Fraser Smith, MATD, ND
Cardiovascular disease is the number one cause of mortality in the United States and worldwide. The primary target for medical therapy continues to be levels of LDL cholesterol. While the absolute reduction in risk by targeting LDL can be debated, there is compelling evidence that LDL elevations generally increase risk.
But this is not the whole story. There is a powerful, underlying phenomena that accelerates risk; and like many other chronic conditions, it is inflammation. Let’s examine the nature of atherosclerosis as a process and how inflammation really accelerates it. Then, in the second half of this paper, we will look at some key drivers of inflammation. That will include strategies to detect and avoid them and nutritional and botanical considerations to mitigate their effects.
A Fire That Grows
Atherosclerosis is defined as the deposition of lipids into a plaque in the lining of medium-sized arteries. This plaque has an inner core of oxidized LDL as well as unfortunate white blood cells that attempted to scavenge it and died in the process. There is a covering on this cellular debris, this is a conduit of blood flow and kinetic energy, so that body puts a covering of fibrous tissue. Although this keeps the plaque from shearing off and blocking blood flow, this “scar tissue” that covers the plaque of oxidized LDL (cholesterol) and dead cells is never quite the normal inner lining (endothelium) of the artery.1 It remains vulnerable to sucking in more oxidized LDL.
The precise causes of the beginning of this vicious cycle are not fully known. Oxidative stress in the vicinity of the arterial endothelium, in younger years, can cause it to dysfunction. High circulating LDL makes LDL invasion of the artery more likely. Oxidation of LDL makes it a more dangerous particle.
Inflammation is the central phenomenon. In the case of atherosclerosis, a positive feedback loop emerges. Typically, in the regulation of the body’s systems, we see lots of negative feedback loops, but not positive. A negative feedback loop can be like thyroid hormone: Levels of thyroid hormone drop, the pituitary releases factors to get the thyroid to make more, as levels of thyroid hormone rise, the pituitary makes less thyroid stimulating hormone. This is how a control system works.
In atherosclerosis, a cycle of events feeds forward and reinforces itself. Oxidative stress damages tissue and damages the LDL particle.1 The LDL particle migrates to the arterial intima (inner lining). The immune system attacks. More inflammation means more damage. The damaged tissue is more susceptible to LDL penetration. Higher inflammation means more damage to LDL, and so on.
It is possible that inflammation is not the ultimate root cause. Perhaps a conflagration of factors simply set in motion a vicious cycle. New lines of research examine the phenomenon of “efferocytosis,” which means to remove dead matter. In the human body, cells die constantly. The immune system, mostly through scavenger cells, removes these dead cells. In the lining of an artery undergoing atherosclerotic changes, the toxic matter (oxidized LDL) and the dead scavenger cells that went in to ingest the toxins and never came out, somehow remain embedded in the tissue. This sets up recurring and unwanted attention from immune cells, who ramp up the inflammation and yet cannot completely resolve the problem. An analogy would be a splinter or foreign body that causes an abscess where the body simply cannot expel it.

While future treatments for atherosclerosis may zero in more and more on immune phenomena and the failure of macrophages to carry out effective efferocytosis, there is no doubt that increased inflammation is no mere symptom. It helps accelerate the disease process. When inflammation is high, that indicates a higher risk of atherosclerosis progression.
The naturopathic medicine approach to inflammation in this case involves the following:
- Address the determinants of health, which includes removing toxic exposure or disturbances.
- Make dietary changes to modulate the inflammatory response and support normal function.
- Have the patient engage or use practices that support overall health, such as stress reduction, acupuncture, cardiovascular exercise.
- Use specific natural medicines to reduce inflammation and to improve the integrity of the arteries.
With a view to “A,” let’s examine some, but certainly not all, of the factors that can drive inflammation.
The Fuels That Drive Inflammation
Arsenic: A variety of pro-inflammatory toxins can either damage the lining of the artery or accelerate inflammation. A prime example is arsenic, which is known to pathologists as a toxin to the cardiovascular system.2 It can increase the risk of death from heart attacks and accelerate atherosclerosis. Arsenic causes a burst of oxidative stress in the body, damage to DNA and mitochondria, and oxidation of LDL.2,3 Groundwater in many parts of the United States exceeds the EPA allowed level of arsenic; and since well water is not regulated, some sources are quite high in arsenic.4
Processed Vegetable Oil: For years, health authorities urged people to substitute “bad” animal-sourced fats with vegetable oil. That would be good advice if the vegetable oil in question were pure, undamaged, and chock full of its natural antioxidants and sterols. Unfortunately, the vegetable oil that crowds the shelves and makes up most of the cooking oil in America’s very busy restaurant industry is pro-atherogenic.5
This issue is somewhat fraught, as there is positive evidence that polyunsaturated fatty acid (PUFA) substitution for saturated fats can help prevent heart disease. The problem is the heating and chemical solvents during extraction, the bleaching to provide a neutral taste, and the fact that they are often overheated in both commercial frying and home use.
When PUFAs are oxidized, they form a number of free radical propagators, such as lipid hydroperoxides, that can increase inflammation in the artery.6-8
Plastic Byproducts: Linked to cancer, plastic conditioning agents, such as bisphenol A are also linked to atherosclerosis. More of this evidence is, for now, in animal research models, like most toxicology information; but it appears that the damage to arteries is real. Interestingly, in test animals, the BPA-exposed rabbits developed more insulin resistance, obesity, and fatty liver.9,10 This shared traits with “metabolic syndrome” as we see it in humans. Moreover, plasticizers have been found to be “obesogens” that can promote obesity in humans.11 They do this by increasing resistance to insulin but also by causing fat cells to proliferate.
Stress: The most general and pervasive phenomenon, stress, can energize us in the right amounts and act to exhaust and prematurely age us in larger exposures. This is especially true in situations where we cannot escape stressful situations that we cannot accept. A combination of metabolic syndrome, obesity, and stress can be particularly atherogenic.12
Air Pollution: Although the connection between particulate matter, ozone, and other forms of air pollution to lung disease is clear enough, this source of toxins can also accelerate atherosclerosis. The calcification of arteries that is associated with progressing atherosclerosis was found to be correlated with air pollution exposure in over 6700 adults in six US metropolitan areas.13
Periodontal Disease: Chronic gum disease that progresses to deeper infection and inflammation can raise inflammation across the body. This is because there are pockets of bacteria that can be held in check but not completely removed. This serves as a constant provocation of the immune system, which causes white blood cells to release higher levels of inflammation activating signals. This inflammation can definitely increase cardiac risk.14 It has also been found that chronic periodontal disease activates certain inflammasomes, proteins that are part of our basic innate immune response that can mount non-specific but powerful responses to invading bacteria. Inflammasomes can, in turn, activate enzymes that cause increases in signals that fire up immune cell activity.15,16
Dousing the Flames
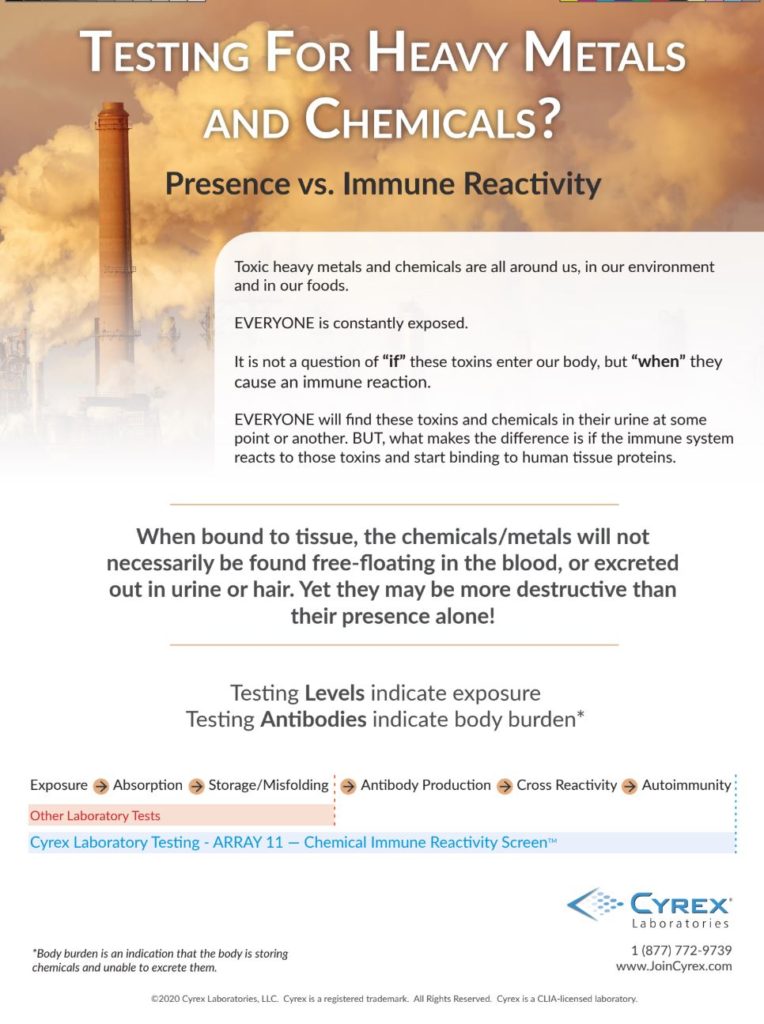
It is clear from just examining a few common examples of pro-inflammatory influences that a concerted effort to identify and reduce (or eliminate) pro-inflammatory influences is needed for many, many people. This may seem daunting or even hopeless, but intelligent changes can pay off. For example, an efficient filter for drinking water as well as some regular testing can help reduce heavy metals. Purchasing healthy “cold pressed” plant oils and not overheating olive oil when cooking can reduce vegetable oil toxins. Additionally, reducing restaurant visits can cut off much of these unhealthy oils at their source.
The work of reducing our risk exposures can seem to incite more and more effort, longer and longer “to-do” lists, and a lot of expense, an approach that can simply increase stress. On the contrary, simplifying our life with slower eating, natural eating, and a growing awareness of what is healthy and natural and what is synthetic and potentially harmful can take root. Not all societies are as driven and as out of touch with the rules of healthy living as ours. So, while it takes an effort to make changes, over time a lot of health-promoting practices that properly address the determinants of health can become the new normal.
There are divergent approaches to healthy eating and individual variances in genetics and biochemistry. It is a safe bet for practically everyone to emphasize plant foods in their diet.17 While advice from conventional health sources (such as the American Diabetic Association as one example) are putting the concept of a plate loaded with plant foods out there, the actual practice in our society has some catching up to do. Processed foods, restaurant foods, and a loss of cooking skills in some homes has taken its toll. Still, the resurgence in interest in cooking, the growth of interest in natural foods, organic and non-GMO foods, and locally sourced foods gives reason for hope.
It should be noted here that there are specific tests that can help identify cardiovascular inflammation.18 A common one is C-reactive protein, which many internists will be happy to order. But there is much, much more on the menu and integrative physicians are often quick to take advantage of this insight and would do well to do so.
Nature’s Fire Brigade
It should be clear that merely throwing supplements at atherosclerosis risk, in particular the unseen but relentless inflammation in the arterial inner lining is no solution. Addressing the determinants of health can never really be bypassed. Nevertheless, supplements, plant extracts and nutrients can do a lot of good. A few examples are the following:
- Curcuminoids from turmeric can interrupt inflammation at multiple points.19
- Grape seed extract and other sources of procyanidolic oligomers (including many berries) can strengthen the lining of the arteries and reduce oxidative stress.10
- Culinary herbs and spices, such as pepper, ginger, garlic, onion, cinnamon and chili, are packed with polyphenolic molecules and other useful compounds that can slow disease progression.20
- Magnesium deficiency, a double digit and widespread phenomenon, can undermine the cardiovascular system. Magnesium can strengthen the arterial structure, make vessels more elastic and flexible, and promote the synthesis of protective antioxidant enzymes in the cell.21
Conclusion
Patients need a very complete inventory of the disturbances to the determinants of their health in order to lower their atherosclerosis risk. Changes to lifestyle, diet, and the use of the very best of nutrients and herbal medicines can change the physiology and inflammation of their arteries and their body as a whole. These changes cost very little and can pay dividends across time.
References
- Wu MY, et al. New Insights into the Role of Inflammation in the Pathogenesis of Atherosclerosis. Int J Mol Sci. 2017;18(10):2034.
- Kuo CC, et al. The Association of Arsenic Metabolism with Cancer, Cardiovascular Disease, and Diabetes: A Systematic Review of the Epidemiological Evidence. Environ Health Perspect. 2017;125(8):087001.
- Jomova K, et al. Arsenic: toxicity, oxidative stress and human disease. J Appl Toxicol. 2011;31(2):95–107.
- Mayer JE, Goldman RH. Arsenic and skin cancer in the USA: the current evidence regarding arsenic-contaminated drinking water. Int J Dermatol. 2016;55(11):e585–e591.
- Spiteller G, Afzal M. The action of peroxyl radicals, powerful deleterious reagents, explains why neither cholesterol nor saturated fatty acids cause atherogenesis and age-related diseases.Chemistry. 2014;20(46):14928–14945.
- Ng CY, et al. Heated vegetable oils and cardiovascular disease risk factors. Vascul Pharmacol. 2014;61(1):1–9.
- Mboma J, et al. Effects of Cyclic Fatty Acid Monomers from Heated Vegetable Oil on Markers of Inflammation and Oxidative Stress in Male Wistar Rats. J Agric Food Chem. 2018;66(27):7172–7180.
- Spiteller G. The relation of lipid peroxidation processes with atherogenesis: a new theory on atherogenesis. Mol Nutr Food Res. 2005;49(11):999–1013.
- Fang C, et al. Bisphenol A exposure induces metabolic disorders and enhances atherosclerosis in hyperlipidemic rabbits. J Appl Toxicol. 2015;35(9):1058–1070.
- Rameshrad M, et al. Bisphenol A vascular toxicity: Protective effect of Vitis vinifera (grape) seed extract and resveratrol. Phytother Res. 2018;32(12):2396–2407.
- Janesick AS, Blumberg B. Obesogens: an emerging threat to public health. Am J Obstet Gynecol. 2016;214(5):559–565.
- Ortega-Montiel J, et al. Self-perceived stress is associated with adiposity and atherosclerosis. The GEA Study. BMC Public Health. 2015;15:780.
- Kaufman JD, et al. Association between air pollution and coronary artery calcification within six metropolitan areas in the USA (the Multi-Ethnic Study of Atherosclerosis and Air Pollution): a longitudinal cohort study [published correction appears in Lancet. 2016 Aug 13;388(10045):660]. Lancet. 2016;388(10045):696–704.
- Hamilton JA, et al. Atherosclerosis, Periodontal Disease, and Treatment with Resolvins. Curr Atheroscler Rep. 2017;19(12):57.
- Yilmaz Ö, Lee KL. The inflammasome and danger molecule signaling: at the crossroads of inflammation and pathogen persistence in the oral cavity. Periodontol 2000. 2015;69(1):83–95.
- Yamaguchi Y, et al. Activation of the NLRP3 inflammasome in Porphyromonas gingivalis-accelerated atherosclerosis. Pathog Dis. 2015;73(4):ftv011.
- Tuso P, Stoll SR, Li WW. A plant-based diet, atherogenesis, and coronary artery disease prevention. Perm J. 2015;19(1):62–67.
- Smith, F. Faydenko, J. Cardiac Biomarkers: A Well Validated Clinical Management Tool. Townsend Letter. May 2019;490.
- Li C, et al. Curcuminoids: Implication for inflammation and oxidative stress in cardiovascular diseases. Phytother Res. 2019;33(5):1302–1317.
- Tsui PF, et al. Spices and Atherosclerosis. Nutrients. 2018;10(11):1724.
- Kostov K, Halacheva L. Role of Magnesium Deficiency in Promoting Atherosclerosis, Endothelial Dysfunction, and Arterial Stiffening as Risk Factors for Hypertension. Int J Mol Sci. 2018;19(6):1724.