…article continues:
TGF-beta is a protein that regulates cell differentiation, proliferation, and apoptosis (cell death); it is also an indicator of prolonged inflammation.
MMP-9 is involved in allergic and non-allergic inflammatory response. When MMP-9 is in balance, it aids in regeneration and remodeling of tissue. However, when it is out of balance it sets up an inflammatory cascade of cytokines and chemokines. Those tissues then have higher levels of histamine, which is why MMP-9 is also used to evaluate MCAS.
MSH is a hormone called a neuropeptide that controls other hormones, as well as immune response and inflammation. MSH is typically low in biotoxin illness, which means it can’t have its normal control on inflammation. Without sufficient MSH, individuals are more susceptible to sleep issues and chronic pain due to reduced endorphin production.
VIP is a neuro-regulatory hormone that regulates peripheral cytokine responses and inflammation in the body. If we don’t have sufficient VIP, we cannot adequately regulate inflammation in the body.
HLA-DR genes. Looking at certain genotypes can help emphasize an individual’s susceptibilities. According to Dr. Shoemaker’s work, approximately 26% of the population are genetically susceptible to mold toxin illness.2
VCS test is not a lab test as much as a self-guided assessment that one can take online. The Visual Contrast Sensitivity test is a reflection of neurological function and the potential damage that biotoxins have done to neurons.
NeuroQuant EEG. I have very limited personal experience with NeuroQuant EEG, however, it may be a useful tool in distinguishing the impact of Lyme versus mold on the human brain. The challenges of this modality are cost, access, and accurate interpretation.
CD-57. I include this in the “indicators” category. CD-57 is a cluster designation marker that is theorized to be suppressed in chronic Lyme patients. I do measure it as a guide; however, it is not a marker that I lean heavily on as I have concerns about reliability of the test.
Level Three: Getting Specific
Here is where the rubber hits the road, and where I put most of my focus with my chronic, complex patients in assessing the underlying causes of their health issues.
While general/basic markers of health are important to have and while the indicators listed above can provide helpful information, I am a firm believer in being as specific as possible in testing. Therefore, the following tests are the ones I choose as a priority in assessing my patients.
Mycotoxins. For assessing mycotoxins, I am a big fan of doing a direct urine mycotoxin test. If mycotoxins measure high in the urine, the patient has mycotoxins. To me it’s simple, its direct, and its quantifiable. It’s not perfect, of course, if a patient doesn’t detoxify well, the output may not be truly representative of their body stores, but it’s good enough in my opinion to be the most useful assessment for mycotoxins.
Now there are many questions that come from a positive result. Where did this exposure come from? Are they still being exposed? Have they had their current home or workplace evaluated? Do they need to move? Do they need to throw away all their belongings? The rabbit hole of mold illness is deep and difficult to navigate.
I mostly use Great Plains Laboratory’s urine mycotox panel. I was always happy with Real Time Labs, but the price point made it prohibitive for many patients. Great Plains Lab has always offered great testing at a reasonable price, and their panel has made mycotoxin testing possible for many of my patients.
I am grateful to Neil Nathan and his book Toxic3 for his suggestion to provoke the urine mycotoxin test. He suggests using glutathione 500 mg twice daily for a week before (if the detoxification effect of this is too strong, patients can stop taking the glutathione and do the collection the following day) or use an infra-red sauna prior to collection.
I do think that MARCONS testing is valuable here too. Aligned with the work of Dr. Brewer and Dr. Nathan, I am seeing the significance of mold and fungal colonization in the sinuses and have responded by using more nystatin and amphotericin B nasal spray, both with EDTA to help break down biofilm. If a MARCONS swab comes back positive, then I would start with BEG spray to try to eradicate bacterial infection before moving on to antifungals, then move on from there to VIP spray, which is more for neurological healing rather than being antifungal or bacterial. If MARCONS negative I move directly to nystatin/amphotericin B with EDTA as a starting point.
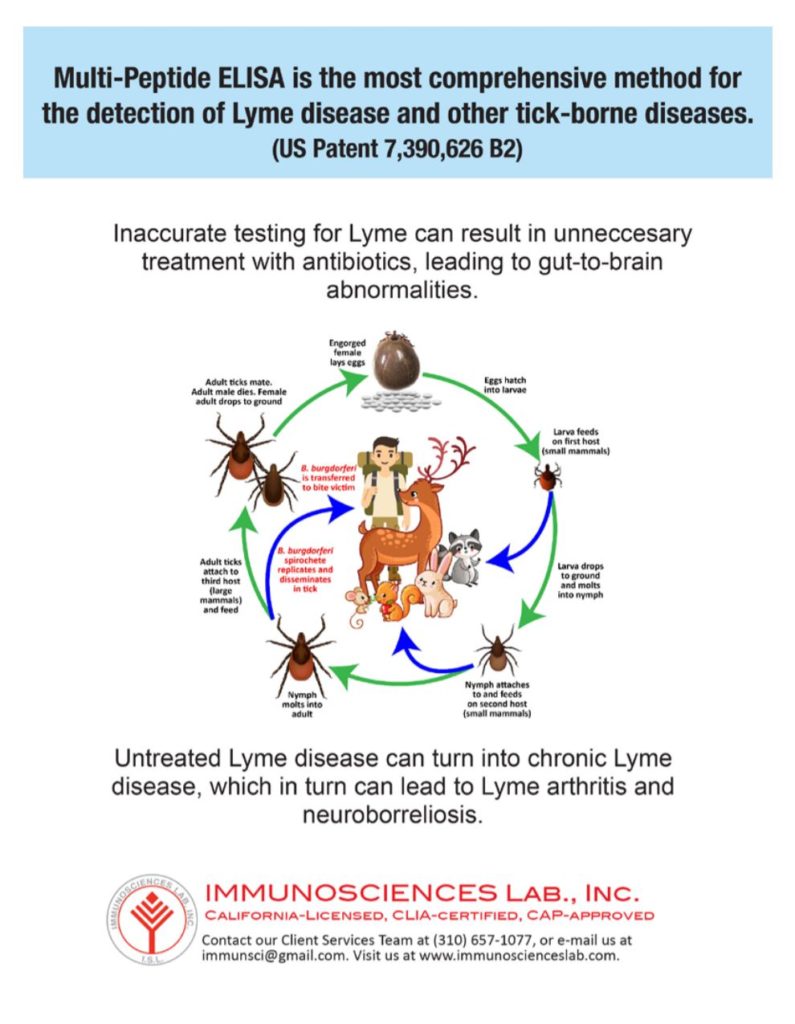
Lyme disease. In my opinion, IGeneX is still the gold-standard for Lyme testing, and I utilize their testing extensively. I believe it’s just as important to assess co-infections as Borreliosis itself, so I recommend that patients get a panel that at least includes the Borrelia IFA, and IgM and IgG Immunoblots, plus testing for tick-borne relapsing fever. I have seen several cases now where the Borrelia Western blots came back negative, but the tick-borne relapsing fever came back positive, so I am appreciating the expansion in strains of Borrelia testing that are becoming available to us.
From a co-infection standpoint, Babesia and Bartonella have always been the ones I’ve kept the closest watch on, mostly because Ehrlichia and Rickettsia tends to respond to the same treatments as the Borrelia itself. Bartonella is a bacterium, as is Borrelia, however its treatment path is fairly distinct. Babesia, being a protozoon, requires a different set of medications and herbs altogether. For that reason, these two are highest on my radar.
Personally, I opt for the antibody tests and the FISH tests for co-infections. As with the Lyme panels, I never felt the PCR tests were sensitive enough to warrant the extra expense.
When urine PCR testing became available, it appeared to be a good, cost-effective, comprehensive option to cover Borrelia and co-infections. I have had some concerns about sensitivity of the test but I will run it in conjunction with IGeneX Borreliosis testing as a more cost-effective option than the full Lyme/co-infection panel.
For new patients, I still tend towards the IGeneX panels using IFA and Western blots. If finances are limited, I might choose the Lyme/TBRF panel 1 (LTP1), along with the new urine PCR panel (TBD7). If finances are not a major consideration, I’ll opt for the tick-borne disease panel 1 (TBD1), as well as the urine PCR just to utilize the different types of testing to maximize the chance of getting helpful information.
Where I think the urine PCR testing is also useful is in evaluating a patient who is nearing the end of treatment. For some, Western blots were always negative or indeterminate at best, so when we go to repeat them during or at the end of treatment, what change are we expecting to see?
If we have high antibody responses on the IFA test, multiple bands on Western blot, positive antibodies for co-infections…they can all be repeated and see change. But what about the many people who had “meh” test results. Is there a point in repeating an indeterminate IgM Western blot? What “before” and “after” are we hoping to achieve? And if IgG is positive to start, can we expect that to turn to negative, or not, since memory cells may stay active for a decade to a previous infection?
Here is where I think the urine PCR testing has a place. If PCR positive, then we know there is some level of ongoing infection. If negative, it doesn’t guarantee it, but it’s a good sign.
The bottom line is, I order Lyme/co-infection testing to try to clarify the chronic infection situation. IGeneX is still my preferred lab, and I will order a combination of blood and urine testing, depending on the patient and their needs. Coupled with the urine mycotoxin panel from Great Plains, that to me offers the most succinct way to evaluate those two issues.
Implications for Treating Lyme/Mold-Related Illness
I am a proponent of trying to be as specific as possible in the testing we do, to identify as clearly as possible the role of Lyme versus mold in a patient’s situation. Obviously, each one is going to have its own specifics of treatment, however, I thought it might be helpful to highlight some of the commonalities between the two. For people dealing with both issues, this may help to feel less overwhelmed and more streamlined in their approach. For this conversation, let’s think about Lyme and mold toxicity both as biotoxin illnesses that trigger massive immune reactions, that then trigger systemic inflammation and chemical mediators of inflammation, including cytokines and chemokines.
Article continues… Click here for Page 3: Conclusion and REFERENCES