By Scott Cuthbert, DC
Research shows that whiplash injuries are a remarkably complex condition, which may explain the modest effects of typical medical, physical therapy and chiropractic interventions investigated to date. Contemporary management options for both the acute and chronic stages of WAD are not straight forward and, while offering some improvements in pain and disability, are far from being a panacea. Trials of medical and physical therapy management of acute whiplash have not demonstrated efficacy in terms of decreasing the incidence for those who develop persistent symptoms.1-3
The existing evidence-base does, however, support a shift in care to de-medicalize these conditions,1-4 and de-emphasize pharmacological and surgical approaches that carry high-risk profiles with no commensurate improvement in outcomes.5
With up to 50% of those sustaining a whiplash injury reporting ongoing pain and disability worldwide, it is essential to identify both the reasons for those at risk of poor recovery and to better understand the reasons in those who recover well. 6-7
The following report describes the multi-modal management necessary (as well as the sequence of previous therapeutic attempts by numerous physicians from many disciplines) for the ultimate recovery of a patient who experienced WAD. This patient had been previously evaluated and treated by three chiropractors, one osteopath, and three traditional medical doctors who performed many evaluations and treatments as well as performing facet and trigger point injections, along with multiple medications. Despite this, the patient showed increased symptoms in the year following her motor vehicle accident (MVA) and failed to reach maximum medical improvement (MMI).
This paper and a recent textbook by its author detail the background of muscular dysfunction in WAD and explain why muscular inhibition is a primary feature of the structural, biochemical, and mental-emotional disturbances accompanying and often perpetuating the symptoms following whiplash injuries.1
Motor Vehicle Accident (MVA) History
On October 21, 2017, this patient was the restrained driver of a 2015 Audi four-door sedan. She was decelerating for a red light in Pueblo, Colorado. The car in front of her stopped very quickly, and she swerved to the left to avoid hitting that car. Her car was hit on the rear-end passenger side by a Jeep Cherokee. The road condition was dry.
She immediately felt pain in her lower back, neck, and upper thoracic spine and acquired an immediate headache. She was taken restrained to a hospital by ambulance. An examination was done, and x-rays taken as well as a CT scan of the brain. She was dismissed with a prescription for medication. Examination ruled out cerebral concussion.
Pictures of her vehicle supplied to me show damage to the right taillight, fender, and bumper. The estimate from a mechanic showed a gross total of $3,665.62 for repair.
In the next several days however, her headache became much more severe, and the low back pain also became more severe.
One week after the accident the patient was advised by a friend to see the first of four chiropractors. She began with three visits per week of chiropractic treatment.
After six months of treatment, one of her three chiropractors asked her to complete the Neck Disability Index Questionnaire, with 9 of the 10 sections completed. On section 7 an answer is not checked, but she notes, “I have to work to pay bills but it causes extra pain.” The raw score of the 9 completed sections was 33, which is a severe level of disability. At this time a Revised Oswestry Low Back Pain Disability Questionnaire was completed, with a raw score of 37. This is considered as complete low back disability.
At six-months post-MVA, the pain drawing now showed pain radiating into the right leg, which was not present on her initial visits, and there is indication of right leg pain with provocative tests. There is further complaint of poor sleeping, dizziness, occasional decreased coordination, and poor memory only during times of headaches. The patient describes feelings of depression and anxiety related with frustration over her persistent pain. Treatment plan continued to be 2x/week for four more weeks. It appears that there was a plan or consideration to make consultation or referral to another medical doctor in the city.
A medical examination after the initial examination in the emergency room was given by her insurance company’s PPO doctor at six months post-MVA. He prescribed anti-inflammatory, muscle relaxer, pain relievers, and physical therapy treatments. Additionally, positive Waddell signs were present that included hypersensitivity to even light skin touch, axial compression as noted above, diffuse and generalized pain complaints, significant over-reaction, multiple bizarre symptom reports with simulated movements that should not cause pain, and profound and diffuse breakaway weakness in the lower extremities. The doctor’s impression was that the patient did indeed have significant pain, but he noted that the Waddell signs were suggestive of symptom magnification versus exaggeration. Relpax® was given for abortive migraine treatment. Subsequent medical treatment involved injections of the bilateral L4-5, and L5-S1 facets with fluoroscopic guidance and trigger point injections. Ten trigger points in the neck and shoulders were injected and only slightly improved her neck and midscapular pain.
A subsequent MRI of the lumbar spine was performed six months after the initial MVA. Findings were (1) Mild degenerative changes of L5-S1 disc space noted with comparable posterior desiccated disc bulge/protrusion causing mild neural canal stenosis without evidence of cauda equina compression. Bilateral neural foramina are patent. There is no evidence of foraminal nerve root encroachment. No posterior disc bulge or herniation is seen. (2) The remainder of the examination was within normal limits.
Professional Applied Kinesiology (PAK) Examination
This long-suffering patient was referred to the author by her dentist, who had been treating her for TMJ imbalances that were thought to underlie her chronic headaches subsequent to the MVA. A thorough orthopedic assessment followed by a thorough manual muscle test (MMT) evaluation were employed in order to demonstrate the fundamental etiologies underlying the symptoms in this patient’s case.8
On my first examination (10 months after her MVA) she indicates that her headache has become much more severe, and the low back had also become more severe during the course of the past year. During my consultation she sat leaning to the right for relief. She stated that she has to sit that way most of the time to take strain off the lower back.
The severe headache is accompanied by visual problems and nausea. She takes medication prescribed by her medical doctor for the severe headache, which is ameliorative. She has difficulty sleeping because of pain. She states that her energy level has decreased since the accident.
In my systems review there are no contributing factors other than the MVA found. The patient remarked that she was in good health prior to the MVA. She had never had chiropractic care prior to the accident and was on no medication before the accident.
Upon measuring the cervical rotation, I mention that there is much better movement in rotation; and she states, “Yes, I can move my neck much better when lying down.” This is confirmed by me visually. Rotation cannot be measured weight-bearing with an inclinometer, and I did not have a goniometer available.
Sitting blood pressure was 103/72; standing b/p 99/73, pulse rate 86. Normally the blood pressure rises around 6 mm when standing to accommodate against gravity so adequate blood is supplied to the brain. She acknowledges that she gets lightheaded when she stands, and also bright lights bother her eyes. This was not present prior to the accident, and are physical signs of adrenal gland stress and dysfunction, called Ragland’s sign.9
Orthopedic tests persisting despite 10 months of therapy for a MVA. Romberg, finger-to-finger, and finger-to-nose tests are passed. Right heel-to-shin test is done easily; the left is done with difficulty. Trendelenburg test is positive on the left. As she moves into Adam’s position there is pain in the low back area, and she stops at about only 20 degrees. Lumbar lateral bending is limited by pain in the left sacroiliac area. Extension is not as painful as forward flexion. Kemp test bilaterally causes discomfort in the left sacroiliac. She states that when she goes into the Kemp position to the left it feels like her back is going to pop. Left Bechterew test causes discomfort in the left sacroiliac; right Bechterew test is negative. Lindner’s seated test causes pain down the entire length of the spine, and she feels it in the back of her left leg. FABERE Patrick test on the left has very limited range of motion and discomfort in the left sacroiliac. There is also very limited range of motion in the right FABERE Patrick test, but it does not cause pain. Left straight leg raise is positive at 45 degrees for pain in the left sacroiliac area. Right straight leg raise is limited at 80 degrees by tight hamstrings. Left Bragard test is positive. Quadriceps and Achilles reflexes are 2+ bilaterally.
Mennell’s sacroiliac test is positive bilaterally. Hip extension is positive for pain bilaterally in the sacroiliac area, worse on the left. Ely’s heel-to-buttocks is negative. Left Leguerre test is positive for pain in the sacroiliac and no pain in the hip; right is negative. Hibb’s test is positive for sacroiliac pain on the left and negative on the right.
Shoulder depression and Jackson foramina compression tests cause discomfort in the cervical spine but there’s no radiation to the arms. Right JayMar dynamometer test is 45/40/40 lbs; left is 20/24/20 lbs.
AK manual muscle test findings. The purpose of specific manual muscle tests in the examination is to determine if there is objective evidence to substantiate the continuing subjective complaints. If so, then the examination design continued to determine the cause of the dysfunction and whether it can be improved. To accomplish this, various sensory receptor stimuli were applied to determine if the muscle dysfunction was improved, indicating the weakness was functional in nature and had potential for improvement. If there was improved muscle function the type of sensory stimulus that causes the improvement separates the problem from a peripheral neuropathy, receptor, spinal cord, brainstem, cerebellum, thalamus, or cortical lesion. Unless otherwise noted the muscle tests listed in this examination as strong are equivalent to 5 and weak as 4 as graded in the Guides to the Evaluation of Permanent Impairment, 5th edition, by the American Medical Association.10
The psoas and tensor fascia lata muscles test weak bilaterally and do not strengthen to suboccipital stimulation. The left psoas strength is grade 3/5. Extensor hallucis muscles are weak bilaterally. Piriformis muscles are weak bilaterally. Tibialis posterior and tibialis anterior muscles are weak bilaterally. Peroneus longus and brevis muscles are weak bilaterally. Hamstring muscles tested as a group are weak bilaterally. Support (“therapy localization”) to the bilateral sacroiliac articulations strengthens the hamstring muscles. Gluteus maximus testing position cannot be maintained (2/5). Bilateral lower trapezius muscles are weak.

McMurray’s test is negative. There is no pain in the knee external ligaments, Patella gliding is smooth. Sartorius and gracilis muscles, however, test weak bilaterally. Passive knee movement is smooth; active knee movement of the right knee produces crepitation.
Pectoralis muscles (clavicular and sternal divisions) test weak bilaterally. Deep neck flexor, anterior scalene, and sternocleidomastoid muscles are weak to the point she cannot hold the testing position (2/5). Abdominal muscles test weak. Deltoid, serratus anterior, infraspinatus, supraspinatus, subscapularis, teres minor, rhomboid, levator scapula, opponens pollicis and flexor digiti minimi brevis muscles are weak bilaterally. Biceps, triceps, and brachioradialis reflexes are 1+ bilaterally.
Impression. All muscle tests done in this examination were graded at 4/5 with the exception of the left psoas, gluteus maximus, and neck flexors which are 2/5 (full movement only when gravity is eliminated).
When there is 4/5 diffuse weakness as in this patient’s case there is often one central cause. If a central cause can be located and corrected, there will be an immediate and dramatically improved 5/5 function of many of the dysfunctioning muscles.
A common cause of diffuse 4/5 weakness is dural tension as described by the neurosurgeon Alf Brieg. Brieg stated that the primary source of adverse mechanical spinal cord tension is “set up directly by virtue of its anchorage at its two extremities, namely the brain and cauda equina.”11 A clue in this patient’s case was the increased pain down her entire spine when Lindner’s seated orthopedic test was done. The dura mater has a firm attachment at the foramen magnum and upper cervical vertebrae, and then does not have a firm attachment again until the sacrum. Lindner’s seated test stretches the spinal cord around the forwardly flexed spinal column, placing tension on the dura and increasing her pain.
Applied Kinesiology Chiropractic Treatment
The first step in this patient’s recovery was being able to observe immediate improvements in objective tests as a result of treatment, i.e., changing muscle function to 5/5 following the manipulative effort. This was accomplished within the first two weeks (6 sessions) of examination and treatment during each and every treatment session.
The next step was to determine if the improved function was still present on the next office visit. Any of the corrections that were not stable were recorrected, or further causes of the positive MMT finding were discovered and treated. The AK examination looks for the reason for recidivism and appropriate corrections are made. This was a two-week-long continuing investigation as levels of injury from the MVA were found and corrected. It must be understood that the body is a self-correcting and self-maintaining mechanism. When the body cannot correct dysfunction, it will often make adaptation to return function to as close to normal as possible. Often when there has been a long period of dysfunction, one may find on examination many adaptations that the body has made attempting to manage the condition.
In this patient’s case, there were several layers of dysfunction that were worked through involving the TMJ, the cranium, the lumbar spine and pelvis, and even the feet, and their associated muscle attachments. Besides the feet, these areas are where the dura mater attaches to the rest of the body, and correction of dural tensions led to improvements in her symptom and functional patterns since the onset of her MVA symptoms one year before.
To test whether spinal dysfunction might be a cause of her dural tension, I evaluated the upper cervical area and found that when static digital pressure was applied to the left side of the axis spinous process in a very specific vector the sternocleidomastoid and right pectoralis (sternal division) and right psoas muscles tested 5/5. As soon as the spinous process digital pressure was released the muscles returned to a 4/5 function. This indicated that a spinal adjustment applied to the axis vertebra in the same vector that produced muscle strength would release tension on the dura and improve function in the motor neurons.
There was poor function and organization of the cervical flexors and extensors that I diagnosed as secondary to subtle entrapment of cranial nerve XI supplying the sternocleidomastoid and upper trapezius muscles. This was supported by the improved muscle function after the AK cranial treatment. Although the deep neck flexors (scalene and others) are not supplied by cranial nerve XI, their function also improved after the cranial corrections. This probably occurred because of improved cervical function affecting the spinal nerves.
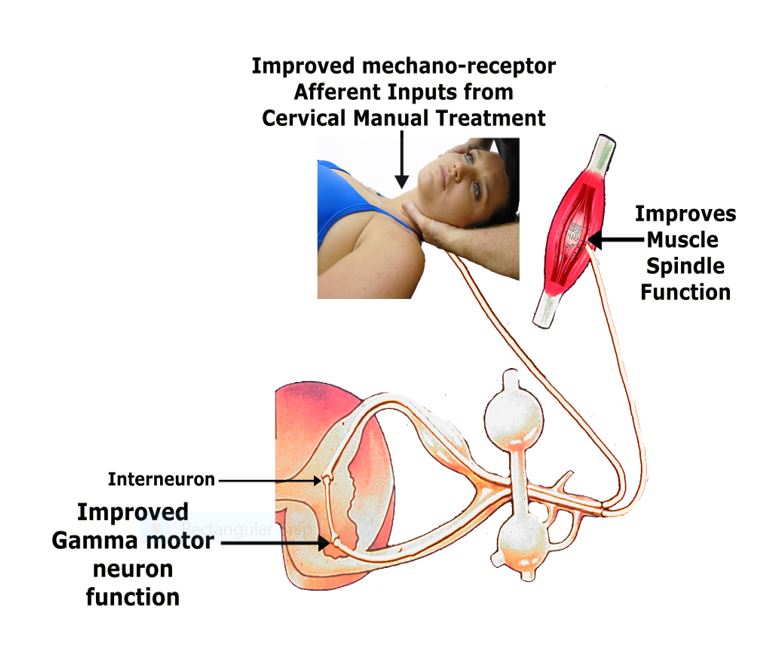
How Chiropractic Adjustments Improve Muscle Tone
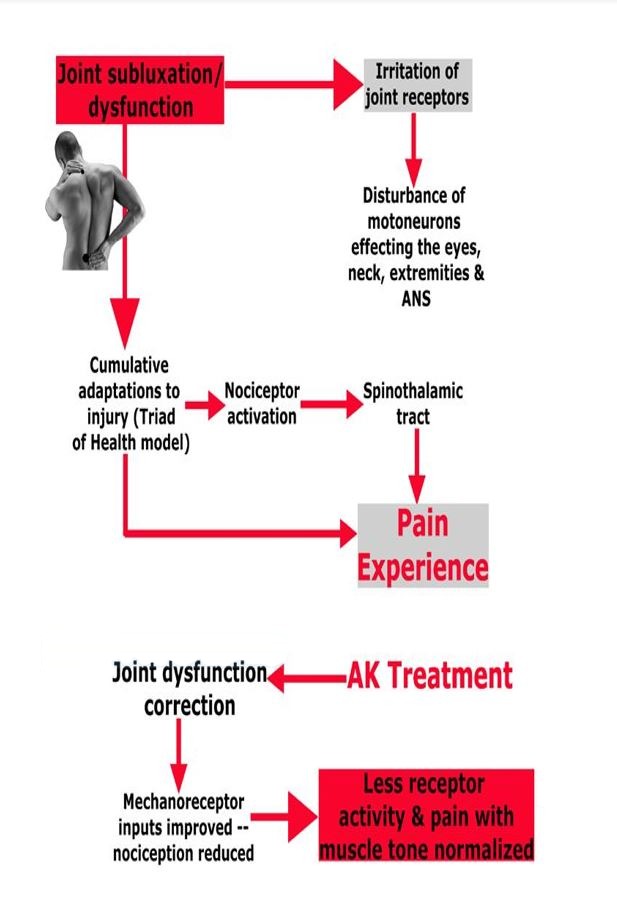
I believe that correction of the cranial-sacral primary respiratory system produced a wide range of objective improvement throughout her body. This correction addresses cranial nerve dysfunction and reduces dural tension, producing a positive effect on many aspects of her nervous system. Follow-up spinal examination found considerable improvement after the cranial-sacral function was improved.12
Treatment to the factors producing her dural tension was effective in relieving her headaches and cervical spine pain and limitations in range of motion over the course of two weeks (6 visits). After the first upper cervical correction, there was profound strengthening of the cervical flexor and sternocleidomastoid and scalene muscles. However, these immediately re-weakened upon opening and then clenching her mouth shut. Once AK TMJ treatment to the muscles of mastication and the temporal bone were given, this no longer occurred. After stabilization of these factors with two weeks of treatment, the improvement in her clinical picture and return to MMI pre-accident status has been maintained for nearly one year.
After two weeks on adrenal nutritional supports (Drenamin (SP) and Ashwagandha), her sleep and adrenal signs as well as her depression and anxiety were improved.13-14
No modalities such as electric muscle stimulation, trigger point injections, etc. were employed during this AK chiropractic treatment period so that the effects of the functional neurologic treatment could be observed. Subjective (symptomatic) improvement was recorded by the steady disappearance of the positive MMT and orthopedic tests noted above as well as by rating her symptoms using visual analog scales.
The impression given by her second medical doctor that multiple Waddell signs were suggestive of symptom magnification vs exaggeration was incorrect. Bizarre symptoms, hypersensitivity, and other unusual findings are compatible with the subtle functional impairments taking place in this patient’s condition. Correction of these physiological imbalances and dural tension post-MVA improved her Waddell signs significantly.
SIDEBAR
| Glossary of Applied Kinesiology’s Integrative and Revolutionary Diagnostic System |
| Manual muscle test |
| The actual testing of the muscle had been firmly established by Kendall and Kendall,15 who held that a muscle from a contracted position against increasing applied pressure could either maintain its position (rated as “facilitated” or “strong”) or break away and thus be rated as “inhibited” or “weak.” The testing of muscle strength itself has been widely practiced in manual medicine for decades and the use of the MMT for functional conditions continues today with the work of Goodheart (and nearly 1 million ‘kinesiologists’ around the world),16 and many others like Janda, Lewit, and Liebenson.17-25 The American Medical Association has accepted that the standard method of MMT used in AK is a reliable tool and advocates its use for the evaluation of disability impairments.10 |
| Challenge |
| Challenge is a diagnostic procedure unique to AK that is used to determine the body’s ability to cope with external stimuli, which can be physical, chemical, or mental-emotional. Cranial and vertebral challenge as used in this case report have been described in the literature previously.1 After an external stimulus is applied, muscle-testing procedures are done to determine a change in the muscle strength as a result of the stimulus. Through this approach, ineffective therapies that produced no improvements in muscle strength were rejected, and only those that elicited a positive muscle response were used. This guided the treatments given to the patient. |
| Therapy localization |
| Therapy localization is a diagnostic procedure unique to AK that consists of placing the patient’s hand over areas of suspected involvement and observing for a change in the MMT. This method assists the doctor in rapidly finding areas that are involved with the muscle dysfunction found on MMT and has been used around the world clinically for over 50 years.1 Rosner et al in two consecutive, blinded, controlled clinical trials and literature reviews clearly supports the AK concept of therapy localization.26-28 Collectively these data suggest that stimulating or stabilizing the muscles, joints, ligaments, and skin — and their associated cutaneomotor reflexes — can produce measurable changes in muscle function. |
| “Weak” muscle |
| A muscle that may or may not develop full power, but on MMT it does not neurologically function at its full capacity. Preferable terms for muscles that test weak or strong are termed conditionally inhibited and conditionally facilitated, respectively. According to the majority of leading researchers in the field of chiropractic and manual medicine today, the combination of muscular inhibition, joint dysfunction and trigger point activity are the key peripheral components leading to functional pathology of the motor system. In AK, the presence of each of these factors are differentially diagnosed using the ‘challenge’ procedure cited above. |
| Indicator muscle |
| A muscle tested to determine if there is a change in its strength as a result of some testing mechanism (challenge or therapy localization, for instance) applied to the body. Generally an indicator muscle is strong prior to the test and weakens as a result of the specific testing procedure. |
References
- Cuthbert SC, Walther DS. Whiplash Dynamics and Manual Muscle Testing. Amazon Kindle, 2018.
- McGee, S, et al. Systematic review of the measurement properties of performance-based functional tests in patients with neck disorders. BMJ Open. 2019 Nov 24;9(11):e031242.
- Rosenfeld M, et al. Early intervention in whiplash-associated disorders: a comparison of two treatment protocols. Spine (Phila Pa 1976). 2000 Jul 15;25(14):1782-7.).
- NE Foster, JR Anema, D Cherkin, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet (London, England), 391 (2018), pp. 2368-2383.
- Traeger AC, et al. Care for low back pain: can health systems deliver? Bull World Health Organ, 97 (2019), pp. 423-433.
- Sterling M. Physiotherapy management of whiplash-associated disorders (WAD). J Physiother. 2014 Mar;60(1):5-12.
- Jull et al. Chap. 4: Alterations in Cervical Muscle Function in Neck Pain. In: Whiplash, Headache and Neck Pain: Research-based directions for physical therapists. Elsevier: Edinburgh; 2008:41-58.
- Cuthbert S. Manual Muscle Testing for Tension-Type and Cervicogenic Headaches. Townsend Letter. June, 2018.
- Cuthbert S, et al. Correlation of Manual Muscle Tests and Salivary Hormone Tests in Adrenal Stress Disorder: a Retrospective Case Series Report. Townsend Letter. Jan. 2015.
- American Medical Association: Guides to the Evaluation of Permanent Impairment, 5th Edition, Chicago, IL, 2001:510.
- Brieg A. Adverse Mechanical Tension in the Central Nervous System. New York: John Wiley & Sons, 1978.
- Cuthbert S, et al. The Association of Manual Muscle Tests and Treatment Outcomes With Headache and Cranial Dysfunctions: A Retrospective Case Series Report. Altern Ther Health Med. 2018 Nov;24(6):8-21.
- Standard Process Labs, Drenamin. https://www.standardprocess.com/products/drenamin.
- Supreme Nutrition Products, Ashwagandha Supreme. https://shop.supremenutritionproducts.com/ashwagandha-supreme/.
- Kendall HO, Kendall FP, Boynton, DA. Posture and Pain. Baltimore, MD: Williams & Wilkins; 1952:77-94.
- Jensen AM. Estimating the prevalence of use of kinesiology-style manual muscle testing: A survey of educators. Adv Integr Med (2015).
- Cuthbert SC, Goodheart GJ Jr. On the reliability and validity of manual muscle testing: a literature review, Chiropr Osteopat. 2007; 15(1): 4
- Schmitt WH Jr, Cuthbert SC. Common errors and clinical guidelines for manual muscle testing: “the arm test” and other inaccurate procedures. Chiropr Osteopat. 2008 ;16(1): 16.
- Janda V. Muscle Function Testing. London, UK: Butterworths; 1983:150-222.
- Lewit K. Manipulative Therapy in Rehabilitation of the Locomotor System, 2nd edition. Oxford, UK: Butterworth-Heinemann; 1991:120-124.
- Liebenson C. Ed: Rehabilitation of the Spine: A Practitioner’s Manual, 2nd ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2007:203-225.
- Motyka TM, Yanuck SF. Expanding the Neurological Examination Using Functional Neurologic Assessment, Part 1: Methodological Considerations. Int J Neurosci 1999;97(1-2):61-76.
- Green GN, Gin RH. George Goodheart, Jr., D.C., and a history of applied kinesiology. J Manipulative Physiol Ther 1997: 20(5): 331-337.
- Schmitt WH, Yanuck SF. Expanding the neurological examination using functional neurological assessment part II: Neurologic basis of applied kinesiology. Int J Neuroscience 1999; 97: 77-108.
- Goodheart GJ: Applied Kinesiology Research Manuals. Detroit, MI: Privately published; 1964-1998.
- Rosner AL, Leisman G, et al. Reliability and validity of therapy localization as determined from multiple examiners and instrumentation. Funct Neurol Rehabil Ergon. 2015;5(3):365.
- Rosner AL, Charles E. Therapy Localization in Applied Kinesiology: Validation by Means of Blinding in a Cohort Study. Funct Neurol Rehabil Ergon 2016;6(2):85-96.
- Cuthbert S. Applied Kinesiology Essentials: The Missing Link in Health Care. Amazon: Kindle. Chapter 3: Applied Kinesiology’s Diagnostic Advantages: Challenge and Therapy Localization. 2014: 25-38.