Page 1, 2, 3, 4
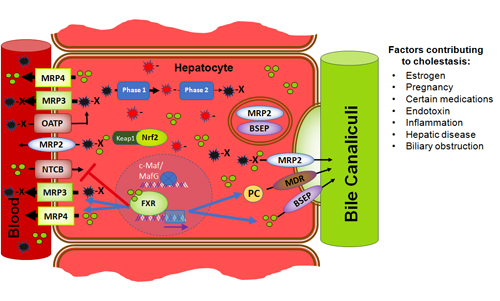
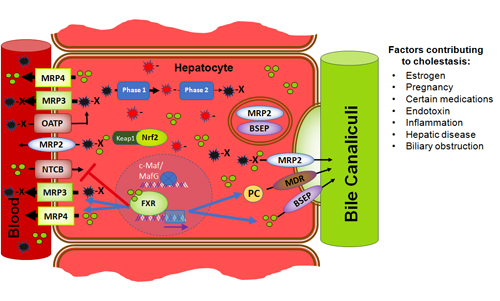
Endotoxin and the associated inflammation leads to glutathione depletion, further contributing to cellular damage as toxins are no longer efficiently transported out of the cells, or protected from oxidative stress.45,46 Exposure to endotoxin and the cascade of inflammatory cytokines it triggers also has the effect of downregulating expression of some of the important CYP enzymes and Phase III transporters.47,48 Endotoxin exposure has a dramatic effect on the urinary elimination of mercury, acting synergistically with the heavy metal to further induce kidney damage.49 Endotoxin also has an effect of rapidly and dramatically reducing bile flow by suppressing expression and function of hepatobiliary transporters (Figure 4b).50
Cholestasis. Bile plays a role in the human body not only for the emulsification and digestion of fatty substances, but also regulates many critical facets of physiology including glucose and cholesterol metabolism as well as thyroid hormone activation.51,52 Along with bile salts, the body secretes cholesterol and phospholipids as well as toxins out of the liver and into the intestines, where they either move out of the body or are reabsorbed via enterohepatic circulation. Bile salts have an impact on the gastrointestinal flora and promote normal gastrointestinal motility.53,54 Because of these many important functions, diminished bile flow can have a serious and broad ranging impact on health.
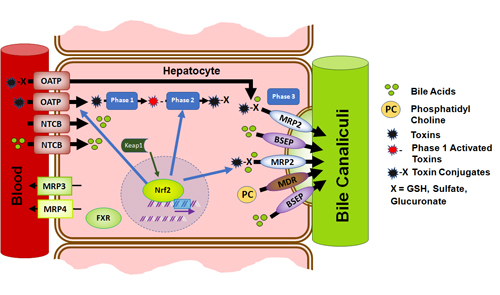
Figure 4a. Normal functioning hepatocyte. FXR remains in the cytosol until activated by bile acids. Oxidative stress causes Nrf2 to dissociate from Keap1 in the cytosol and bind ARE in the nucleus, increasing transcription of detoxification-related enzymes and proteins.
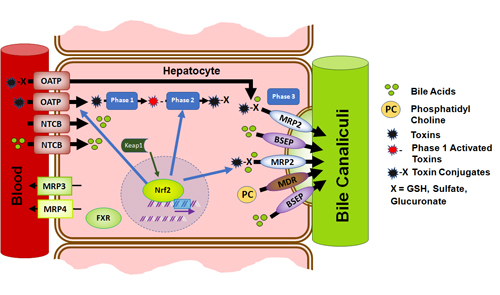
Bile acids are normally secreted from hepatocytes across the canalicular membrane via the bile salt export protein (BSEP), as well as the Phase III transporter MRP2.55 BSEP and MRP2 are from the same superfamily of transporters known as ATP-binding cassette (ABC) transporters, which also includes the Phase III transporters MRP1, MRP3, MRP4, BCRP, and P-gp. Very importantly, BSEP and MRP2 have an interdependent expression, and under normal conditions are colocalized in the apical membrane of the hepatocytes lining the bile canaliculi (see Figure 4a).56 The binding of bile salts to nuclear bile salt receptors, including farnesoid X receptor (FXR),57 pregnane X receptor (PXR),58 the vitamin D receptor (VDR),59 and possibly the xenobiotic receptor, constitutive androstane receptor (CAR),60 increases the expression of transporters for their efflux from the cell, and also regulates their uptake and biosynthesis (see Figure 4a).61
The rate limiting step in bile salt excretion is transport at the canalicular membrane, as there is a high concentration gradient to overcome in order to excrete bile salts into the bile acid pool.62 There are many factors which can inhibit or limit bile acid production and secretion. Substances such as estrogen (in excess), certain medications (including antidepressants), endotoxin, and related inflammatory cytokines are capable of inducing cholestasis by impairing the function of the bile acid transport proteins.63-66 Though often triggered by inflammatory responses, cholestasis also induces an inflammatory response, leading to ROS- and surfactant-induced hepatocyte damage and death due to intracellular bile sale accumulation.67,68 This failure to move bile salts into the bile canaliculus is termed intrahepatic cholestasis.
Cholestasis is toxistasis. With cholestasis, not only is there reduced biliary excretion of bile, but, due to coregulation of BSEP and MRP2, detoxification is impaired as well. There is a reduction of transport of toxins out of the cell by the Phase III proteins, a reduction of Phase II metabolism, and decreased hepatocellular synthesis of GSH, in part due to the blocking of Nrf2 binding to ARE (see Figure 4b).69-71 In cholestasis, a decreased expression of BSEP and the Phase III transporter MRP2 is seen at the canalicular membrane.72 The Phase II estrogen metabolite, estradiol-17β-d-glucuronide (E217βG), triggers internalization of both BSEP and MRP2,73 while LPS causes relocation of MRP2 to the basolateral membrane.74 Each of these factors negatively impacts the ability of the hepatocyte to transport toxins out into the bile. OATP, which serves to transport bile acids and toxins from the blood into the hepatocyte, decreases. An additional protein in the ABC transporter family, MRP3, upregulates in cholestasis, protecting the hepatocytes from toxin-related damage and death.75 However, rather than serving to transport toxins out into the bile canaliculi as MRP2 does, it eliminates them from the cell back into the blood and neighboring cells (see Figure 4b).76 With the additional relocation of MRP2 to the basolateral membrane there are now two pumps moving toxins and toxin conjugates back into the blood during cholestasis. This is likely the mechanism of "detox reactions" or "Herxheimer reactions" experienced during unbalanced detoxification protocols and points to therapeutic interventions to remedy those reactions or prevent them in the first place.
Figure 4b: In cholestasis, there is reduced levels of BSEP and MRP2 at the canalicular membrane due to internalization and relocation. Binding of bile salts to FXR inhibits NTCB transport of bile acids into the cell and increases transcription of BSEP and MRP3 and 4 to lower intracellular bile acid concentration. Nrf2 is blocked from binding ARE by c-Maf/MafG, leading to reduced Phase II inactivation of toxins as well as diminished glutathione synthesis.
The kidney reflexively adapts in attempts to support bile salt removal from the blood in cholestasis by a variety of mechanisms.77 Passive glomerular filtration increases, while at the level of the tubules, active secretion of bile increases, and tubular reabsorption of bile acids is repressed.78 MRP2 is one of the specific proteins that have increased expression in the kidney, protecting the organism by increasing renal bile salt and toxin elimination.79 In severe biliary obstruction, acute renal failure may occur.80 In the intestines, with biliary obstruction, the expression of MRP2 in the enterocytes, where it also serves to transport toxins out, is dramatically reduced.81 The intestinal reabsorption of bile also adapts in cholestasis, as a bile acid transporter that contributes substantially to enterohepatic reabsorption in the duodenum is also downregulated.82
Clinical Manifestations of Cholestasis/Toxistasis
A range of conditions including biliary obstruction, pregnancy, chronic viral hepatitis, cirrhosis, primary biliary cholangitis, and primary sclerosing cholangitis may lead to cholestasis. Cholestasis related to extrahepatic or intrahepatic biliary obstruction is suggested by gastrointestinal symptoms including right upper quadrant pain or tenderness which may be prolonged, epigastric tenderness, discomfort or nausea after meals, and stool changes possibly including evidence of gross fat malabsorption (see Table 1a). Symptoms often are exaggerated with consumption of meals containing a high amount of fat. General or isolated pruritis, localized to the palms or soles of feet, is common, and often worse at night or pre-menstrually in women.83 Depending on the cause of cholestasis, there also may be symptoms of fatigue and impaired memory and concentration.84,85 These symptoms, however, mirror those of toxemia and point to the liver "backfire" (basolateral toxin transport dominating over canalicular transport, Figure 4b) described previously as being causal. Laboratory findings and imaging which may suggest cholestasis are found in Table 1b.
Table 1a: Signs and Symptoms of Cholestasis
Right upper quadrant pain or tenderness
Discomfort or nausea after meals
Pruritis, often worse at night
Epigastric tenderness
Fat malabsorption
Stool changes, especially pale stool
Jaundice
Fatigue
Impaired memory and concentration
Table 1b: Labs and Imaging Suggestive of Cholestasis
Elevated serum aminotransferases86
Elevated alkaline phosphatase, particularly if marked elevation with respect to aminotransferases87
Elevated gamma-glutamyl transpeptidase88
Elevated bilirubin
Elevated 5'-nucleotidase89,90
Elevated serum bile acids91
Biliary sludge or gallstones shown on imaging
A "Push-Catch" Strategy to Maximize Liver Detoxification Pathways
Successful and effective detoxification requires not just support for the phases of detoxification, but also the implementation of a proper directionality to progressively mobilize and eliminate toxins from the cells and tissues, and then from the body as a larger entity. As described previously, much of this is controlled at the canalicular membrane of the hepatocyte; however, it also involves the efficient binding of toxins in the upper GI tract. With a rapid delivery system, such as nanoscale lipid-based deliveries, it is possible to supplement nutraceuticals to support detoxification phases and stimulate bile flow (the "push") and then, within 30 minutes, follow with solid-phase toxin binders (the "catch"). This Push-Catch strategy creates an efficient and discreet detoxification cycle that can be done once per day or can be repeated multiple times per day for more rapid detoxification. Importantly, because of the focus on directionality, "detoxification symptoms" are minimized or eliminated. Though many combinations of compounds can be used, the following are core concepts.
Glutathione Support
Glutathione is central to multiple cell functions, such as detoxification, free-radical control, immune balance, and cell growth. Because glutathione is lost during removal and elimination of mercury and other toxins from the cell, it also can become chronically depleted in settings of toxicity.92 Many conditions such as autoimmune disease,93 chronic infections,94,95 and autism96 are also associated with lower levels of glutathione, which sheds light on why individuals who experience one of these are often extremely vulnerable to additional insults and toxicants.97 Furthermore, liver concentrations of glutathione are five-fold higher than other cells in the body. Glutathione support is thus a cornerstone of detoxification protocols.
Typical oral supplementation of glutathione has low bioavailability, and minimally impacts intracellular levels.98 N-acetylcysteine (NAC), which supports the production of glutathione by providing the precursor L-cysteine, also has limited ability to support intracellular glutathione levels as the conversion of L-cysteine to glutathione is often poor.99-101 Because of this, intravenous glutathione, and alternate oral glutathione delivery forms, such as liposomes and S-acetylglutathione, are often utilized.102,103
Another important mechanism to consider in detoxification protocols is inducing the endogenous cellular production of glutathione and the related antioxidant-supporting and chemoprotective (detoxifying) enzymes and proteins via the Nrf2/ARE pathway (see Figure 2). Sustained activation of Nrf2 has been shown to counteract hepatic injury and bilirubin elevation associated with cholestasis.104 Although Nrf2 is maintained at a basal level, it has a half-life of approximately 15 minutes and is constantly degraded in cells not experiencing stress.105,106 Natural substances that have been shown to induce Nrf2 include lipoic acid (especially the R-form), selenium, diindolylmethane (DIM), sulforaphane, lycopene, milk thistle, and epigallocatechin gallate (EGCG).107-111 Importantly, lifestyle factors also have the ability to affect Nrf2 induction. Activities such as relaxation, breathing techniques, and exercise have the effect of inducing Nrf2.112-114
Page 1, 2, 3, 4 |
![]()
![]()
![]()
![]()