By Betsy Redmond, PhD, MMSc, RD
Medical Education, Diagnostic Solutions Lab, LLC (DSL);
private practice, Nutrition Provisions, LLC, Atlanta, GA (USA).
and David M. Brady, ND, DC, CCN, DACBN, IFMCP, FACN
Associate professor, University of Bridgeport, College of Health Sciences, Bridgeport, CT, (USA); chief medical officer, Diagnostic Solutions Lab, LLC (DSL) and Designs for Health, Inc. (DFH); private practice, Whole Body Medicine, Fairfield, CT (USA).
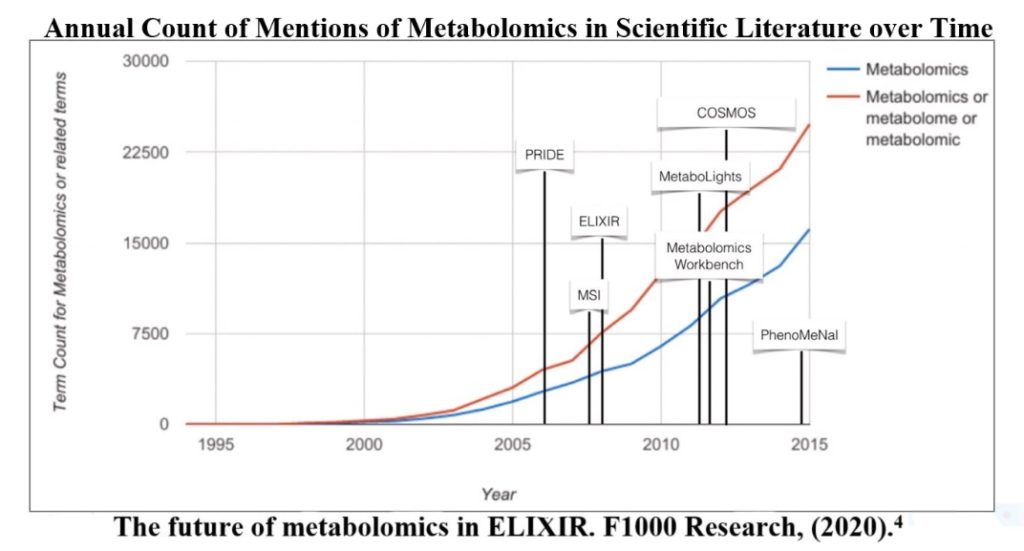
The term “metabolome” was first introduced in 1998. Metabolomics is the scientific study of chemical processes involving metabolites, and the metabolome represents the complete set of these metabolites.1 A metabolomic fingerprint is the measure of metabolites to describe an individual’s current metabolic status and has the ability to truly personalize healthcare. Metabolites can be impacted by past and current exposures, genetics, gut microbiome, diet, nutritional status, etc., and can aid in individualizing treatments and lifestyle recommendations. Functional medicine has long utilized urine organic acid testing to identify metabolites and impairments in key metabolic pathways. Conventional medicine clinicians are primarily familiar with organic acid testing for use in evaluating inborn errors of metabolism, such as maple syrup urine disease (MSUD) and phenylketonuria (PKU), or a few limited markers such as lactate, citrate, methylmalonic acid (MMA), and ketones. Though some claims made by functional medicine regarding organic acid testing have lacked support, metabolomics research is providing insight. Metabolomics allows the identification of key metabolites and pathways that can aid in discovery of associations with metabolic impairments or disease prediction, helping to refine functional medicine claims.2,3 Establishing better biomarkers is especially exciting when combined with wearables that can monitor activity and physiology, along with knowledge of gut bacteria, genetic status, and nutrient intake. Complete knowledge of applied metabolomics and all its synergistic effects may take decades, though individuals can still identify biomarkers that could shed light on their individual function.
Many functional laboratories that are currently operating developed their organic acid test reports prior to the development of modern metabolomics. The majority of these laboratories originated in the 1990s, some as early as the 1970s, and their educational materials were developed well before the introduction and coming of age of metabolomics.1
Initially, laboratories offering organic acid testing relied on educational material primarily based on biochemical pathways with limited literature, or even a single supporting study. When specific markers were elevated, it was generally identified as a lack of nutrient cofactors and nutrient need. Markers also identified other issues such as increases in detoxification pathways or microbial activity. Several laboratories established proprietary nutrient algorithms that reviewed all the markers they believed could be impacted by a lack of a specific nutrient. The full algorithms are not generally available for review, though many of the nutrient claims appear to have limited literature support; yet functional and integrative medicine clinicians, as well as some nutritionists and health coaches, routinely make nutritional intervention recommendations based solely on this data. If a pathway is blocked due to an impaired enzyme and specific metabolites are elevated, it is extrapolated that those markers would also be elevated in a nutrient deficiency that requires the same nutrient. Though an insufficiency of nutrient cofactors may certainly ‘clog’ pathways leading to elevated markers due to a decrease in enzyme function, it is often more complicated. A deficiency of a specific nutrient may not have the same metabolic impact as an impairment of a single enzyme. Research studies of metabolites from nutrient deficiencies are limited. Many laboratories have been slow to incorporate newer research and have shown reluctance to discontinue markers that have limited literature support.
An example is using elevated urine branch chain keto acids (BCKA) as a primary indicator for increased need of vitamins B1, B2, B3, B5, and lipoic acid. Biochemically it appears straightforward as each of the vitamins is needed for the BCKA enzyme function, though it has limited support in the literature, and there is only one human study that directly looks at B vitamin levels and intake in comparison to urine BCKA. The study found that supplementation of a B-complex (B1, B2, B3, B5, biotin, B12) supplement did lower urine BCKA levels, though it could not differentiate individual vitamins.5 The BCKA dehydrogenase enzyme is most sensitive to B1 levels, as noted in thiamin responsive MSUD.6 Additionally, the level of urine BCKA’s can also be impacted by other factors such as level of exercise, protein intake, fasting, inflammation, etc.7 Corporate algorithms may not consider these factors.
Henry Nix’s famous statement8: “Data does not equal information; information does not equal knowledge; and, most importantly of all, knowledge does not equal wisdom. We have oceans of data, rivers of information, small puddles of knowledge, and the odd drop of wisdom.”
Early metabolomics research conclusions often had limited explanations of why individual metabolites or associated pathways were impacted. Clinicians aware of functional assessments are likely more familiar with many of the metabolites and proposed explanations, though many have not been well researched in a clinical setting. Newer metabolomics research helps to bring clarity to evaluating metabolites, their associated pathways, how they respond in specific disease states or nutrient deficiencies, and proposed treatments. In order to have a broader acceptance, functionally focused laboratories will need to be more transparent in how conclusions were made, such as the literature support for each recommendation, the specimen type used, and populations targeted. Ideally laboratories would partner with research institutions to better refine and support current assumptions. Patients have partially been attracted to functional medicine because of dissatisfaction with conventional medicine, which many patients feel has been slower to incorporate newer research into practice. However, the flip side of this may be the danger in functional and integrative medicine models of practice in relying too heavily on some of this functional testing data in its current state, with its limited literature and evidence support, as a primary, or even sole determinant of interventional and therapeutic strategy. The old saying “Keep your minds open, but not so open as to allow your brains to fall out” should be aptly remembered as we engage in the practice of functional and integrative medicine.
Moving from Organic Acid Testing to Applied Metabolomics
Metabolomics research has primarily looked at the metabolites of disease by identifying which metabolites are more common in a specific disease compared to controls. Though much of the early research utilized plasma markers, urine metabolomics has gained ground in the last several years, as urine is easy to collect and as a waste product represents metabolic breakdown. The Urine Metabolome Database was developed to house a full list of urine metabolites and has been folded into the Human Metabolome Database (https://hmdb.ca/). Research has focused on identifying key urine metabolomic markers and pathways that are able to discriminate disease states from controls in a range of conditions, including autism spectrum disorders (ASD), kidney disease, glucose homeostasis, non-alcoholic steatohepatitis (NASH), cancer cachexia, and others.9-15 Newer research is starting to establish how these markers may identify an earlier stage of disease development and the associated pathways. For example, plasma alpha-hydroxybutyrate levels have been found elevated years prior to a diagnosis of diabetes and is known to be a key marker of glutathione status.16 Metabolomics may also support clinicians targeting treatments by discriminating responders from non-responders or assessing the impact of a particular recommendation like exercise or supplementation.17-20 Kim et al found urine glycine and phenylacetylglycine levels aided in discriminating responders from non-responders of antioxidant supplementation’s impact on erythrocyte GSH:GSSG ratio (reduced to oxidized glutathione).17 Research is starting to identify patterns of disease and connecting systems. An example of applied metabolomics in practice is utilizing data such as the Copenhagen Inter99 study. Subjects were drawn randomly from the Civil Registration System. Measurements were available for 4,117 subjects who participated in both baseline urine metabolomics assessment and a five-year follow-up examination.
Researchers found several higher baseline markers to be associated with a greater risk of elevated hemoglobin A1c (HbA1c) and insulin resistance (IR) five years later. These included 1-methylnicotinamide, alanine, creatinine, and lactic acid. Though not diagnostic, the markers may help to identify areas of concern long before an issue arises, allowing patients the opportunity to focus on lifestyle and dietary strategies that may provide some level of risk reduction.15 1-Methylnicotinamide has been associated with increased rates of diabetes, cirrhosis, and cancers, suggestive of increased nicotinamide N-methyltransferase (NNMT) activity.15 Perturbations in the glycolysis pathway have been reflected by increased lactate, pyruvate, and alanine.21
Targeted Metabolomics methods have already identified new molecular markers and metabolomic signatures of cardiovascular disease risk (including branched-chain amino acids, select unsaturated lipid species, and trimethylamine-N-oxide), thus in effect linking diverse exposures such as those from dietary intake and the microbiota with cardiometabolic traits.22
–Scientific State from the American Heart Association 2017