By Debby Hamilton, MD, MPH
Introduction
As autoimmune disease continues to rise, we need to learn how to bring the immune system back into balance. In Part 1 of “New Understanding of Autoimmunity Development through T Helper Cell Regulation,” I discussed the new understanding of how elevated Th17 cells were involved in autoimmunity. Previously it was thought that elevated Th1 cells created autoimmunity; but with the identification of Th17 cells, researchers now believe Th17 cells appear to be the primary driver.
When Th17 cells are activated by pathogens or toxins along a mucosal border, they trigger an inflammatory response, leading to the development of autoimmunity. Since they are antagonistic to Th1, the Th1 cells are driven to lower levels, which increases the risk of infections. These infections can then trigger more elevation of Th17, continuing and worsening the autoimmune cycle. With the elevation of Th17, there is a decrease in Treg cells causing a loss of immune tolerance. With the lowering of Th1, there is an increase in Th2 with a concomitant increase in allergies.
Treatment Goal: Immune Balance
With autoimmune disease, the goal is to return the immune system to balance. This entails decreasing Th17 and Th2 while increasing Th1 and Treg cells. A balanced immune system decreases autoimmune disease and its triggers along with decreasing allergies. In addition, immune tolerance will be restored, and the immune system will be strengthened in its ability to fight infections
Autoimmune disease is a chronic inflammatory disease. Therefore, one of the goals in treating autoimmune disease is to decrease inflammation. Elevated Th17, activation of STAT3 (the transcription factor for Th17), and activation of NFkB all contribute to chronic inflammation. All three of these drive neutrophils into the tissue. Neutrophils are the first line of immune defense and are necessary to mount a needed immune response. Macrophages are called in next, and they are responsible for removing neutrophils from the tissue after they complete their function in fighting infections. If there are too many neutrophils and they are not removed, they self-destruct, causing release of ATP and other damaging molecules that lead to tissue destruction. Chronic inflammation and tissue damage arise from a continual activation of neutrophils.
Transfer Factors
Transfer factors are one tool to help with immune imbalance. They are small proteins with RNA that are made by activated T helper cells. Transfer factors by other mammals appear to be molecularly similar to human transfer factors. Antibodies are like transfer factors in that they are proteins but released by B cells as immune markers instead of by T cells.
Transfer factors are part of cell mediated immunity which is considered a Th1 response needed to fight viruses and other intercellular infections.1,2 Research has found efficacy of transfer factors for fighting many of the herpes viruses and HIV.3,4 When a patient has a low Th1, supplementing with transfer factors is a good option to support this system. By increasing Th1, this helps balance and decrease elevated Th17 levels. Transfer factors then help the body fight infections better, without tilting the body towards elevated Th17 response and autoimmunity.
The cell mediated immune response starts with an infection that invades the body. A phagocyte engulfs the infected body cell and then forms an antigen on its surface and releases cytokines to notify the Th1 CD4 cells to mount a cell mediated response. These Th1 CD4 cells release transfer factors and Th1 cytokines, which stimulate an increase in new T helper CD4 cells, new cytotoxic T CD8 cells, natural killer cells and macrophages. The transfer factors bind to an antigen on an infected body cell. The CD8 killer T cells target the cell tagged with the transfer factor to destroy it. Natural killer cells are also cytotoxic by releasing proteins called perforin that form holes in the cell membrane where granzymes enter to destroy the virus inside the cell. NK cells are activated in response to interferons or macrophage-derived cytokines. They serve to contain viral infections while the adaptive immune response is generating antigen-specific cytotoxic T cells that can clear the infection.
Transfer factors are derived from leukocytes (dialyzable leukocyte extract: DLE), bovine colostrum, or egg yolk. General transfer factors increase the number of T helper CD4 cells, T cytotoxic CD8 cells, macrophages, and natural killer cells so the immune system is ready to fight infections. Targeted transfer factors can be made in a manner to promote passive immunity. Chickens or cows are infected with attenuated specific antigens. Once the animals produce an immune response, the transfer factors are collected. These targeted transfer factors when used as a supplement give the person passive immunity to that antigen. Research has shown this can be an effective way to support the immune system. Children with cancer and no immunity to varicella were randomized to receive a targeted transfer factor to varicella or placebo.5 After 12 to 30 months, only one out of 16 children developed varicella in the transfer factor group versus 13 out of 15 children in the placebo group developed varicella.5 Research has not repeated studies like this one even though the results were significant for strengthening immunity.
With autoimmune disease, the goal is to return the immune system to balance. This entails decreasing Th17 and Th2 while increasing Th1 and Treg cells. A balanced immune system decreases autoimmune disease and its triggers along with decreasing allergies.
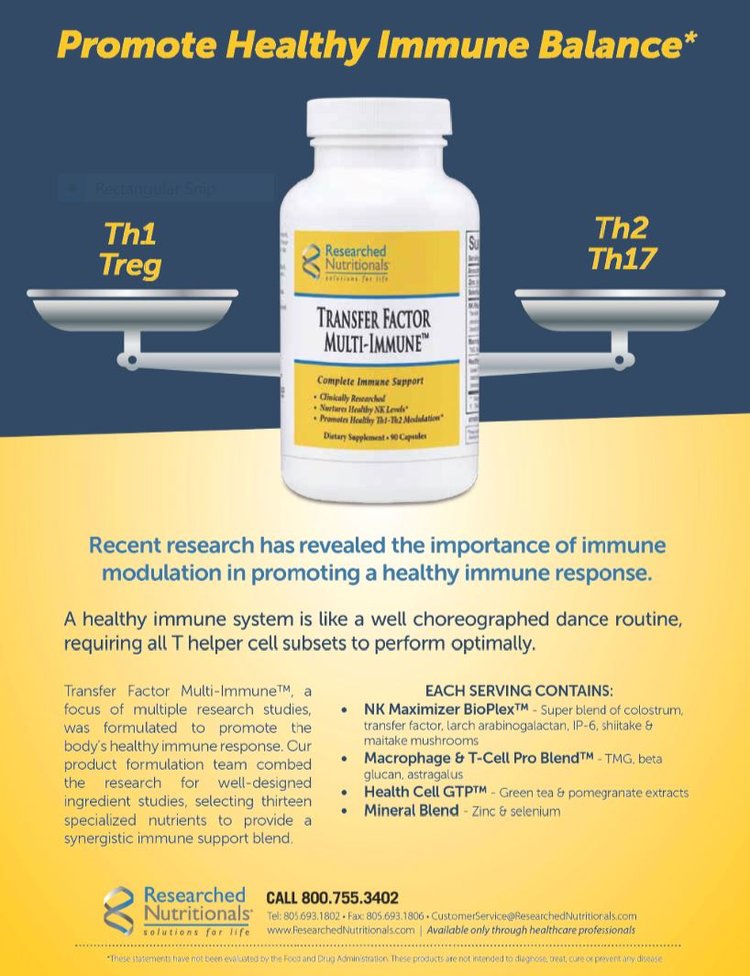
Transfer Factor Multi-ImmuneTM
To learn more about transfer factors’ specific effects on the immune system, research was done on a supplement called Transfer Factor Multi-Immune™ (TFMI).6 This product is a multi-ingredient supplement that contains transfer factors, a small amount of colostrum along with immune-supporting mushrooms and herbs, zinc, and selenium. In vitro research was completed to investigate both immune response and immune modulation. Much confusion has existed about whether proline rich peptides are the same as transfer factors, so Transfer Factor Multi-Immune™ was compared to proline-rich peptides (PRP) with the additional immune support the same as the supplement. Colostrum with the herbal blend but no transfer factors was also compared. All were measured against a control.
The three products compared for the study:
- Transfer Factor Multi-Immune™ (Researched Nutritionals) plus colostrum/herbal blend
- Colostrum and Herbal blend portion (excludes transfer factor)
- Proline-rich Peptides (in place of transfer factor), colostrum and herbal blend
The study measured immune activation, cytokine response, and cytotoxic response. The research studied three different effects on the immune system:
- Immune activation: How the body begins an immune response by activating specific types of white blood cells
- Cytokine (inflammatory) response: Measurement of cytokine chemical messenger release from white blood cells
- Cytotoxic response: Measurement of cell destruction ability by natural killer cells
The study found a difference between the three supplements for immune activation and immune modulation. With this information, it appears that transfer factors and proline-rich peptides (PRP) are not the same entity, as the transfer factors demonstrated the most powerful response in all immune categories tested. For both natural killer cell activation and T and B cell lymphocyte activation, TFMI had a three- to four-fold improvement over the colostrum and PRP supplements. For an acute immune reaction, a strong immediate cytokine response is needed; TFMI was significantly stronger than the PRP and colostrum blends. Immune modulation is needed to prevent autoimmunity and allergies. This involves keeping a balance between Th17, Treg, Th1, and Th2 cells. TFMI showed a greater immune modulation than the other two products, including an elevation of the anti-inflammatory cytokine IL-10 needed for the development of Treg cells. Overall the research showed the efficacy of transfer factors’ supporting a strong immune response along with immune modulation needed to balance the immune system.
Natural Anti-inflammatories
Autoimmune disease is a chronic inflammatory state. Therefore, decreasing inflammation is a critical part of treatment. Inflammation supports the development and the continuation of autoimmune pathology. There are several transcription factors that influence the development of inflammation and can be either pro- or anti-inflammatory. Activation of NFkB and STAT3 both lead to an increase in pro-inflammatory cytokines, inducing Th17. In contrast, activation of the transcription factor Nrf2 leads to an increase in cellular protective responses, including increasing many antioxidants in the body. When researching natural anti-inflammatories, finding herbs and nutrients that impact these pathways has been helpful. Increasing Treg cells to increase immune tolerance is another mechanism to decrease autoimmune disease. Several supplements have been discovered that impact autoimmunity through this mechanism. Below I will discuss some examples of some researched-backed natural compounds that improve immune balance. Other natural anti-inflammatories exist but were excluded due to insufficient research.
Curcumin
Curcumin is one of the active ingredients in turmeric. It is one of the most well known and researched natural anti-inflammatories. By targeting multiple cell signaling molecules, it has many actions in the body. Two of the resulting mechanisms of action from these molecules are active antioxidant and anti-inflammatory effects.7 It has been shown to benefit multiple inflammatory conditions including pain, metabolic syndrome, and chronic kidney disease.7 The primary mechanism of action that has been studied is curcumin’s ability to block the activation of NFkB and therefore the release of the pro-inflammatory cytokine TNF-alpha. NFkB is then activated further by TNF-alpha, creating an escalating inflammatory cycle.8
For the autoimmune inflammation created by elevated Th17 and low Treg cells, curcumin also appears to play a role. Il-23 is one of the main cytokines that induces the formation of Th17 from naïve T cells. Curcumin plays a role in inhibiting the formation of Th17 by selectively inhibiting the production of Il-12 and Il-23 by dendritic cells.9 The transcription factor STAT3 that is related to the development of Th17 is silenced by curcumin.9 In addition to decreasing Th17 and therefore Il-17, curcumin also has a role in increasing Treg cells.10 Research has shown a modulation of the Th17/Treg balance away from autoimmune conditions such as SLE (lupus).(10) Treg cells are the primary producer of the anti-inflammatory cytokine IL-10. Curcumin enhances IL-10, which may be one of its anti-inflammatory mechanisms.11
One of the main drawbacks of curcumin clinically is its poor bioavailability. Much of the curcumin is broken down in the intestine before it is absorbed systemically.12 Many companies have created better absorbed forms of curcumin that have been researched and found to achieve better curcuminoids in the blood stream.12,13 What is important when using curcumin is to dose it appropriately for the form being used for inflammation.
Resveratrol
Resveratrol is a well-known polyphenol. It is best known for its presence in red wine, presumably leading to its benefits. In a manner similar to curcumin, resveratrol has an impact on many cellular pathways. Its anti-inflammatory effects appear to be from its negative impact on NFkB. By inhibiting NFkB, it causes a decrease in TNF-alpha and a subsequent decrease in IL-23, leading to decreased levels of autoimmune stimulating Th17.14 Part of the mechanism of TNF-alpha is to cause a T-cell proliferation, which is inhibited by resveratrol.14
Another mechanism for decreasing NFkB is through the activation of SIRT-1. Resveratrol activates SIRT-1 which deacetylates NFkB.15 Sirtuin 1 (Sirt-1) is a longevity gene related to multiple diseases associated with aging. Its mechanism of action is through a NAD+ dependent protein deacetylase which is how it inactivates NFkB.16 Sirt-1 also has a role as a master metabolic regulator. Resveratrol by increasing SIRT-1 has an anti-aging effect as well as an anti-inflammatory and anti-oxidative stress response.16
Autoimmune disease through activation of Th17 can be stimulated by dysbiosis. Therefore, restoring the microbiome can decrease inflammation, driving an increase in Th17 and a decrease in immune tolerance. In a mouse model of colonic inflammation, resveratrol led to a restoration of the bacterial microbiota in the intestine with a concomitant increase in the short chain fatty acid butyrate.17 This was accompanied by a decrease in Th17 cells and an increase in Treg cells.17 Because of its multiple mechanisms, resveratrol appears to be a good anti-inflammatory and anti-autoimmune supplement.
Quercetin
Quercetin is a flavonoid compound found in many fruits and vegetables. Flavonoids are part of the group of polyphenols that are used in integrative medicine for their antioxidant and anti-inflammatory properties. Quercetin is most well-known for its influence of decreasing histamine levels and IL-4 and IL-5 and therefore allergies.18 It appears to also have a role in autoimmune regulation. It decreases the release of the pro-inflammatory cytokines, IL-6 and IL-1 through inhibition of MAPK signaling.19 A decrease in these pro-inflammatory cytokines leads to a suppression in Th17 and subsequently IL-17 production.20
Another mode of action for quercetin is inhibition of the protein kinase called mTOR (mammalian target of rapamycin). The function of mTOR as a serine/threonine kinase regulates cell growth, cell proliferation and survival, protein synthesis, transcription of proteins and autophagy.21 A new role of mTOR appears to be regulation of T-cell homeostasis.22 There are two different mTOR subunits that together can promote Th1, Th2, and Th17 differentiation.22 When quercetin inhibits both mTOR forms, it decreases Th17 and induces Treg development.20,22 Quercetin helps promote immune tolerance in this way and decreases the tendency towards autoimmunity.
EGCG
Epigallocatechin-3-gallate (EGCG) is a green tea polyphenol with well-known antioxidant and anti-inflammatory effects. It also plays a role in modulation of T helper cell differentiation. EGCG inhibits T helper cell differentiation into Th1 and Th17 cells through impacting their respective signaling transducers and transcription factors.23 It also has a role in increasing Treg cells.24,25 Some of the mechanisms are by decreasing Th-17 associated pro-inflammatory cytokines including IL-1β, IL-6, IL-17A, and TNF-α expressions.25 To do this, EGCG can down regulate the transcription factors STAT3 and mTOR.23 These results suggest that EGCG may improve T-cell-mediated autoimmune diseases.
Probiotics
Autoimmune disease triggered by elevated Th17 is often from dysbiosis or an imbalanced microbiome in the intestine. Severe imbalance with elevated Th17 and its cytokine IL-17 can lead to chronic intestinal inflammation promoting the development of inflammatory bowel disease (IBD).26,27 Probiotics have an anti-inflammatory effect in the intestine through immunomodulation and suppression of Th17 cell elevation.26 Probiotics impact the immune system through several mechanisms including signaling through the Toll-like receptor family.26 Several studies have shown the effectiveness of probiotics in preventing and treating IBD (ulcerative colitis, and Crohn’s disease).27 In addition to decreasing Th17 cells, probiotics along with prebiotics increase Treg cells and therefore immune tolerance.28 With the majority of people now without a normal microbiome, it makes sense as a preventative measure to supplement with probiotics.
Vitamin D
Vitamin D appears to have a role in autoimmune disease. VDR or the vitamin D receptor is present on lymphocytes leading to one mechanism of interaction with the immune system.29 VDR contains many polymorphisms that lead to a difference in risk for vitamin D deficiency. Autoimmune diseases appear to be correlated with vitamin D levels where patients have an increased risk and increased severity of disease with lower vitamin D levels.29
How vitamin D influences autoimmune disease has been researched in several autoimmune diseases. It appears to influence two of the mechanisms of autoimmune development. It can inhibit the differentiation and increasing levels of Th17.30 Through this influence on Th17, vitamin D helped decrease symptom severity in children with asthma.30 Multiple studies have shown vitamin D to have a role in supporting Treg cells.31,32 The higher the vitamin D level, the higher the level of Treg cells leading to improved immune tolerance.
Vitamin A
Vitamin A, like vitamin D, appears to play a role in autoimmunity by modulating the balance of Th17 and Treg cells. Patients with SLE who had lower levels of vitamin A in the blood had higher levels of Th17 cells.33 Retinoic acid is the metabolite of vitamin A that is the key regulator in modulating this balance.33,34 Retinoic acid in the presence of TGF-B promotes the conversion of naïve T cells into Treg cells.35 It also inhibits IL-6 from driving the naïve T cells into the development of the pro-inflammatory Th17 cells.34 Overall the retinoic acid can lead to different differentiation by being an important regulator of TGF-B.34
Summary
With the increasing rates of autoimmune disease, it is important for practitioners to understand the underlying immune mechanisms. Research has consistently shown autoimmune disease to be associated with immune dysregulation. This dysregulation leads to an elevation of Th17 and Th2 with a decrease in Th1 and Treg cells, which creates a cycle of chronic inflammation and infection, perpetuating autoimmune disease. With the understanding of the immune mechanisms underlying this imbalance, we can use our tools in integrative medicine to break this inflammatory cycle.

Dr. Debby Hamilton, MD, MPH, is a pediatrician with experience in primary care, integrative medicine, research, speaking, and writing. Her education includes an undergraduate degree from Wesleyan University followed by a medical degree from Chicago Medical School, where she graduated with honors. She is board-certified in pediatrics, physician nutrition, and integrated/ holistic medicine (AIHM), and has a Master of Science degree in Public Health (MPH). Dr. Hamilton founded Holistic Pediatric Consulting in Colorado in 2005. Her practice focused on treating children with chronic diseases such as autism and ADHD and preconception counseling based on her book, Preventing Autism and ADHD: Controlling Risk Factors Before, During & After Pregnancy. Her book led to her collaboration in the writing of The Healthy Child Guide through the Neurological Health Foundation. She has also contributed chapters for Child Decoded: Unraveling Learning and Behavioral Disorders. In 2017, Dr. Hamilton joined Researched Nutritionals. Her focus is managing and expanding Researched Nutritional’s clinical research on the efficacy of nutritional supplements, working on protocol development, and promoting the education of healthcare professionals.
References
- Viza D, et al. Transfer Factor: an overlooked potential for the prevention and treatment of infectious diseases. Folia Biologica. 2013;59: 53-67.
- Lawrence HS. Transfer factor in cellular immunity. The Harvey Lecture Series 68. New York: Academic Press, 1987.
- Granitov VM, et al. The use of activated transfer factor in the treatment of HIV patients. Jour of HIV, AIDS and Related Problems. 2002; 6(1):79-80.
- Estrada-Parra S, et al. Comparative study of transfer factor and acyclovir in the treatment of herpes zoster. Int J Immunopharmacol. Oct 1998;20(10):521-535.
- Steele RW, et al. Transfer factor for the prevention of varicella-zoster infection in childhood leukemia. N Engl J Med. Aug 14, 1980;303(7):355-359.
- Jensen G. Transfer Factor Multi-immune report, 2018, NIS labs, Klamath Falls, OR.
- Hewlings SJ, Kalman DS. Curcumin: A Review of It’s Effects on Human Health. Foods. 2017;6(10):92.
- Chung SS, Vadgama JV. Curcumin and epigallocatechin gallate inhibit the cancer stem cell phenotype via down-regulation of STAT3-NFκB signaling. Anticancer Res. 2015;35(1):39–46.
- Bruck J, et al. Nutritional control of IL-23/Th17-mediated autoimmune disease through HO-1/STAT3 activation. Sci Rep. 2017;7:44482.
- Handono K, et al. Treatment of low doses curcumin could modulate Th17/Treg balance specifically on CD4+ T cell cultures of systemic lupus erythematosus patients. Cent Eur J Immunol. 2016;40(4):461–469.
- Mollazadeh H, et al. Immune modulation by curcumin: The role of interleukin-10. Crit Rev Food Sci Nutr. 2019:59(1):89-101.
- Douglass BJ, Clouatre DL. Beyond Yellow Curry: Assessing Commercial Curcumin Absorption Technologies. J Am Coll Nutr. 2015;34(4):347–358.
- Jager R, et al. Comparative absorption of curcumin formulations. Nutr J. 2014;13:11
- Silva AM, et al. Resveratrol as a Natural Anti-Tumor Necrosis Factor-α Molecule: Implications to Dendritic Cells and Their Crosstalk with Mesenchymal Stromal Cells. PLoS One. 2014; 9(3): e91406.
- Bagul PK, et al. Resveratrol ameliorates cardiac oxidative stress in diabetes through deacetylation of NFkB-p65 and histone 3. J Nutr Biochem. 2015 Nov;26(11):1298-307.
- Deng Z, et al. The roles of sirtuin-1 and its activator, resveratrol in osteoarthritis. Biosc. Rep. 2019 Apr 17.
- Alrafas HR, et al. Resveratrol modulates the gut microbiota to prevent murine colitis development through induction of Tregs and suppression of Th17 cells. J. Leuikoc Biol 2019 Mar 21.
- Hosseinzade A, et al. Immunomodulatory Effects of Flavonoids: Possible Induction of T CD4+ Regulatory Cells Through Suppression of mTOR Pathway Signaling Activity. Front Immunol. 2019;10:51.
- Mahmoud Hashemi A, et al. Quercetin Decreases Th17 Production by Down-Regulation of MAPK- TLR4 Signaling Pathway on T Cells in Dental Pulpitis. J Dent (Shiraz). 2018;19(4):259–264.
- Kim HR, et al. Quercetin, a plant polyphenol, has potential for the prevention of bone destruction in Rheumatoid Arthritis. J Med Food. 2019. Feb;22(2):152-161.
- Huang Y, et al. Enhancing TFEB-Mediated Cellular Degradation Pathways by the mTORC1 Inhibitor Quercetin. Oxid Med Cell Longev. 2018;2018:5073420.
- Pierdominici M, et al. mTOR signaling and metabolic regulation of T cells: new potential therapeutic targets in autoimmune diseases. Curr Pharm Des. 2011 Dec;17(35):3888-97.
- Wu D. Green tea EGCG, T-cell function, and T-cell mediated autoimmune encephalomyelitis. J Investig Med. 2016 Dec;64(8):1213-1219.
- Yang EJ, et al. EGCG attenuates autoimmune arthritis by inhibition of STAT3 and HIF-1α with Th17/Treg control. PLoS One. 2014;9(2):e86062.
- Li J, et al. Green tea catechins alleviate autoimmune symptoms and visual impairment in a murine model for human chronic intraocular inflammation by inhibiting Th17-associated pro-inflammatory gene expression. Sci Rep. 2019;9(1):2301.
- Tanabe S. The effect of probiotics and gut microbiota on Th17 cells. Int Rev Immunol. 2013 Oct-Dec: 3295-6:511-25.
- Owaga E, et al. Th17 Cells as Potential Probiotic Therapeutic Targets in Inflammatory Bowel Diseases. Int J Mol Sci. 2015;16(9):20841–20858.
- Dwivedia M, et al. Induction of Regulatory T Cells: A Role for Probiotics and Prebiotics to Suppress Autoimmunity. Autoimmunity Reviews. 2016.
- Dankers W, et al. Vitamin D in Autoimmunity: Molecular Mechanisms and Therapeutic Potential. Front Immunol. 2017;7:697.
- Hamzaoui A, et al. Vitamin D reduces the differentiation and expansion of Th17 cells in young asthmatic children. Immunobiology. 2014; 219(11).
- Perezabad L, et al. The establishment of cow’s milk protein allergy in infants is related with a deficit of regulatory T cells (Treg) and vitamin D. Pediatr Res. 2017 May;81(5):722-730.
- Batmaz SB, et al. Seasonal variation of asthma control, lung function tests and allergic inflammation in relation to vitamin D levels: a prospective annual study. Postepy Dermatol Alergol. 2018;35(1):99–105.
- Handono K, et al. Vitamin A improve Th17 and Treg regulation in systemic lupus erythematosus. Clin Rheumatol. 2016 Mar;35(3):631-8.
- Mucida D, et al. Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science. 2007;317(5835):256–60.
- Manicassamy S, et al. Toll-like receptor 2-dependent induction of vitamin A-metabolizing enzymes in dendritic cells promotes T regulatory responses and inhibits autoimmunity. Nat Med. 2009;15(4):401–409.







