by Hal S. Blatman, MD
I played golf with sharp and disabling lower back pain for twenty-five years before I learned how to make it go away. Trigger point injections and myofascial work always helped; but when I learned about inflammatory food, there came my first almost pain-free nine holes. Then with platelet-rich plasma, prolotherapy, and repairing tendon injuries, I can hit golf balls as hard as I want with no pain on any swing…unless my food is contaminated with gluten… and then I am in pain for three weeks.
Twenty years ago, I walked off the tennis court with pain in my knees that was bad enough to prevent running and reaching to hit a ball. With what I researched and learned, my bow-legged knees were pain free in six months and without surgery can still ski black diamond mogul slopes and bend to play tennis.
Do you know someone, have a patient, or do you yourself suffer with chronic pain? How many practitioners have been seen, and how many therapies have been tried? Perhaps surgery has been suggested and even already performed.
What do you do if there is a paper cut on your finger and it is bleeding? Options include emergency room for the severity of bleeding, take some ibuprofen and wait until morning, or apply pressure to stop the bleeding. This answer is pretty simple. So what if your back or knee hurt after a game of tennis? Options again include emergency room, taking ibuprofen and waiting until morning, and what if you could apply pressure somewhere and make the pain go away? In actuality, this is more than possible and thoroughly changes how I think about pain and its treatment.
One of the unfortunate phenomena in medicine is that the doctor recommending your treatment, and perhaps even surgery, has likely never really touched you. A pain patient’s examination and recommendations are typically based on X-ray, CT scan, MRI scan, and perhaps other diagnostic studies.
Indeed, finding these clues of what causes pain requires a different kind of physical examination than what doctors and health care providers are usually taught. It’s not the stethoscope, x-ray, MRI, or pin prick test, but rather a gentle and specific touch that provides many of the necessary clues.
How can we discover the location of these important clues to a lifetime of pain-causing injuries?
 Pain educators discuss a familiar theme with regard to what is called chronic and intractable pain. Practitioners and the public have been taught that acute pain comes from injury, and that if this pain persists longer than three-to-six months it becomes “chronic pain” and then it is unlikely to ever go away. Current medical treatment of chronic pain then becomes variations of making the nervous and immune systems less active. Among other choices, this can be accomplished with medications such as cortisone, gabapentin, and opiates, electrically with TENS and spinal cord stimulators, and surgically with radio-frequency and other nerve ablation procedures.
Pain educators discuss a familiar theme with regard to what is called chronic and intractable pain. Practitioners and the public have been taught that acute pain comes from injury, and that if this pain persists longer than three-to-six months it becomes “chronic pain” and then it is unlikely to ever go away. Current medical treatment of chronic pain then becomes variations of making the nervous and immune systems less active. Among other choices, this can be accomplished with medications such as cortisone, gabapentin, and opiates, electrically with TENS and spinal cord stimulators, and surgically with radio-frequency and other nerve ablation procedures.
Pain education also teaches that nociceptive and neuropathic pain are distinguishable by the quality of pain symptoms. This doctrine ascribes different pathology to sensations of burning, numbness, aching, and stabbing. In addition, it is suggested that these various sensations of pain might be more effectively treated with different modalities and by different medications, or even that some are not treatable by one type of medication or another. Symptoms are presumed to be indicators of origin, ascribing specific etiology for burning, tingling, sharp, dull, achy, and more. Practitioners spend a lot of time documenting the nuances of sensation because they have been taught that this is of diagnostic significance.
These theories of pain biology and physiology have a foundation in spinal anatomy, knowledge of dermatomes, joint dysfunction, and understanding of nervous system plasticity and windup or up-regulation. All these ideas have been substantiated by anatomical study.
While the anatomy behind pain theory based on current understanding of neuropathic and nociceptive pain is not disputed here, many of the conclusions that traditionally follow are based on assumptions that may not be correct.
Janet Travell, MD, seemed to understand that a great preponderance of what we perceive as pain originates in fascia. She described myofascial trigger points in fascia causing sensations of discomfort that vary to include numbness, tingling, burning, and pain.(1)
A new understanding of anatomy and fascia based on the work of van Der Was J (2009),(2) Langevin et al (2009),(3) Schleip,(4) and others leads to new ways to work with healing chronic pain.
Review of Anatomy
Anatomy and physiology teach that feedback to the central nervous system comes largely from Golgi tendon organs, Pacinian corpuscles, and Ruffini nerve endings. Anatomical studies have supported this teaching to students of medical physiology for many years. While these mechanoreceptors are important, anatomically they represent only 20% of afferent information to the brain. Approximately 80% of afferent information about our periphery comes from free nerve endings that terminate between the cords and fibrils of fascia throughout the body. These are small diameter interstitial muscle/ fascia receptors, 90% of which are unmyelinated free nerve endings. The majority of these are for mechanical tension and pressure.(5) This would include muscle, organs, and all of what is considered “soft tissue.” Some of these nerve endings are for chemo and thermo reception, but the vast majority measure pressure and friction (shear forces). Research has shown that it is these nerve endings that originate much of the input from which we interpret both proprioception and myofascial pain. Indeed, the interaction of these nerve endings and fascia becomes the antenna for our brain to understand its periphery.
The significance of this anatomy is that the vast majority of afferent information to the brain is providing feedback about pressure and sheer force within the collagen fibrils of fascia. This would include tendon, ligament, enthesis, muscle, and even the bladder wall. As an example, as the bladder distends, the fascia and bladder wall also become thinner. These interstitial nerve endings interpret this pressure change and shear of expansion as “I have to pee,” or perhaps the pain of what we call “interstitial cystitis.” The balance of homeostasis is part of what keeps our nervous system thinking urination vs urinalysis and antibiotics.
As an orthopedic surgery resident in 1980 we were taught that proprioception of joint position came primarily from “goniometer nerves” in the joint. We know now that this is not true, and that instead these free nerve endings in fascia provide the input that becomes proprioception. We also know that receptors in skin are more important than receptors in joints. When a joint moves, information about this movement comes from fascia shear being different on the extensor and flexor sides of the joint. As we mature from infancy through our early years, our brain learns how to integrate this information and provide the data for understanding where we are in space.
Many people speak about a concept called muscle memory. In actuality, muscles are not capable of memory, and don’t remember anything. They are simply bound muscle cells that only have the ability to turn on and turn off. Instead, it is fascia holding these cells together that remembers everything. Some feel that fascia remembers every bump and twist a body ever takes. Therapists speak of somato-emotional release as a phenomenon where fascia releases and the emotions, tied to the trauma, release simultaneously with pain. A close relative of this are the theories and concepts of “interoception.” Much of the CNS neuroinput from these free nerve endings in fascia terminates in the posterior insula of the brain before reaching the cortex. This primate-only area of brain anatomy integrates emotion into our perception and reality.(6) Perhaps we know how we feel about being injured even before we recognize what happened.
 With consistency we observe acute injury causes acute pain that can lead to chronic pain. Statistics on resolving chronic pain show that if acute pain is not resolved by three to six months after injury, it becomes chronic pain that can likely never go away. We are also taught that our bodies become tolerant to opiate medication and doses might need to be increased over time. While these ideas represent the reality of current medical understanding, they are not the reality of our biology. While acute pain may lead to chronic pain, this chronicity only continues until the injuries that caused it are found and healed. The months or years spent in pain do not matter as much as we might think. In fact, much of the paradigm of how pain is considered, examined, and treated today does not work as well as it should if it were correct. If it were correct, wouldn’t treatment be more successful? Don’t doctors say they will try this, and if it does not work then try that, and so on? Perhaps figuring out the answer shouldn’t take so many tries if our understanding is mostly correct.
With consistency we observe acute injury causes acute pain that can lead to chronic pain. Statistics on resolving chronic pain show that if acute pain is not resolved by three to six months after injury, it becomes chronic pain that can likely never go away. We are also taught that our bodies become tolerant to opiate medication and doses might need to be increased over time. While these ideas represent the reality of current medical understanding, they are not the reality of our biology. While acute pain may lead to chronic pain, this chronicity only continues until the injuries that caused it are found and healed. The months or years spent in pain do not matter as much as we might think. In fact, much of the paradigm of how pain is considered, examined, and treated today does not work as well as it should if it were correct. If it were correct, wouldn’t treatment be more successful? Don’t doctors say they will try this, and if it does not work then try that, and so on? Perhaps figuring out the answer shouldn’t take so many tries if our understanding is mostly correct.
Injuries that result in chronic pain are usually many years old and started in childhood. It is not lifting the box that started what is causing the lower back pain. It is likely to be old injuries that weakened the fascia which gave way during the lifting injury resulting in years of pain. Then the pain results when the tissue becomes even more fragile and injured. In our experience, seldom is chronic pain truly intractable. Instead, with finding and helping the body to heal from these old and new injuries, significant levels of pain can indeed be made to go away much of the time.
While theories of acute and chronic pain, inflammation, nociceptive and neuropathic pain, electric stimulator modulation, and pharmaceutical interventions have their place, our research shows that much of this is not our biologic reality.
When a patient presents asking for evaluation of pain, the practitioner is being asked to play CSI for pain. A diagnostic medical “who done it.”
In diagnosing and treating chronic pain, our research has led to conclusions that form the basis of the Blatman Method-Five Rules of Pain CSI®:
1. You, as the patient, cannot believe the pain you experience comes from where you feel it.
2. You also cannot believe what you think the pain feels like, and the distinction is not diagnostically important.
3. The most significant thing you can believe is that where you are specifically tender, mm by mm, is where your fascia is tied in a knot, or where your fascia attaches to you, holds you together and is injured.
4. The specific sites where you are most tender are the locations of pain generators in your fascia that generate most of the pain you feel.
5. If you can get your body to heal the specific places that are this tender, a large amount of the pain you experience will go away.
Amazingly, as resistance and allegiance to what we have been taught will draw you away from these rules, results of following them lead to amazingly consistent results and help answer questions from years of practice. And fortunately, this paradigm applies to healing from most pain in the body – most of the time.
Some of the various pain conditions where this directly applies include migraine and headache, neck and shoulder pain, arthritis and joint pain, lower back pain, leg and foot pain, interstitial cystitis, pelvic pain, plantar fasciitis, TMJ syndrome, and fibromyalgia. It also applies to muscle and ligament strains and sprains from sporting injuries. Indeed, condition of fascia is at the core of most injury, at the core of most pain issues, and at the core of orchestration of real healing. Not just physical, but also emotional as referred to by interoception.
Let’s discuss each of the five rules. Referring to Rule 1, you cannot believe the pain comes from where you feel it. Headaches do not come from your head. The pain in your left arm could be from your heart attack. You as the patient have little idea and know only that the pain is in your head or arm. Similarly, why do you think that knee pain comes from the knee, or low back pain comes from the lower back, or even that foot pain comes from the foot or heel spur. One of the more impressive examples is the person who has had total knee replacement surgery, and still suffers perceiving pain in the replaced knee joint. Indeed, pain attributed to a joint may not be coming from the joint itself but rather from the myofascia that holds the joint together and makes it move.
Referring to Rule 2, it is not so important what you think the pain feels like. This issue has been an amazing education. It started with Dr. Travell teaching that myofascial trigger points caused sensations of radiating numbness, tingling, aching, cramping, and pain. During examination and pushing on trigger points to impress a patient these ideas, often the radiating pain would be a mixed sensation of numbness, burning, and pain. This may be why some pain symptoms are so difficult to describe. Keeping my personal faith in helping the body heal the most tender of its fascia injuries, I utilized platelet rich plasma injection therapy to treat injured gluteal tendons in a chronic low back pain patient. This man had a history of lumbar fusion surgery 10 years prior and suffered persistent pain and also numbness to the bottoms of his feet. Upon return a month after his procedure, he reported that since two days afterwards and for the first time in 10 years, he had been able to feel his dog lick the bottoms of his feet. Doesn’t this mean that numbness does not have to originate in spine and nerve pathology? Numbness and tingling are consistent phenomena that are not explained by nerve, dermatome, and spine theories of pain. They are best understood as symptoms of fascia injury and repair.
Referring to Rule 3, if you cannot believe where you hurt or where the pain comes from, this rule is about what you can really and truly believe. Indeed, the only thing you can believe as a patient is that where you are specifically tender, mm by mm, is where the fascia strings and cords that attach to you and hold you together are either tied in a knot or they are injured.
Referring to Rule 4, the specific places where your body and fascia are most tender usually relate to the most significant of the injuries causing the pain symptoms that are more likely to attract your attention. It’s fascinating that this seems to be true no matter what turns out to be your pain issues of affliction – from headache to foot pain and all areas in between. Examine very carefully and trust what is tender.
 Referring to Rule 5, when you can get your body to heal from the injuries discovered during the physical examination of Rule 3, you will find the pain from Rule 1 will mostly or possibly even completely go away. This means that coping skills, medications, epidural steroids, nerve blocks, neuro-ablative procedures and more might not be so necessary if we could only make the pain go away nearly all of the time. And indeed, there is a path which you can work to make this happen.
Referring to Rule 5, when you can get your body to heal from the injuries discovered during the physical examination of Rule 3, you will find the pain from Rule 1 will mostly or possibly even completely go away. This means that coping skills, medications, epidural steroids, nerve blocks, neuro-ablative procedures and more might not be so necessary if we could only make the pain go away nearly all of the time. And indeed, there is a path which you can work to make this happen.
One of the issues of treatment for chronic pain is that the practitioner or doctor prescribing your medication and surgery has likely never really touched you. Your chiropractor has to some extent, massage therapist has perhaps more, but who else? Success from this work and understanding of injury and pain depends on knowing a touch that is not taught in medical school. And then, an understanding of what that touch means to healing injury and resolving pain.
What about treatment? Besides basic stretching, has anyone taught you how to work on and change the “kinks” in your myofascia? And are you doing this a few times each day?

Every muscle and fascia injury has three physical engineering issues. First there are injuries where the fascia weaves to the periosteum weakening the attachments that anchor muscle. These injuries can also be anywhere along the fascia cords between anchor (enthesis) and trigger point. Second, there are the actual places where the fascia cords and muscle cells are wound into the trigger point. This actual coil is not only tender when palpated, it is directly responsible for much of the tightening that causes the ropey bands and is also responsible for generating much of the noticed discomfort or pain as it applies pressure to the interstitial nerve endings. Lastly, there is the ropey band. The significance of the ropey band is that it has to impede blood flow. This will mean the muscle will then necessarily start to burn fuel anaerobically long before it normally should. At this point, continuing to use the muscle will increase formation of lactic acid as ATP is made. The consequence is that with more use of tight muscles, the more a person will have to massage or use their foam roller to squeeze metabolic exhaust from the ropes just to keep up. See Figure 5.
Trigger points and fascia kinks need to be smoothed out so the nerve endings in-between the fascia cords stop being squeezed and causing symptoms. Sometimes the injured enthesis and fibers in the muscle cord require repair so that muscle pull can be more solid without recurrence of the kinks (trigger points).
For more than 25 years I have taught about massaging trigger points and fascia with a rubber ball. This ball can reduce concentration of metabolic toxicity within a muscle, and also help untangle the wound up knots of fascia called trigger points. Fascia-based pain patterns from these knots are illustrated along with rubber ball massage and stretching techniques in my book, Winners’ Guide to Pain Relief, Danua Press.
Trigger point injections and dry needling induce the fascia knots to directly unwind. Discomfort from this treatment is from the free nerve endings sensing the ripple along the fascia that results from the release. Afterwards the person will likely feel soreness of a muscle that finally has a chance to relax after too much exercise.
What about joint pain? Doesn’t it come from arthritis? Many are advised that their bone on bone joint will require replacement surgery. Orthopedic texts state that we are born with cartilage to wear out and when this happens ourjoints require replacement. In a body that grows a new gut lining every three days, new skin every 7-10 days, and even new brain cells, it does not make sense that our body cannot repair cartilage from daily wear and tear. A closer truth is that we regrow cartilage in every joint in our body every minute of every day, and there are alternatives to joint replacement surgery.
One of the first questions to ask is about how well the joint still moves. If you can fully straighten your knee and also bend it 100°, there is no possible way this joint is bone on bone. Moreover, the joint has enough cartilage remaining to not only move, but also there is a good chance of regenerating and avoiding replacement surgery.
There are surgeons who call joints bone on bone to persuade patients to proceed with replacement surgery. Some x-rays I have seen in second opinion consultation have more joint space than mine. Even when cartilage is very thin and the x-ray may look like bones are very close together, it only takes two to three cell layers of cartilage for a joint to move. Seeing cells requires a microscope, and this thin layer cannot be seen by x-ray.
What then of the pain? Again, much of our pain comes from injury demarcated by where the fascia is tender. With regard to knees, nearly all people have tender injuries in their pes anserine tendons and the insertions of distal vastus medialis muscles. Not only do these patients need to regenerate cartilage in their joints, these fascia injuries also need repair. And it is often injury to these structures that is the basis for chronic knee pain after joint replacement surgery.
What about food and its effect on fascia and pain? Of all therapeutic challenges, this simple issue is one of the more complicated to work with and motivate people for change. Many of the answers however, are much more straight forward.
When injury occurs at the enthesis and throughout the muscle as fascia cords get stretched and torn, inflammatory mediators are released. It has been shown that 90 seconds of osteopathic touch can change this chemistry and reduce the inflammatory soup in the local tissue.(7)
In a similar fashion, exposure to inflammatory food also increases the release of inflammatory mediators by the fibroblast diffusely and throughout the body.(8) In the central nervous system this has been shown to increase cerebral injury.(9) In the body this fascia inflammatory response increases pain.

Where pain comes from interstitial nerves reacting to injuries in fascia, in my experience inflammation from food and environmental toxicity makes these injuries light up like a holiday tree for days to weeks. According to our research, being able to sense pain from weather and barometric change implies a fasciawide level of inflammation caused by some ingested food during the previous six weeks. The corollary is that in the absence of any food inflammatory to your body through six weeks, most likely you will not feel “rain pain,” or it will be much lighter than expected and you are looking to discover another sensitivity.
Of equal significance, if the fibers of a ropey band can be separated by a treatment, they will stick back together by the inflammation from food. Indeed, success of myofascial treatment is intimately tied to nutrition and environmental toxicity.
There are many practitioners and treatments for chronic issues. Many are helpful to people who suffer and much has been written. Common denominators of successful treatments can often be found in fascia and nutrition.
There are many diets and nutritional philosophies that have been helpful for those with chronic issues. In figuring this out, it is helpful to know our body speaks with a common and particular language. If one wakes in the morning with pain not present the night before, and there was no intervening injury, a highly likely cause of this increased pain is inflammation from food ingested the evening before. A stiff neck does not come from the window, and it is unlikely for anyone without Ehlers-Danlos syndromes to sleep that wrong. It is more likely the sudden pain issue came from last night’s pizza and a high dose of inflammatory bread flour and dairy. Similarly, pain in the evening may have come from breakfast or lunch.
At heart to the issues of chronic pain is that current treatment does not work very well. In addition, reliance on opiates and other medications has not proven to be such a good option. Surgery remains controversial, with success and failure less than predictable. And pain treatment is often based on epidural steroids and ablative procedures that may be harmful.
Alternative medicine pain clinics offer acupuncture, mind-body-spirit, herbal medicine, and training in coping skills. This article discusses a different paradigm…that of finding and healing the injuries and watching the pain go away. Really, please, why don’t we learn to just make it go away!![]()
In my experience after 30 years of research, pain is not what we are taught. It is not about inflammation, disc, spine, or even joint. Indeed, all of this can be in the mix, but the predominant injuries are to the fascia that holds our bodies together. The very tissue we were taught to discard during anatomy and also surgery is more important than ever imagined.
The miracles of healing bring us the ability to repair from old injuries and also to regrow worn cartilage in our joints. Many of us have patients who are living proof. No one should be led to think their cause is hopeless. So many people who suffer with chronic pain can be helped to function better and with much less discomfort.
To feel better and better, locate and help heal the pain generators caused through time, stop all ingestion of inflammatory food, and then consider your next steps. Practitioners of regenerative medicine, detoxification, ozone therapy, nutrition and myofascial pain may be a good choice for information and help.
If you are a practitioner, learning new ways to consider common problems of pain will help you be more able to help people with frustrating issues where there are otherwise too few good options.
◆
A Case Report:

Patient XX is a 62 year old woman who presented on June 17 with a history of scoliosis and pain in her neck, back, hip, and leg on the right side. She had felt a pulling sensation in her psoas muscle during yoga about 1 year prior, and then again while doing a Rumba dance about 5 weeks prior to this office visit. She had one acupuncture treatment and then more recent activities with her grandchildren greatly aggravated her symptoms.
Health care professionals have been taught to think this pain could likely be related to her history of scoliosis and x-ray findings of degenerative lumbar facet changes. Her presenting pain pattern is illustrated in fig. 1.

With only myofascial release, use of rubber ball massage techniques as described in “Winners’ Guide to Pain Relief,” and nutritional changes her condition improved and she presented on July 2 with the pain pattern illustrated in figure 2.
This is representative of improvement in most all chronic pain patients 4 weeks after myofascial work with rubber ball, and a gluten free non-inflammatory diet. Even before injection or needling therapies, simple food changes and self massage techniques have already made a significant difference.

Working with the 5 rules of the Blatman Method of Pain CSI, trigger point injections resulted in significant and rapid improvement demonstrated by the pain diagram colored on July 12, see figure 3, on the right.
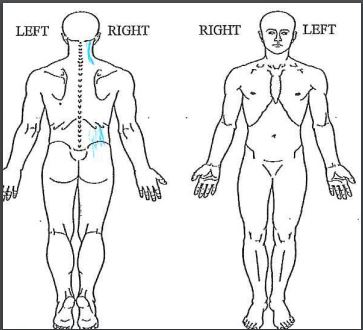
And then after more of the same treatment: figure 4, below, is from August 16.
Summary
This patient presented with disabling pain involving the right side of her body from neck to thigh. She had seen another physician, experienced some acupuncture, and had an MRI scan of her lower back. The MRI scan illustrated scoliosis and arthritic changes that included facet arthropathy L2-S1, disc space narrowing at multiple levels in conjunction with mild osteophytic spurring, disc space narrowing at L5-S1, and mild degenerative endplate changes.
This patient’s diagnosis of myofascial injury was made by careful and very specific physical examination of muscle and fascia. Treatment was directed toward helping her body recover from the injuries this examination detected, and also by reducing the fascial inflammation in her body resultant from food and perhaps environmental toxic exposures.
Patient XX was an ideal person for healing from this pain. She took all suggestions seriously, and followed all directions completely. Gluten and dairy free choices were absolute. Without inflammation from food and environmental toxicity, treatment acording to this paradigm of discovering and helping to heal the fascia injuries of a life time, pain can be relieved as quickly as the body can heal.
Hal S. Blatman, MD, is the founder and medical director of the Blatman Health and Wellness Center in Cincinnati, Ohio, a nationally recognized specialist in myofascial pain, and co-author of The Art of Body Maintenance: Winners’ Guide to Pain Relief, a reference for treating myofascial pain, from migraine headaches to plantar fascitis. He is credentialed in pain management, occupational and environmental medicine, and integrative holistic medicine, and also trained in craniosacral therapy and Healing Touch. After receiving his medical degree from the Medical College of Pennsylvania in 1980, Dr. Blatman completed two years of training in orthopedic surgery. He later studied ergonomics and toxicology during his residency in occupational and environmental medicine at the University of Cincinnati Hospital. In the early 1990’s, he studied with the late Dr. Janet Travell, a pain physician to President Kennedy. Dr. Blatman currently leads a team that specializes in the holistic and comprehensive rehabilitation and treatment of pain, ligament and tendon injury, fibromyalgia, and chronic fatigue syndrome. He is a past president of the American Holistic Medical Association, with offices also in Manhattan and Seattle.
.

References
1. Simons D, Travell J. Myofascial Pain and Dysfunction: The Trigger Point Manual, vol 1. 2nd ed, Lippincott Williams & Wilkins, 1999.
2. van der Wal J. The architecture of the connective tissue in the musculoskeletal system – an often overlooked functional parameter as to proprioception in the locomotor apparatus. Int J Ther Massage Bodywork. Dec 2009; 2(4) -23.
3. Langevin et al. Fibroblasts form a body-wide cellular network. Histochem Cell Biol. July 2004; 122(1)7-15.
4. Schleip et al. Fascia is able to contact in a smooth muscle-like manner and thereby influence musculoskeletal mechanics. J Biomech. 2006;39 (Supplement 1):S488.
5. Mitchell & Schmitt. Cardiovascular reflex control by afferent fibers from skeletal muscle receptors, In: Shepherd JT et al. (eds), Handbook of Physiology,Sect. 2, Vol III, 1977.
6. Berlucci G, Aglioti S. The body in the brain revisited, Exp Brain Res. January 2010;200(1);25-25.
7. Standley, Meltzer, J Body Mov Ther.July 2008; 12(3):201-3.
8. Pillon N et al., Muscle cells challenged with saturated fatty acids out an autonomous inflammatory response that activates macrophages. Cell Communication and Signaling.2012;10:30.
9. Perlmutter D. Grain Brain. Little Brown and Company, 2013.




