Marc Grossman, OD, LAc
Overview
Age-related macular degeneration (AMD) is the leading cause of irreversible blindness today and is the leading cause of vision loss of people over 60.1 By the year 2020, an estimated 7.5 million Americans will suffer significant vision loss due to this disease. In 2010, 2.5 percent of white adults age 50 and older had AMD. By comparison, AMD affected 0.9 percent each of blacks, Hispanics, and people of other races. The risk of AMD increases with age. The disease is most common among older white Americans, affecting more than 14 percent of white Americans age 80 and older.1 Although there is no effective conventional treatment yet, natural remedies can go a long way in helping to prevent this disorder from progressing to the point of vision loss.
What is macular degeneration? Macular degeneration is the slow deterioration of the cells in the macula, a tiny yellowish area near the center of the retina where vision is most acute. This deterioration affects central vision, the vision used for reading, writing, driving, and identifying faces. With macular degeneration, straight lines become crooked, distinct shapes are blurry, lines become wavy, and a fog forms in the center of vision. Peripheral vision however is not affected.
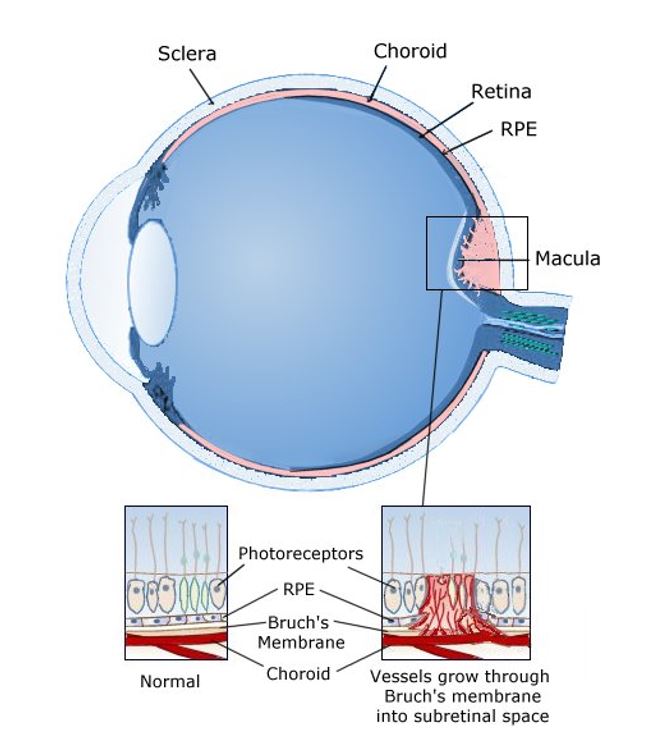
The two most common types of macular degeneration are the dry and wet type. Ninety per cent of people with macular degeneration have the dry type, in which small yellow spots called drusen form underneath the macula. The drusen slowly break down the cells in the macula, causing distorted vision. In approximately 10-15% of the cases, dry macular degeneration can progress to the second, more severe type called wet macular degeneration.
In the wet type of macular degeneration, abnormal blood vessels begin to grow toward the macula. These new vessels may leak blood and fluid that further deteriorate the macula, causing rapid and severe vision loss.
Parts of the Retina
The retina consists of four different layers, specifically:
- Outer neural layer, which contains nerve cells and blood vessels;
- Photoreceptor layer, which is a single layer containing the light sensing rods and cones;
- Pigmented retinal epithelium (RPE), with the Bruch’s membrane separating the RPE from the
- Choroid layer, consisting of connective tissue and very fine capillaries known as choriocapillaries. They are responsible for carrying nutrients and oxygen to the cellular layers above them.
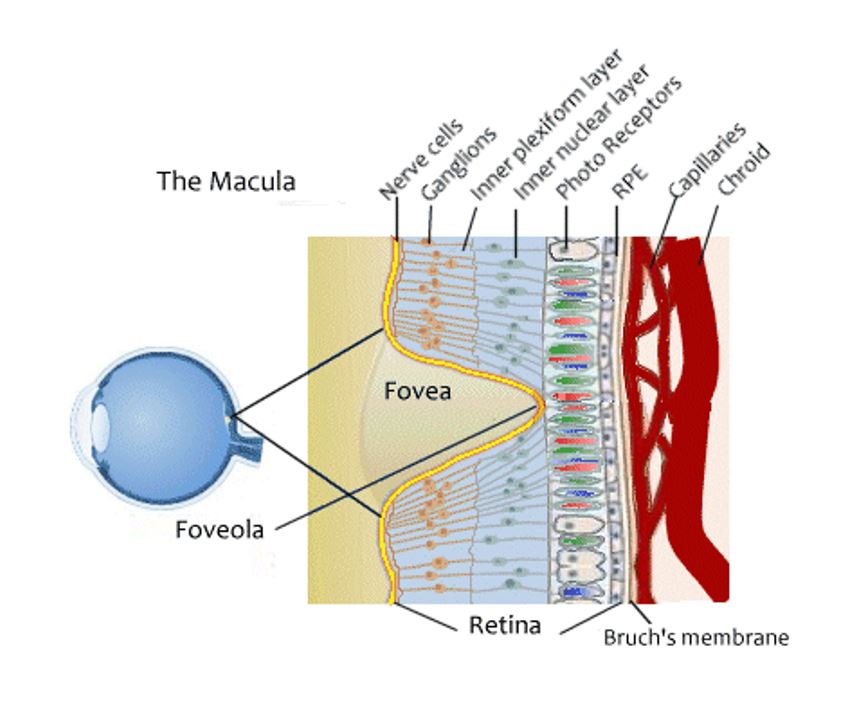
The choroid layer contains most of the eyeball’s blood vessels. It is also the layer prone to bacterial and secondary infections. If not treated, the abnormal blood vessel growth can readily develop resulting in sight impairment or eventually total vision loss.
The macula (see illustration) contains two areas of unusually high concentrations of cones, which are the photoreceptors responsible for daytime and color vision, fine detail and central vision. There is a slightly depressed area in the center of the macula called the fovea where there is no retinal nerve fiber layer, only photoreceptors, approximately 199 to 300 thousand cones per square millimeter. At the center of the fovea is the foveola where there are no rods, only cones.
The gradual breakdown of these cells in the macula results in damage to or loss of your central vision. The macula provides focus in the center of vision where your vision sharpness is most acute. Such deterioration reduces the ability to read and recognize faces, two important tasks that use the central vision.
Types of Macular Degeneration (AMD)
The most common type (90%) is dry AMD, which results from the inability of the retina to reabsorb the natural waste created in the retina in the process of passing light from the photoreceptor cells to the optic nerve (and other normal physiological activity). The result is the slow deposit of this waste onto the retina (called “drusen”), which over time can result in loss in healthy vision. Drusen are thought to be comprised of waste proteins and lipids (oily material) that begin to accumulate due to poor circulation and waste-flushing in the eye. Antioxidants are important for the normal waste-clearing process and have the potential for even reducing drusen in the eyes. The drusen slowly crowd, distort, or break the visual cells in the macula, leading to deterioration and resulting in blurred vision. Because drusen also include pro-inflammatory components, it is thought that they trigger the immune system. AMD has few symptoms in the early stages, so it is important to have your eyes examined regularly, and yearly, if you have a family history. For people who have early AMD in both eyes, about 10-15% percent will develop late AMD in at least one eye after 10 years.2
The second type (10%) of macular degeneration is the “wet” form, (also known as choroidal neovascularization) in which new blood vessels begin to develop near (underneath) the macula, causing fast and serious vision loss. These vessels can leak fluid and blood, which may lead to swelling and damage of the macula. The damage may be rapid and severe, unlike the more gradual course of dry macular degeneration. It is possible to have both dry (geographic) atrophy and neovascular AMD in the same eye, and either condition can appear first. Wet macular degeneration is determined through a dilated retinal examination that can identify the presence of bleeding or leakage in the retina (wet AMD) versus only drusen, which are waste deposits underneath the retinal pigmented epithelium (dry AMD). Note that even if one has drusen in the retina, the diagnosis may not be dry AMD until the eye doctor determines the location and severity of the drusen.
If AMD is found first in one eye, the other eye tends to follow the same progression. This is because the nutrient deficiencies and other system-wide problems would exist in both eyes but manifest in one eye before the other. Research shows that a healthy diet and taking targeted supplements can significantly reduce the onset of neovascularization (new blood vessel growth that results in retinal bleeding).3-8
Stargardt’s disease is the third type of macular degeneration. It affects about one in 10,000 children in the US. Although the disease starts before age 20, you may not notice vision loss until age 30 to 40. It is a genetic form of macular degeneration where patients need to avoid supplementing with vitamins that contain vitamin A and beta-carotene, along with foods high in certain carotenoids that can be converted to vitamin A in the body.9
Myopic macular degeneration, the fourth type, typically results in those people who are very nearsighted. In these cases, there is an extreme elongation of the eyeball, which causes the stretching of the retina and can result in tears in the macula and bleeding beneath the retina. Over time, this can cause cells in the center of the retina (the macula) to atrophy or die, causing a blind spot in the center of the visual field. In some cases, this form of macular degeneration can convert to the wet form. People who are very nearsighted, generally requiring glasses of -6 diopters or more, are at risk for myopic macular degeneration. The risk is higher as myopia becomes greater than -10 diopters.
Pathology of Macular Degeneration
The development and progression of macular degeneration rests upon the occurrence of the following pathological changes in the eye:
- Oxidative stress is the imbalance between damage-causing free radicals and protective antioxidants. Because of its high metabolic activity, the retina is especially vulnerable to stress from free radicals. Inability of the retinal tissue to obtain adequate oxygen and nutrients leads to deterioration of the pigmented layer, which protects the retina from UV and blue light damage.10,11 Antioxidants can significantly reduce the effects of oxidative stress.12
- Angiogenesis is the growth of new, rapidly made blood vessels in response to a lack of oxygen. These fragile blood vessels tend to easily break and leak fluid and blood onto and into the retina, which can distort vision in the retina.Targeted nutrients can inhibit new (unwanted) blood vessel growth.3
Apoptosis is the process of cell death that allows the body to replace worn and damaged tissue cells with new cells. However, in the retina, oxidative stress is closely tied to excessive cell death. Antioxidants and enzymes can reduce excessive apoptosis.12,13
Inflammation response is the body’s attempt to rescue tissue from cell injury but can also result in vision damage over time due to scar tissue and bleeding in the retina (growth of new, unwanted blood vessels).14 Proteins that are responsible for the immune results are among the constituents of drusen deposits in the retina.
Signs and Symptoms
- Lines look distorted or wavy. Try the Amsler test for both dry and wet AMD. In more developed AMD, the Amsler grid can look quite distorted.
- Shapes look blurred, fuzzy, or hazy in central vision.
- Colors appear dimmer and less distinct.
- Words are hard to read because they are blurred.
- Blank or dark areas hide the center area of your vision.
- The center of vision looks foggy or cloudy.
Causes and Risk Factors
Macular degeneration in childhood and early adulthood is typically the result of genetics, versus seniors who develop age-related macular degeneration, which is more related to poor circulation, inadequate waste removal, and lack of availability of oxygen and essential nutrients getting to the eyes due to poor digestion, medications, less active lifestyle, etc. However, genetics does play a role in the age-related form of macular degeneration. One study determined that there was a 12-fold increase in the risk of getting macular degeneration if one had a sibling with AMD.15 The risk factor was considered large with a parent with AMD.
The field of epigenetics shows that even though one may have a genetic disposition of getting AMD (or any other health condition), environmental factors including early childhood nurturing and lifelong lifestyle choices can play a significant role in whether these genes become active or not.15
There is a great deal of peer review research showing that the likelihood of onset of AMD can be significantly reduced through lifestyle choices such as eating a healthy diet,16-18 exercising regularly,19 not smoking,3,20 avoiding heavy drinking21 (moderate drinking of wine may have a beneficial effect22), managing chronic stress,23 not being overweight,24 controlling blood pressure,25 and high cholesterol,26 as well as supplementing with targeted supplements such as lutein, zeaxanthin and omega-3 fatty acids (such as fish oil or DHA from algae for those who are vegetarian).
Once a diagnosis of dry AMD is given, healthy lifestyle choices can both help maintain healthy vision and reduce the risk of the dry form of AMD turning to the wet form.
The more advanced the AMD has gotten, healthy lifestyle choices and targeted supplementation still can play a major role in slowing down and stabilizing the AMD; but lost vision due to the death of retinal cells cannot at this time be regenerated (though excellent research such as stem cells to regenerate lost retinal cells is underway). Keep in mind that patients can sometimes see improved vision if low functioning retinal cells can be stimulated and helped to become more active through diet, exercise, and targeted supplementation. Microstimulation can also be very useful to revitalize unhealthy retinal cells.
In addition to genetics and lifestyle factors, other risk factors include the following:
- Free radicals can damage the eyes. Free radicals are formed when the blue and ultraviolet sunlight passes through the crystalline lens of the eye. Free radicals are also byproducts of our bodies’ natural metabolic processes. These chemicals are highly reactive and cause oxidation; the result is destabilization of healthy macula cells in the eyes. Blue light alone is not tied to macular degeneration; however, researchers have found that there is a consistent and significant connection between age-related macular degeneration and patients in the lowest quartile nutritional intake of vitamin C, vitamin E, zeaxanthin, and dietary zinc.27
- Hypertension. People with high blood pressure are more likely to develop AMD than those with normal blood pressure.25
- Smoking, chronic fatigue, and a weakened immune system hasten damage from free radicals. Smoking increases the risk of AMD by 200-300%.3,20
- Poor digestion and nutritional deficiencies: People with AMD are often deficient in a number of nutrients that are essential to eye health such as lutein and carotenoids,17 essential fatty acids, zeaxanthin, taurine, antioxidants, zinc, bioflavonoids, selenium, and vitamin B-complex.16-18, 28
- Systemic inflammation, indicated by high levels of C-reactive protein, has been tied to increased macular degeneration risk.29
- High homocysteine levels.30,31
- Women are more at risk at developing AMD.32
- People with diabetes are more at risk to develop AMD.33
- Phototoxicity is caused by exposure to blue and ultraviolet (UV) radiation, both of which adversely affect the functioning of retinal pigment epithelium (RPE) cells. The RPE’s role is to nourish the fragile nerve tissue of the retina and maintain its health by transporting molecules in and out, getting rid of dead cells, secreting hormones, modulating immune factors, and more. All this has magnified the RPE’s role in macular degeneration.20 RPE cells are susceptible cell death induced by ultraviolet B (UVB) irradiation. Excessive exposure to sunlight without protective sunglasses is a risk factor for AMD. The retinal pigment epithelium (RPE) closely interacts with photoreceptors in the maintenance of visual function, responsible for providing blood and nutrients to reach the photoreceptor cells and supports the elimination of waste products.
- Drugs that can damage the retina:34Plaquenil® (hydroxychloroquine sulfate), often prescribed for rheumatoid arthritis, has been found to cause permanent damage to the retina; Catapres® (clonidine hydrochloride is the generic name), for high blood pressure; NSAIDs (non-steroidal, anti-inflammatory drugs). Side effects from regular use include retinal hemorrhages. This group includes ibuprofen, aspirin, ketoprofen, flurbiprofen, and naproxen sodium. In addition, acetaminophen (Tylenol), though not a NSAID, can harm vision.
Related Conditions
Poor circulation in the eye is a contributing factor to many eye conditions and is a side effect of diabetes and cardiovascular disease.35
Elevated homocysteine levels have been associated not only with macular degeneration but also glaucoma, diabetic retinopathy, optic neuropathy, and ocular complications from Behcet disease, as well as a macular pucker (epiretinal membrane), in which a thin layer of tissue grows over the retina.36
Retinitis pigmentosa is a degenerative disorder of the photoreceptor cells of the retina.
Conventional Treatment
No effective conventional treatment currently exists for dry macular degeneration.
Wet macular degeneration is typically treated with injections of Lucentis®, Avestin®, or Eylea®. These drugs have anti-antigiogenic properties, meaning they help prevent the growth of new blood vessels, while drying up existing blood vessels that are leaking. The injections are typically necessary on an ongoing basis, depending on the severity and history of bleeding. Over the long run, they do not necessarily prevent vision loss; however, they can be essential for helping to slow down the progression of the wet AMD. Moreover, these drugs are not designed to address the underlying problem, which in most cases, is the inability of the body to deliver essential nutrients to the retina and naturally eliminate waste materials generated in an ongoing process in the retina. Ultimately, the short-term goal is to stabilize the AMD, and the long-term goal is to maintain healthy vision and prevent additional vision loss. Drugs can have potentially serious side effects, so the benefits of using them should be evaluated with your eye doctor and your family doctor.
Laser surgery (photodynamic therapy) may be an alternative option to injections if the eye doctor determines that the injections may be ineffective or contraindicated for the patient. Your eye doctor will be able to provide guidance on the best therapy for you. Laser surgery accurately targets and seals leaking blood vessels, through the injection of a form of ink into the blood stream that gets absorbed at a much higher rate by leaking blood vessels than healthy ones.
Complementary Treatment
As always, prevention is the best medicine. Since less than one per cent of people with macular degeneration have progressed to the point of legal blindness, most are in a position to benefit greatly from preventive measures, particularly at the earlier stages of the disease.
Taking targeted supplements and establishing healthy lifestyle habits are still helpful at any stage of AMD, keeping in mind that the preservation of vision and potential level of vision improvement is based on the vision the patient has at the time of incorporating complementary approaches. Oxidative stress and inflammation play critical roles in the initiation and progression of a range of eye diseases, including age-related macular degeneration, glaucoma, cataract and diabetic retinopathy that lead to progressive loss of vision and blindness if untreated.37-39 There is growing evidence that supplementing with targeted antioxidants, with their antioxidant and anti-inflammatory properties, may have a potential role in the prevention and treatment of these age-related eye diseases and disorder.40
Diet: We recommend following a strong alkaline diet to reduce overall inflammation in the body as chronic inflammation has been identified as a contributing factor in macular degeneration.41 It has become more accepted that both local and systemic inflammatory processes contribute to the development and progression of AMD. Chronic inflammation for many may be related to leaky gut syndrome, so again an anti-inflammatory diet should be adopted as well if applicable.
Many research studies have shown that diet has a significant effect on health of the macula. Unfortunately, once a person has macular degeneration, a healthy diet is not enough to prevent this disease from worsening, so other interventions are needed which may include conventional as well as targeted supplementation.
It is very important to make sure your diet includes plenty of fresh, preferably organic, dark leafy greens. These vegetables are rich in carotenoids, which are phytonutrients (“plant chemicals”) that help plants absorb light energy for use in photosynthesis, and that deactivate free radicals, meaning they have antioxidant properties and are helpful for the entire body. Carotenoids are also responsible for the bright red, yellow, and orange color pigments in many fruits and vegetables; however, as evidenced by dark leafy greens, not all fruits and vegetables that contain carotenoids have these colorations. There are more than 600 carotenoids in the body, but two, lutein and zeathanthin, are of particular importance to eye health. So, even if you don’t like vegetables such as collards, kale, Swiss chard, and spinach, you can add them to soups, puree them in green drinks, juice them with other fruits and vegetables, or add them to other greens in salads. Many studies report that the nutrients found in these healthy vegetables lower the risk of developing macular degeneration.
Numerous research studies have shown that diets high in antioxidants which includes a lot of fruits (particularly colored fruit such as berries that are lower in sugar, and leafy green or colorful vegetables) play two critical roles; they significantly reduce the risk of AMD onset, and they help to protect AMD patients from vision loss.12,42
It is also very important to reduce or eliminate all types of refined sugars (particularly white sugar, but also fructose, sucrose, fruit juice concentrates, maltose, dextrose, glucose, and refined carbohydrates). This includes “natural” drinks that contain a lot of sugar, including all fruit juices. Even milk sugar, lactose, found in all dairy products can contribute to macular degeneration as sugar contributes to overall body inflammation and the fluidity of circulation throughout the body and eyes. In one study those in the highest one-fifth of the dietary glycemic index (a system that ranks foods on a scale from 1 to 100 based on their effect on blood-sugar levels) had more than a 40 percent increased risk of significant macular degeneration than those in the lowest one-fifth.18
Click here to read Dr. Grossman’s article:
Cataracts – An integrative Medical Approach
In addition to these dietary guidelines, it is very important to drink eight glasses of water per day (preferably filtered or purified). This is optimally taken as a four-ounce glass of water every half-hour, to equal 16 four-ounce glasses. Our bloodstream can only effectively handle about four ounces at any one time. When you drink more than four ounces at a time, this means more work for the kidneys to filter water that hasn’t had a chance to travel through the lymph system and clean body tissues. Adequate water intake helps to maintain the flow of nutrients to the lens and to release wastes and toxins from tissues. Do not smoke (or quit smoking); smoking increases the risk of AMD onset by two-to-three times.20
It is important to limit or eliminate dairy products. For some people, regular consumption of dairy products can exacerbate eye problems by causing sinus congestion, which can impair lymph and blood drainage from the area around the eyes. When lymph and blood can’t flow in and out of the eyes, nutrients don’t reach the eyes, and toxins and metabolic wastes aren’t eliminated as efficiently. Many people are lactose intolerant to some degree, so you may want to avoid dairy for at least one month to experience the effects of this, and to see the differences in your body and eyes. As a general rule, reducing or eliminating dairy from one’s diet has many benefits. If you still choose to consume dairy, commit to organic products from A2 cows. A2 milk is just one amino acid different from the more common A1 milk products and the resulting proteins do not have the damaging effects that have come to be associated with milk products. Alternatively, you can switch to goat milk since milk from goats does not carry the A1 gene; or at the very least, obtain fresh, raw milk from local farmers for the freshest product. In general, changes in lifestyle related to healthier vision and taking targeted supplements will start making a difference right away; but it may take three-to-six months before maximum benefit starts to be seen.
Drinking freshly made juice is also important. Our recommendation is six-to-eight ounces of fresh juice per day. Choose at least four-to-six items to combine; use mostly green leafy vegetables and do not use too many carrots because of their high natural sugar content (1 carrot per 12-16 oz. juice is preferred), as well as using organic products as much as possible. You can choose any combination of the recommended nutrients (in Part 2 to be published in TL May 2020) (always include green, leafy vegetables), plus add any of your favorite fruits and vegetables: broccoli, green and red bell pepper, raspberries, apples, copious amounts of dark leafy greens.
References
- https://nei.nih.gov/eyedata/amd
- Jager RD, Mieler WF, Miller JW. Age-Related Macular Degeneration. NEJM. June 12, 2008;358(24):2606-2617.
- Seddon JM, et al. Dietary carotenoids, vitamins A, C, and E, and advanced age-related macular degeneration. JAMA. 1994;272(18):1413-1420.
- Studies show there is consistent evidence that high intake of docosahexaenoic acid (DHA; 22:6, n-3), a long-chain omega-3 polyunsaturated fatty acid (PUFA) present in oily fish, is associated with a reduced risk of neovascular AMD. 1.) Chong EW, et al. Dietary omega-3 fatty acid and fish intake in the primary prevention of age-related macular degeneration: a systematic review and meta-analysis. Arch Ophthalmol. 2008;126(6): 826–833. 2.) Augood C, et al. Oily fish consumption, dietary docosahexaenoic acid and eicosapentaenoic acid intakes, and associations with neovascular age-related macular degeneration. Am J Clin Nutr. 2008;88(2): 398–406. 3.) Smith W, Mitchell P, Leeder SR. Dietary fat and fish intake and age-related maculopathy. Arch Ophthalmol. 2000;118(3): 401–404. 4.) Cho E, et al. Prospective study of dietary fat and the risk of age-related macular degeneration. Am J Clin Nutr. 2001;73(2): 209–218. 5.) Merle B, et al. Dietary omega-3 fatty acids and the risk for age-related maculopathy: the Alienor Study. Invest Ophthalmol Vis Sci. 2001;52(8): 6004–6011. 6.) Seddon JM, et al. Dietary fat and risk for advanced age-related macular degeneration. Arch Ophthalmol. 2001;119(8): 1191–1199. 7.) Merle BM, et al. High concentrations of plasma n3 fatty acids are associated with decreased risk for late age-related macular degeneration. J Nutr. 2013;143(4): 505–511.
- SanGiovanni JP, Chew EY. The role of omega-3 long-chain polyunsaturated fatty acids in health and disease of the retina. Prog Retin Eye Res. 2005;24(1): 87–138.
- C. Tamar, et al, Serum dehydroepiandrosterone sulphate level in age-related macular degeneration. American Journal of Ophthalmology. February 2007. (Researchers found that the lower the levels of DHEA the greater the severity of the macular degeneration in both men and women; note that a 2013 study contradicted these findings, so more research needs to be done).
- Cho E, et al. Prospective study of intake of fruits, vegetables, vitamins, and carotenoids and risk of age-related maculopathy. Arch Ophthalmol. 2004;122(6):883-892.
- Wang S, et al. Tissue Distribution of trans-Resveratrol and Its Metabolites after Oral Administration in Human Eyes. Journal of Ophthalmology. March, 2017.
- Sofi F, et al. Dietary profile of patients with Stargardt’s disease and Retinitis Pigmentosa: is there a role for a nutritional approach? BMC Ophthalmology. January 2016.
- Youssef PN, Sheibani N, Albert DM. Retinal Light Toxicity. Eye. 2011; 25:1-14.
- Mares-Perlman JA, et al. The body of evidence to support a protective role for lutein and zeaxanthin in delaying chronic disease. Overview. J Nutr. 2002;132(3):518S-524S. This study suggests that the quality but not the quantity of dietary carbohydrate influences the risk of AMD in both the early and late stages.
- Vives-Bauza C, et al. The age lipid A2E and mitochondrial dysfunction synergistically impair phagocytosis by retinal pigment epithelial cells. Journal of Biological Chemistry. November 2008. Antioxidants fight the resulting damage by protecting the eye from oxidative stress.
- Cai J, et al. Oxidative Damage and Protection of the RPE. Progress in Retinal and Eye Research. 2000;19(2): 205-221.
- Seddon JM, et al. Progression of Age-Related Macular Degeneration: Prospective Assessment of C-Reactive Protein, Interleukin-6, and Other Cardiovascular Biomarkers. Arch Ophthalmol. 2005;123:774-782.
- Shahid H, et al. Age-related macular degeneration: the importance of family history as a risk factor. Br J Ophthalmol. 2012;96(3):427-431.
- Pinazo-Durán MD, et al. Do Nutritional Supplements Have a Role in Age Related Macular Degeneration Prevention? J Ophthalmol. 2014; ID901686.
- Cooper DA, Eldridge AL, Peters JC. Dietary carotenoids and certain cancers, heart disease, and age-related macular degeneration: a review of recent research. Nutr Rev. 1999;57(7):201-214.
- Chiu CJ, et al. Association between dietary glycemic index and age-related macular degeneration in nondiabetic participants in the Age-Related Eye Disease Study. Am J Clin Nutr. 2007;86(1):180-8.
- McGuinness MB, et al, Past physical activity and age-related macular degeneration: the Melbourne Collaborative Cohort Study. British Journal of Ophthalogy. October 2016.
- Stanislovaitiene D, et al. SCARB1 rs5888 is associated with the risk of age-related macular degeneration susceptibility and an impaired macular area. Ophthalmic Genetics. July 2016.
- Cederbaum AI. Role of lipid peroxidation and oxidative stress in alcohol toxicity. Free Radic Biol Med. 1989;7:537–5394.
- Obisesan TO, et al. Moderate wine consumption is associated with decreased odds of developing age-related macular degeneration in NHANES-1. J Am Geriatr Soc. 1998;46:1–7.
- Dougherty BE., Cooley S-S L, Davidorf F H. Measurement of Perceived Stress in Age-Related Macular Degeneration. Optometry and Vision Science. March 2017;94(3):290–296.
- Zhang Q-Y, et al. Overweight, Obesity, and Risk of Age-Related Macular Degeneration. Invest Ophthalmol Vis Sci. 2016 Mar;57(3):1276-83.
- Hyman L, et al. Hypertension, Cardiovascular Disease, and Age-Related Macular Degeneration. Arch Ophthalmol. 2000 Mar;118(3):351-8.
- Targeting cholesterol build-up in eye may slow age-related vision loss. April 3, 2013.
- VandenLangenberg GM, et al. Associations between antioxidant and zinc intake and the 5-year incidence of early age-related maculopathy in the Beaver Dam Eye Study. Am J Epidemiol. 1998 Jul 15;148(2):204-14.
- Patients with confluent soft drusen, or “pre-wet” ARMD, were found to have evidence of vitamin B6 deficiency. B. Lane, Annual Meeting of the American College of Nutrition, 1991.
- Mitta VP, et al. C-Reactive Protein and the Incidence of Macular Degeneration: Pooled Analysis of Five Cohorts. JAMA Ophthalmol. April 1, 2013;131(4):507-513.
- Elevated homocysteine is associated with a number of degenerative eye diseases, including macular degeneration, glaucoma, diabetic retinopathy, optic neuropathy and ocular complications from Behcet disease. It is also associated with accelerating the progression of the aging process. 1.) Bleich S, et al. Elevated homocysteine levels in aqueous humor of patients with pseudoexfoliation glaucoma. American Journal of Ophthalmology. July 2004. 2.) Coral K, et al. Plasma homocysteine and total thiol content in patients with exudative age-related macular degeneration. Eye. April 2005.
- Huang P, et al. Homocysteine and the risk of age-related macular degeneration: a systematic review and meta-analysis. Scientific Reports. July 2015. The meta-analysis results demonstrated that with high homocysteine and AMD, vitamin B12 was also low. The researchers also point out that AMD is a condition in which there are many contributing factors; vitamin B12 and homocysteine are not the sole indicators.
- Feskanich D, et al. Menopausal and Reproductive Factors and Risk of Age-Related Macular Degeneration. Arch Ophthalmol. 2008;126(4):519-524.
- Mares-Perlman JA, et al. The body of evidence to support a protective role for lutein and zeaxanthin in delaying chronic disease. Overview. J Nutr. 2002;132(3):518S-524S. This cross-sectional analysis suggested that poor dietary carbohydrate quality may increase the risk of AMD through several common etiologic factors of diabetes and CVD, including the formation of AGE and increases in oxidative stress, inflammation, and hyperlipidemia. This study also suggests that the quality, but not the quantity, of dietary carbohydrate influences the risk of AMD in both the early and late stages of the disease.
- Fraunfelder FT, Meyer SM. The national registry of drug-induced side effects. Aust J Ophthalmol. May 1984;12(2):129-31. And https://www.macular.org/medications-use-caution.
- Wu J, et al. Age-Related Macular Degeneration and the Incidence of Cardiovascular Disease: A Systematic Review and Meta-Analysis. PLoS One. 2014; 9(3): e89600.
- Bleich S, et al. Elevated homocysteine levels in aqueous humor of patients with pseudoexfoliation glaucoma. American Journal of Ophthalmology. July 2004.
- Levkovitch-Verbin H. Retinal ganglion cell apoptotic pathway in glaucoma: Initiating and downstream mechanisms. Prog. Brain Res. 2015;220:37–57.
- Kowluru RA, Mishra M. Oxidative stress, mitochondrial damage and diabetic retinopathy. Biochim Biophys Acta. 2015;1852:2474–2483.
- Dib B, et al. Mitochondrial DNA has a pro-inflammatory role in AMD. Biochim Biophys Acta. 2015;1853:2897–2906.
- Rhone M., Basu A. Phytochemicals and age-related eye diseases. Nutr. Rev. 2008;66:465–472.
- Tan PL, Rickman CB, Katsanis N. AMD and the alternate complement pathway: genetics and functional implications. Human Genomics. 2016;10(10:23.
- Hogg R, et al, AMD and micronutrient antioxidants. Current Eye Research. December 2004.

Since 1980, Dr. Marc Grossman has helped many people maintain healthy vision and even improve eyesight. He is best described as a holistic eye doctor, dedicated to helping people with conditions ranging from myopia and dry eyes to potentially vision threatening diseases such as macular degeneration and glaucoma. His combined multi-disciplinary approach using nutrition, eye exercises, lifestyle changes and Chinese medicine provides him with a wide array of tools and approaches to tackle difficult eye problems.
Dr. Grossman founded the Rye Learning Center in 1980, a multidisciplinary center for learning problems, in 1996 co-founded Integral Health Associates in New Paltz, New York, and in 1999 co-founded Natural Eye Care, Inc.
His background includes degrees in optometry, biology, physical education and learning disabilities, coupled with yoga, bioenergetics, nutrition, Chinese medicine and acupuncture, the Alexander Technique and Feldenkrais. This orientation provides the foundation for an integrated approach to vision and its influence on the body, mind and spirit of each individual patient.