By Dr. Trevor Cates
Skin is the body’s largest organ; and although it is superficial, it is very revealing about overall health. We see that every day in our patients, such as dark under eye circles (allergies), dry lips (dehydration), dry skin (hypothyroidism), yellow skin (jaundice), cold sores (herpes), butterfly rash (lupus), facial hair in women (PCOS), acne along the jawline (hormonal imbalance), keratosis pilaris (nutritional deficiencies), and those are just a few. As practitioners, the clues that show up on our patients’ skin are valuable pieces for solving the mystery of their dis-eased state.
It is also a protective instinct for others to know the state of individuals’ health by looking at their skin. People that are acutely sick have facial cues, including on the skin, that warn others of the potentially contagious illness. “Stay away!” the ill person’s skin is telling others. This comes in handy when we want to avoid catching colds and the flu. But, with chronic skin issues, the patient with the skin problem suffers not only physically but often emotionally as well from rejection.
People with chronic dermatologic conditions, such as acne, eczema, rosacea, vitiligo, and psoriasis are often looked at differently; and it often impacts them emotionally. I have my own personal story of my childhood struggles with eczema, hives, and mysterious bumps that would appear on my face; kids would pick on me at school. I hid and stayed home as much as I could. Conventional approaches, including antihistamines, corticosteroids, and antibiotics only made me feel worse with allergic reactions and adverse reactions. Thankfully, in my case, what seemed like a curse at the time, turned into a blessing because holistic medicine is what turned my health around, eventually leading me to naturopathic medical school—and, later, to focus on naturopathic dermatology.
I share all this because, if you have not struggled with dermatologic issues, then you may not be aware of how emotionally upset your patients may be about their skin problems and how desperate they are to recover from them. While you are helping them physically, please also provide or refer for emotional support. And, know that they are likely to seek you out because they are distressed and looking for answers not to suppress but to address their skin.
You will continue to see more and more patients with chronic dermatologic conditions show up in your practice. Globally, the United States has the largest market for dermatology and GMR Data forecasts $12.3 billion in 2018, growing to $22.6 billion in 2028.1 One of the reasons for this rise is due to an increase in dermatologic conditions such as acne, skin cancers, atopic dermatitis, and skin infections.
Atopic dermatitis affects one in ten people during their lifetime.2 Rosacea affects 16 million Americans.3 Around 7.5 million people in the United States have psoriasis.4 But, the one we typically see the most in clinical practice is acne. After all, it is the most common skin condition in the United States, impacting over 50 million Americans annually.5 Although the majority of people with acne (approximately 85%) are between the ages of 12 and 24,6 adult acne is increasing, affecting around 15 percent of women.7
The American Academy of Dermatology states, “There is not enough data to recommend dietary changes for acne patients.” Instead, the Academy says, the “recommended treatments include topical therapy, antibiotics, isotretinoin, and oral contraceptives.” While that is currently their stance, there are many of us practicing a more integrative approach and finding excellent results.
Many soaps, skincare products, and topical medications
have a pH that disrupts the skin microbiota.
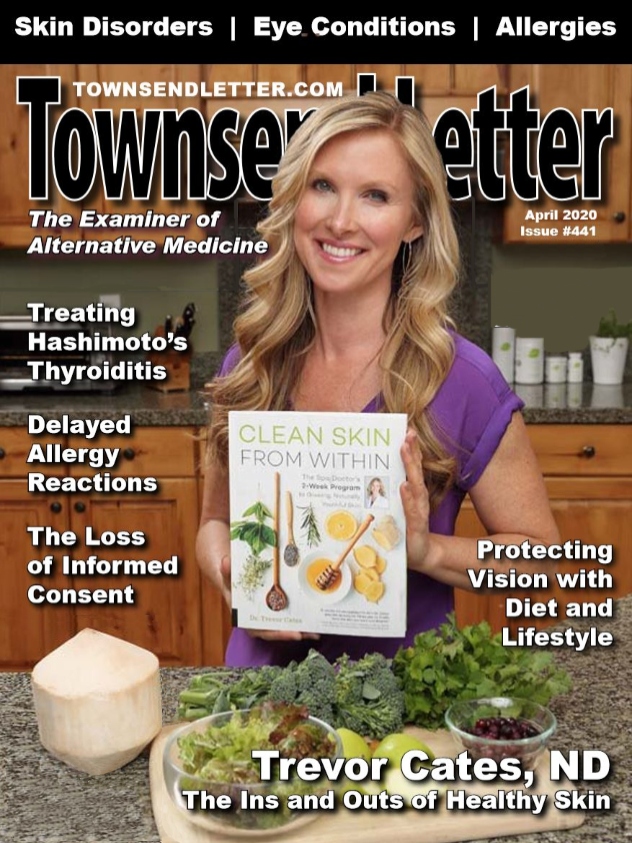
In my book Clean Skin from Within, I discuss six main underlying causes that can lead to chronic skin issues: inflammation, microbiome disturbance, oxidative damage, blood sugar issues, nutritional deficiencies, and hormonal imbalances
These root causes probably do not surprise you because they are common to many chronic health problems. Performing a thorough history, lab testing, and physical exam helps unveil the root causes. When it comes to treating my patients with dermatologic conditions, I have seen certain patterns that have led me to focus on these six root causes with my patients.
While addressing root causes is no secret in the naturopathic and functional medicine world, the key is to address them both internally and externally. While dermatologists may rely heavily on topical treatments and estheticians focus on facials, naturopathic physicians and functional medicine practitioners often focus on the internal treatments (diet, supplements, BHT, etc.). However, greater success with dermatologic conditions comes when you come from both angles.
For the first fifteen years of my practice, I too focused on addressing the root causes internally. My patients would get sixty to eighty percent better, but then the improvements would stop. Around that time, my patients kept asking me why when they switched to natural skincare (which they were doing because I wanted them to avoid exposure to toxic ingredients) that their skin did not look as good. So, I asked my dermatologist and esthetician friends for recommendations on effective natural skincare products, but they replied that I had to choose between natural or effective and that the combination did not exist.
This answer was not sufficient for me because of my experience, personally and with my patients, with the healing powers of nature. So, I dug into the research to see what might be missing in the natural skincare products my patients were using. That is when I learned more about the skin microbiome and what helps it flourish not only internally but also externally.
Human skin is inhabited by approximately one million bacteria/cm,8 and the microbiota varies around different areas of the body as well as amongst different individuals. Lifestyle, environment, hygiene, diet, age, and sex all greatly impact the makeup of the skin microbiome.9 With unhealthy lifestyle choices, overuse of antibiotics, and overzealous hygiene practices over the years, it should not be a surprise that we are seeing these higher rates of acne, atopic dermatitis, and other inflammatory skin disorders.
Many of the microbiome studies to date have focused on describing the gut microbiota, but the skin microbiota has been gaining more attention over the past 10 years. The gut and skin are both densely vascularized and richly innervated organs. They have important immune and neuroendocrine roles and are significantly related. A healthy gut microbiome protects the gut lining, increases the body’s ability to absorb nutrients, and protects against microorganisms that affect healthy skin. It is important to promote the skin microbiome from the inside out (via the gut) with diet.10
Achieving a well-balanced skin microbiota protects skin from harmful pathogens and promotes the natural lipid barrier and skin immune system. Ultimately, this function helps prevent acne, atopic dermatitis, and other skin eruptions. We can do that both internally through diet and supplements, such as probiotics, and also topically. Part of that ties into creating an ideal environment for skin microbiota diversity. Superficially, an important factor in supporting the skin microbiota involves the pH of the skin. The external pH of human skin has a natural pH level of about 4.5 pH.11
This mildly acidic environment helps keep the skin’s microbiota in balance. On the other hand, a more alkaline pH (around 8 to 9), can disrupt the microbiota. Many common skincare products, including soaps, cleansers, masks, moisturizers, and OTC topical medications, have a pH of 5.5 and higher, which can make the skin more prone to infections and premature aging.12 Ideally, skincare products and topical treatments should be in the 4.5-5.0 pH range to support healthy skin microbiota diversity.
When you create a healthy place for the skin microbiota to thrive, it also helps address other root causes externally, such as inflammation and oxidative damage. In addition to supporting the ideal pH for skin, it is important to protect the skin’s barrier function by using topicals with natural humectants and emollients. And, use caution with occlusive ingredients since they may further disrupt the skin microbiota.
So, bringing it all together, we want to address root causes with a healthy diet, individualized supplements, and other key aspects of an integrative approach. To help demonstrate how to tie it together, here is a patient with acne and the course of her treatment.
Acne Case
This 24-year-old female came in to see me with acne vulgaris on her face and back, hypothyroidism, and dysmenorrhea. The onset of her acne started at 12 years old. At that time, she saw a dermatologist who prescribed topical retinoid and oral antibiotics. She also used a well-known MLM acne skincare line. This helped some; but, in high school, she developed cystic acne and then scarring.
At the time of her appointment, she was taking Armour Thyroid medication for hypothyroidism, her skin was oily, and she was still breaking out in acne on her face and back. For skincare, she was using a popular cleanser from the health food store plus a natural body scrub.
At this initial appointment, I ordered lab work and put her on an oral probiotic, chaste tree berry, EPO, and a supplement with skin, hair, and nails nutritional support (containing a blend of nutrients, including vitamin A, B vitamins, zinc, MSM, and green tea extract). I also counseled her on avoiding trigger foods, including sugar and dairy, and how to increase her intake of fiber, healthy fats, protein, and phytonutrients.
After one month, looking at her lab results, I switched her thyroid medication to WP Thyroid and lowered the dosage, and added vitamin D3 (5000 IU) to her supplement regime. Topically, I recommended African Black Soap (liquid soap) for her back and recommended she remain on her supplements. (Note: African Black Soap is known for its pore cleansing and natural exfoliating effects. I prefer liquid soaps over bar soaps due to the fact that bar soaps, by the nature of how they’re made, have a higher pH that is not ideal for healthy skin.)
The following month, she mentioned her skin was less oily since starting the new thyroid prescription, but the cystic acne continued. Besides her skin, her menses were no longer painful, and her fatigue had diminished. At this appointment, she mentioned she was using a clarisonic skin brush for her face with a cleanser from her local health food store and a DIY mask made with apple cider vinegar and clay. Due to the fact that facial brushes can be too abrasive and over-exfoliating for compromised skin, I suggested she stop using the clarisonic brush. And, because I was concerned the DIY mask she was using was the wrong pH for her skin, I switched her skincare to a mildly acidic natural four-step skincare system; and I called in a topical prescription for her to the local compounding pharmacy for daily use on her face: azeloyl glycine with 5% niacinamide. (Note: Azeloyl glycine (also known as potassium azeloyl diglycinate or azeloglicina) is an azelaic acid derivative that resolves many of the issues azelaic acid carries with it. Azeloyl glycine is known for helping control the secretion of sebum and appears to have anti-inflammatory benefits when combined with niacinamide.13 Even sensitive skin types have found azeloyl glycine easier to tolerate compared to azelaic acid. Nicotinamide gel applied twice daily for two months helps significantly reduce acne, appears to reduce excess sebum, decreases skin inflammation, and improves the skin barrier, according to a 2013 paper published in the International Journal of Dermatology.14)
The next month, she shared she had a decrease in blackheads as well as cystic acne and that the topical treatment on her face had helped so much that she reduced its use to just three to four times per week. At that point, she reported that her skin was neither oily nor dry. The texture of her skin had improved. Even her esthetician said the skin on her face was the best it had ever looked, so she had stopped seeing her esthetician for regular facials. She mentioned that her back acne was still a problem even though her face had cleared up. At that point, I called in a topical prescription to apply daily to the skin on her back: Natapres (a blend of aspen bark, radish root, and honeysuckle) at 10% for antibacterial activity, with niacinamide at 4%, and glycolic acid at 3%. I also recommended using natural Konjac sponges for face and body with her mildly acidic plant oil-based natural cleanser; and, I recommended a series of PRP facials for acne scarring.
At the next appointment a month later, her back acne had reduced about 40%. When I inquired about her laundry soap, she said it was an eco-friendly detergent from the health food store. She tested (per my request) and found the pH to be 7. So, I had her add one-half to one cup vinegar to each laundry wash (50/50) to decrease the pH toward mild acidity. And, at her next appointment the acne on her back was an additional 40% better.
Three years later, I continue to see this patient a few times per year. She’s received three PRP facials, which have decreased her acne scarring. Breakouts on her face and back only occur when she’s eating sweets, traveling, and stressed, such as during the holidays. As with all my acne patients after they recover, she is thrilled to not only have her healthy skin back, but also her confidence.
As you can see from this case, we addressed the root causes of inflammation, nutritional deficiencies, hormonal imbalances, and microbiome disturbance internally with supplements and a healthy diet. And, while she had some improvement, there was greater recovery after adding in topical treatments with sebum-balancing, antibacterial and anti-inflammatory properties, plus the mildly acidic daily skin care system and topical support.
Hopefully, this inspires you to view your patients’ skin as their magic mirror. What messages is the skin giving you that will direct their care, even if dermatologic conditions are only one of their concerns? You can also use skin as a guide for recovery since it is right on the surface and your patients can easily give you feedback. And, when they see the change right in the mirror, they will be forever grateful.
Bio:
Dr. Trevor Cates graduated from the National University of Natural Medicine in 2000 and was the first woman licensed as a naturopathic doctor in the state of California. She was appointed by former Governor Arnold Schwarzenegger to California’s Bureau of Naturopathic Medicine Advisory Council. She has worked with world-renowned spas and sees patients from around the world from her Park City, Utah base. She is author of the USA Today and Amazon #1 bestselling book Clean Skin from Within. She has her own PBS Special Younger Skin from Within and is host of The Spa Dr. Podcast. Dr. Cates’ The Spa Dr. skincare line is formulated with the ideal pH and plant-based organic ingredients designed to help individuals achieve vibrantly healthy skin. www.TheSpaDr.com
References
- The Global Dermatology Market. April 2018. https://www.marketresearch.com/GMR-Data-Ltd-v3996/Global-Dermatology-11687402/?progid=90909
- Abuabara K, et al. Prevalence of Atopic Eczema Among Patients Seen in Primary Care: Data From The Health Improvement Network. Ann Intern Med. 2018.
- Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology: a review of recent findings. J Am Acad Dermatol. 2013; 69: S15–S26.
- Menter A, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: Section 1. Overview of psoriasis and guidelines of care for the treatment of psoriasis with biologics. J Am Acad Dermatol. 2008 May;58(5):826-50.
- Bickers DR, et al. The burden of skin diseases: 2004 a joint project of the American Academy of Dermatology Association and the Society for Investigative Dermatology. Journal of the American Academy of Dermatology. 2006;55:490-500.
- Bhate K, Williams HC. Epidemiology of acne vulgaris. The British Journal of Dermatology. 2013;168:474-85.
- Tanghetti EA, et al. Understanding the Burden of Adult Female Acne. The Journal of Clinical and Aesthetic Dermatology. 2014;7:22-30.
- Grice EA, et al. Topographical and temporal diversity of the human skin microbiome. Science. 2009; 324: 1, 190-1, 192.
- Rodrigues H. The cutaneous ecosystem: the roles of the skin microbiome in health and its association with inflammatory skin conditions in humans and animals. Vet Dermatol. 2017; 28(1):60-e15.
- O’Neill CA, et al. The gut-skin axis in health and disease: a paradigm with therapeutic implications. Bioessays. 2016; 38 1167–1176.
- Lambers H, et al. Natural skin surface pH is on average below 5, which is beneficial for its resident flora. Int J Cosmet Sci. 2006; 28(5):359-70.
- Jung YC, et al. Effect of skin pH for wrinkle formation on Asian: Korean, Vietnamese and Singaporean. J Eur Acad Dermatol Venereol. 2013; 27(3):e328-32.
- Lembo S, et al. Azeloglycine and niacinamide down-regulate pro-inflammatory mediators in vitro. G Ital Dermatol Venereol. 2017 Feb;152(1):90-92.
- Shalita AR, et al. Topical Nicotinamide Com- pared with Clindamycin Gel in the Treatment of Inflammatory Acne Vulgaris. International Journal of Dermatology. June 1995;34(6): 434–7.