients no matter what caused the fibromyalgia.1-7
After treating over 500 fibromyalgia patients in 23 years, it has become obvious that there are at least five different and distinct causes of fibromyalgia. The literature says that 27% of cases are caused by physical trauma. Clinical experience puts that number at closer to 40%. The other causes are organic chemical exposure, severe prolonged stress, viral illness, and there is a genetic type characterized by genetic defects in the serotonin pathways that affect pain processing or genetic defects in other neuroendocrine pathways. Fibromyalgia may start from any one or from a combination of these causes. Regardless of how they start out, fibromyalgia patients end up looking like the patient described in the first section of this article.8-13
Chronic fatigue syndrome (CFS) is distinct from fibromyalgia although both diagnoses are sometimes used as a garbage-can diagnosis by many of the physicians who treat these patients. Chronic fatigue is associated with a positive Epstein-Barr titer and tender lymph nodes suggesting some infectious influence. Some researchers question whether EBV causes CFS or is opportunistic. There is some support for the idea that CFS is an advanced form or variant of fibromyalgia but that is not well accepted. In CFS, fatigue and cognitive problems are the overwhelming complaints, along with non-exudative pharyngitis, swollen cervical lymph nodes and low-grade fever. In one study substance P was not elevated in the spinal fluid of CFS patients whereas it is generally elevated in fibromyalgia patients.14-17
Multiple chemical sensitivities (MCS) is a controversial diagnosis unless you are the patient who has it. The medical community is still trying to decide whether it is a clinical diagnosis or not. Many in the medical community consider MCS symptoms to be a physical manifestation of psychiatric illness rather than a primary medical illness. This attitude prevailed towards fibromyalgia for many years until there was finally enough research to demonstrate consistent physiological abnormalities among fibromyalgia patients. There are those in the medical community and patient advocate groups who agree that multiple chemical sensitivity is a negative physical reaction to certain chemicals. Which patients have which symptoms may depend on individual genetic variants in individual liver detoxification pathways and neurochemical and metabolic pathways. There is still debate as to whether multiple chemical sensitivity can be a diagnostic illness on its own.
The most common symptoms of multiple chemical sensitivity may include headaches, rashes, asthma, muscle and joint aches, body pain, fatigue, memory loss, and confusion exacerbated by exposure to specific organic chemicals, fragrances or volatile organic chemicals (VOCs) that outgas off of carpets, synthetic fibers or paints. Each patient experiences symptoms differently, which may be why the medical community has difficulty deciding that this is one diagnosis.18
A Unified Hypothesis for these three conditions isn’t meant to suggest that they are the same thing; this hypothesis suggests that the vagus nerve plays a role in the cause and perpetuation of the symptoms in these conditions.
…Article continues on next page.