by Carolyn McMakin, MA, DC
The most important things to keep in mind when considering mental health, the brain and PTSD is that in the brain:
- Everything is connected to everything else;
- The system is designed to help you survive trauma and threat in a primitive world; and,
- Nothing in the brain reacts well to inflammation.1,2
First let’s look at the curious construct of mental health. What do we actually mean when we say “mental health?” According to the World Health Organization (WHO), mental health is “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community.”3
But subsequent commissions wrote numerous articles to expand this definition, such as:
Mental health is a dynamic state of internal equilibrium which enables individuals to use their abilities in harmony with universal values of society. Basic cognitive and social skills; ability to recognize, express and modulate one’s own emotions, as well as empathize with others; flexibility and ability to cope with adverse life events and function in social roles; and harmonious relationship between body and mind represent important components of mental health which contribute, to varying degrees, to the state of internal equilibrium.4
It becomes obvious that anything requiring so many words and which has so many different definitions, must be both complex and elusive. For the purposes of this article, we will have to admit that no one appears to have a clear concise definition of “mental health,” but we think we know it when we see it.
In oversimplified words, every mental health definition includes some reference to cognitive ability, social integration, emotional balance, stress coping skills, and work productivity. Once you begin to study psychology and neurology, it becomes clear that each component of mental health depends on a properly functioning brain. It is less obvious that a properly functioning brain is entirely dependent on balanced and healthy function of the immune, digestive, and endocrine systems. Let’s look at this one function at a time and then look at what happens in PTSD when it all goes wrong.
Cognitive ability describes the process by which we acquire and manipulate information and use that information to learn, remember, organize, problem-solve, pay attention, make decisions, and communicate. Cognitive functions are the domain of the brain’s frontal lobe. But in the brain, everything is connected to everything else. The information acquired by the senses and sent to the cortex is sent instantaneously to every other part of the brain and modified and responded to by the healthy appropriate function of all of those brain structures.
An oversimplified example follows: the eyes send the visual image of a four-legged animal with orange colored short fur decorated with the asymmetric dark linear markings we call stripes to the visual cortex in the occipital lobe for perception. The perceived image is instantly sent to the frontal lobe and the prefrontal cortex (PFC) for interpretation and assessment. That image is interpreted as “cat” or “orange-striped-house-cat known as Tabby.” The prefrontal cortex performs the executive function of identification, interpretation, and threat assessment. Threat assessment for “cat” under normal circumstances is minor. The amygdala stress response centers remain quiet, stress hormones remain low, and the PFC determines the appropriate action is to move the arm and hand to gently stroke the cat. Impulses sent to the cerebellum and spinal cord motor centers create this gentle slow motion, and the interaction usually ends with a mild pleasant increase in serotonin and oxytocin. All of this activity occurs in less than five seconds.
Under some circumstances of education and experience, the visual image may be interpreted as “tiger.” The various portions of the prefrontal cortex in a person raised in India where orange striped cats may be large and dangerous, determine that this particular orange cat is shaped differently from a house cat and identifies it as “tiger.” Executive function in the prefrontal cortex determines that “tigers” are “bad and dangerous.” The prefrontal cortex signals the amygdala that “bad dangerous tiger” is present, threat assessment is high with lethal potential, catecholamines go up in the PFC and limbic system, the amygdala registers fear and communicates with the hippocampus regarding memories of previous trauma and tigers, then instantaneous communication coordinates cerebellum and spinal cord signaling to improve motor function for swift response. Signaling from the PFC, amygdala, and hippocampus feed into the anterior pituitary to increase adrenocorticotropic hormone (ACTH) and stimulate the adrenals to secrete cortisol to suppress inflammation and improve reaction time.
All of these impulses feed back to the prefrontal cortex which instantly decides the fastest, most certain escape route and how best to survive. The PFC determines: Whether and where to run? Where to hide and how best to get there? Is there anyone else at risk who should be helped? Will the time involved in helping someone else put the self at lethal risk and how is this to be decided? And all of these responses are only appropriate when the perceived image is indeed a tiger not a house cat.
During this threat and stress event, neurochemical feedback from the amygdala, hippocampus, and PFC directly inhibit higher cortical processing and short-term memory. Higher cortical processing and short-term memory are not essential; the only essential memory function is how the tiger was eluded the last time. When the threat is survived, everything should return to baseline equilibrium and comfortable function. This primordial system is in place specifically to help you survive threat in a primitive world.
In the modern world, the threat response can compromise the mental health function of “productive and fruitful work” since there are so many possible real and perceived threats, not just tigers. Productive and fruitful work requires higher cortical processing and both long- and short-term memory. If the brain is busy responding to threats like poverty, food shortage, housing or employment insecurity, domestic violence, and internalized world conflict, the same neurological survival strategies operate; and mental health suffers whether the threat is real or perceived.
That’s how the brain helps us survive threat. But surviving trauma in a primitive world is a little more complicated. When threat is identified and stress hormones rise rapidly in the PFC and limbic system, the connections between the amygdala, hippocampus, and medulla signal the vagus nerve that threat is imminent and turn down vagal tone. The vagal nerve nuclei reside in the medulla and give rise to the longest and, arguably, most crucial nerve in the body, the vagus.
The vagus mediates all basic bodily functions and 80-90% of its fibers are afferent. The vagus notifies the brain directly and immediately about infection and trauma in the periphery when it is stimulated by PAMPs (pathogen associated molecular patterns) and DAMPs (damage associated molecular patterns). Afferent vagal signaling goes to the vagal nuclei in the medulla and from there to the limbic system and the PFC to alert the brain to infection or injury. Efferent signaling from the limbic system to the medulla turn down vagal function to help survive the stress. It is a well-coordinated self-correcting circular feedback system.
The vagus controls digestion by increasing digestive secretions, maintaining pH and motility in the GI system. It slows the heart rate by connections to the atria and the ventricles. The vagus controls all but one muscle involved in speech and swallowing. The vagus has a primary role in suppressing the immune system when there is injury, infection, or threat. If you are repairing a laceration, fracture, or infection you want the immune system active until repair is complete; and since the vagus suppresses the immune system, you want vagal stimulation reduced during this time.5 Direct connections from the limbic system to the vagal nuclei in the medulla ensure swift and reliable communication. The vagus suppresses glucose production by the liver. Since you need glucose to fuel the muscles that will help you run away from the tiger, the vagus needs to be suppressed so the liver can produce glucose so the muscles can run so you can get away from the tiger. If there is no need to run, but the vagus is suppressed due to misperception of threat, glucose may rise contributing to elevated blood sugar.
Once the threat is gone and the PFC, amygdala, and hippocampus return to normal, pituitary and endocrine function return to normal, the adrenals quiet, vagal suppression stops and visceral, endocrine and immune function return to normal.
This entire process is designed to have you live or die within minutes during threat and recover or not within six to eight weeks during trauma or infection.6 If the threat, infection or trauma continues for longer than eight weeks, the brain changes function and even structure to accommodate to the new dire situation.
When stress hormones, norepinephrine and cortisol are elevated for more than a few days, the brain “decides” that long-term stress has to be handled centrally and corticotropin releasing factor (CRF), also known as corticotropin releasing hormone (CRH), increases centrally. The central nervous system takes over the stress response.
The central neurochemistry and endocrine response are complicated but make sense from a survival standpoint. CRF decreases all non-essential hormone functions. Follicle stimulating hormone (FSH) and luteinizing hormone, which promote ovulation, sperm production and pregnancy are reduced centrally. Pregnancy in the face of long-term threat is not a good idea. CRF suppresses growth hormone releasing hormone (GHRH) centrally, which reduces release of growth hormone that enhances amino acid transport across cell walls in an adult to promote tissue repair. CRF reduces thyroid stimulating hormone (TSH) centrally, thyroid hormone being non-essential to short term survival. CRF stimulates cortisol release from the adrenals. Cortisol suppresses acute inflammation but also thins the gut wall and leads to leaky gut, which results in further immune system activation, IgG and IgE antibodies, allergies and chronic inflammation. When the gut wall gets thin enough it has trouble transporting the bulky branched chain amino acids that make neurotransmitters like dopamine, serotonin, epinephrine, and the thyroid hormone receptor. CRF in the cortex acts specifically as a neurotransmitter itself that impairs complex cognitive processing and short-term memory and promotes selective long-term memory for traumatic events previously survived.7-12
Remember that the entire neuro-endocrine-immune system is designed to keep you alive in conditions of threat, stress, and trauma. Survival is the prime directive.
All neurochemical signaling happens in microseconds and requires electrical impulses to release specific neurotransmitters at specific synapses in specific parts of the brain, spinal cord, and nerves in delicate instantaneous coordination. And that is where inflammation becomes a problem.
Remember item 3. Nothing in the brain reacts well to inflammation. In general, inflammation slows conduction and interferes with neurotransmission. If the stress response and vagal function are not back to baseline in minutes, if the injury and infection are not repaired in eight weeks and the vagus remains suppressed, then the vagus is not suppressing the immune system or controlling the motility, the pH and the microbiome in the gut; the gut leaks small peptides from ingested food, further activates the immune system, and inflammation increases. When inflammation increases, the nervous system becomes more dysregulated and slower. Corticotropin releasing factor (CRF) causes the cortex to focus on previous traumatic events to the exclusion of recent events that may be neutral or positive. If this goes on long enough, the amygdala, hippocampus, and prefrontal cortex eventually change in activity and even in size.
What does that mean for mental health? Remember that every mental health definition includes some reference to cognitive ability, social integration, emotional balance, stress coping skills and work productivity. Inflammation, CRF and alterations in the PFC impair cognitive function,1 executive function and decision making.2 Social integration and emotional balance depend on the specific neurotransmitters serotonin, dopamine, and oxytocin all of which depend on branch chain amino acids for their structure.13 When the gut wall thins and branch chain amino acid transport is inhibited,14 synthesis of neurotransmitters that depend on branch chain amino acids is delayed or reduced. Without serotonin, dopamine, and oxytocin mental health is elusive or impossible.
Stress coping skills depend on normal levels of stress hormones and the proper function of the prefrontal cortex and the limbic system (the amygdala and the hippocampus). In long-term stress, all of this delicate balance is disrupted. And the ability to do productive work will depend on the type of work that is considered productive for any specific individual. A concert pianist, an astrophysicist and a carpenter all have different demands on PFC, cortical function, and long- and short-term memory. The inevitable conclusion is that severe chronic stress is incompatible with mental health.
How does this lead to PTSD? A complete detailed description is beyond the scope of this article, and includes genetics, perinatal influences and nutrition as well as neurology and endocrinology. A broad-brush and incomplete answer takes us to the prefrontal cortex, the relationship between the cortex, the limbic system and the vagus, and inflammation. There are so many portions of the stress response that increase inflammation. Inflammation slows conductivity in neurons and impaired conductivity interferes with the delicate feedback system that keeps the brain, limbic system, vagus, and immune system balanced and supportive of mental health.
When your prefrontal cortex has to make the instantaneous discrimination between threat and not threat, cat and tiger, norepinephrine or serotonin, run or cuddle and communicates that to the limbic system on a moment to moment basis and inflammation slows the feedback, what can happen? Survival is the prime directive.
In chronic stress, limbic input to the cortex and PFC increases and biases the prefrontal cortex towards perceiving threat. The PFC in PTSD patients fails to extinguish conditioned fear, fails to inhibit neuroendocrine response to threat-related stimuli, fails to re-assess emotional responses and sees all stimuli as threats to the self.2 The amygdala in PTSD is more likely to perceive the environment and any stimuli as threatening. The hippocampus is more likely to remember only traumatic events and disregard context. The limbic memories are so strong that they spill over into the visual cortex and cause flashbacks and nightmares. The limbic system becomes sensitized to perceive any stimuli as threatening and turns down the vagus through its connections to the vagal nuclei in the medulla. The vagus stops suppressing the immune system, inflammation increases and the split-second communication that would give the PFC time to discriminate cat from tiger is disrupted. Stress hormones go up and the brain becomes more sensitive to them.
Mental health as demonstrated by cognitive ability, social integration, emotional balance, and work productivity becomes secondary. Stress coping skills are overwhelmed. Survival is the prime directive.
PTSD is being treated as a mental health disorder instead of a neuro-endocrine-immune problem. It is a huge problem worldwide and affects 8% of the general population, worse in war zones and much worse for women than for men. It is more prevalent than cancer or schizophrenia. The statistic is staggering. There are pharmaceutical therapies aimed at raising serotonin by slowing the degradation of serotonin at the synapse and medications for anxiety. Cognitive behavioral therapy is a type of talk therapy aimed at teaching the cortex that it’s really a cat not a tiger and trusting the cortex to prevail in communicating this to the PFC and limbic system. Eye movement and head tapping therapies attempt to recruit more primitive parts of the brain and distract them to reprogram the stress loop. These therapies seem to be able to interrupt the neuro-endocrine-immune cycle in enough parts of the loop to produce limited success. But the prime directive fights change, and PTSD that is two-years chronic is considered permanent.
But what if there was a single therapy that could reduce inflammation and quiet overactivity in specific parts of the brain, quiet inflammation in general, repair the intestinal wall to stop thinning and leaking and allow proper absorption of bulky branch chain amino acids to restore healthy neurotransmitter levels. If this therapy could also directly quiet the limbic system and increase secretions and function of the vagus, it would be ideal to restore mental health and repair PTSD. It appears as if frequency specific microcurrent (FSM) might have been doing exactly that since 2005.
FSM uses frequencies from a list found in an osteopathic office in 1946 that came with a machine manufactured in 1922. There is no evidence about how the frequencies were developed or verified that survived the medical purges of the 1930s.
In 1995, the list was discovered, and the frequencies were first applied with a two-channel microcurrent device approved for regulatory convenience by the FDA as a TENS device even though it delivers 1000 times less current than a TENS unit. The list has frequencies for tissues and for the conditions or pathologies that make those tissues dysfunctional. At first the frequencies were used only to treat muscle and nerve pain,15-17 but the list included frequencies for the immune system, the spinal cord, and specific parts of the brain. Clinical success was followed by limited neurochemical research.
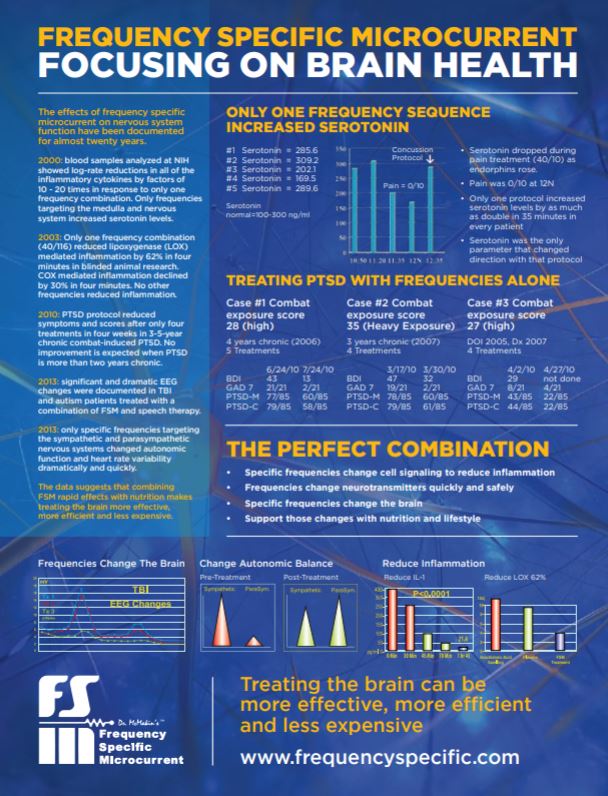
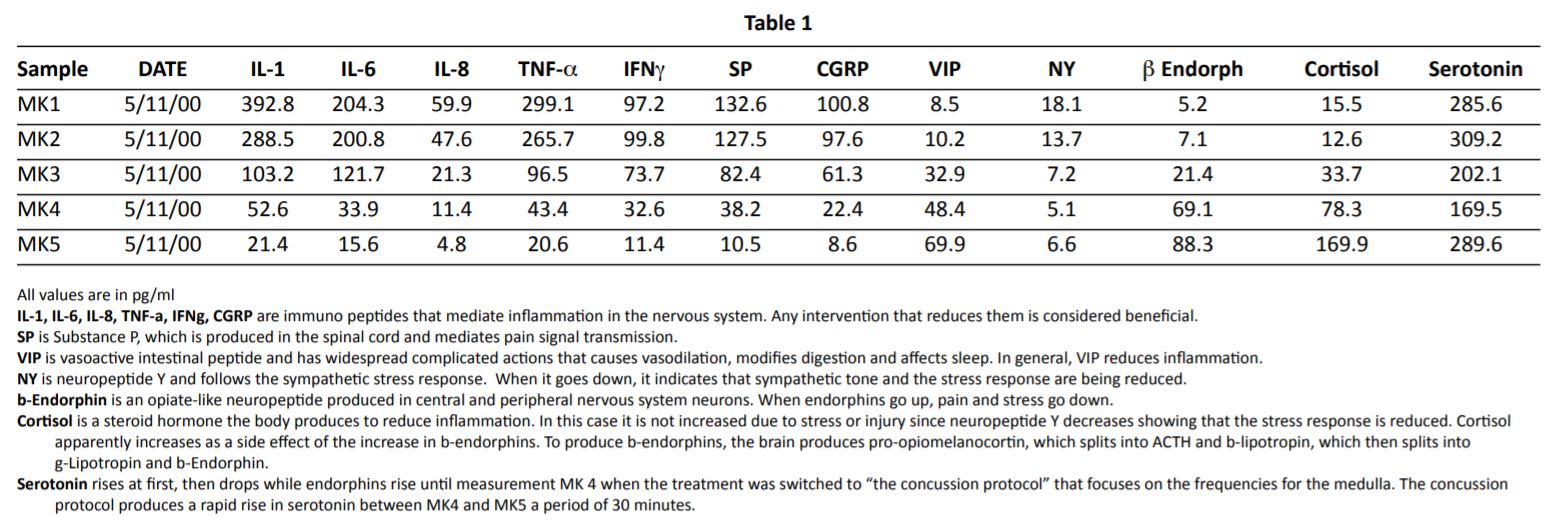
In 2000, it was discovered that the frequencies from the list “to reduce inflammation” (40 hertz) in the “spinal cord” (10 hertz) could not only reduce pain in fibromyalgia associated with spine trauma but also reduce all of the inflammatory cytokines and substance P and increase endorphins (See Table 1). The neuroimmune data was produced by an NIH immunochemist and show rapid logarithmic changes in neuro-inflammation never seen with any medical therapy.18 The same data showed that serotonin decreased while endorphins skyrocketed but immediately reversed course and rapidly increased when a frequency protocol for the medulla, called “the concussion protocol” was applied. This finding suggests that microcurrent electrical signaling can rapidly change the electro-neurochemical functions of the brain to change neurotransmitter levels based on specific frequencies.
Blinded animal research followed in 2003 showing that the frequencies to “reduce inflammation in the immune system” reduced lipoxygenase (LOX) mediated inflammation by 62% in four minutes and cyclooxygenase (COX) mediated inflammation by 30% in four minutes which was equivalent to injectable Toradol when it was tested in the same animal model by the same researcher.19 Clinical research followed demonstrating effectiveness in thalamic pain syndrome and phantom limb pain, both of which involve the thalamus and central sensitization.
In 2005, Barbara Harris, MD, combined her post-doctoral education in neuropsychology and her knowledge of FSM and began treating PTSD with FSM. When there were consistent successes and no adverse reactions, her protocol was taught at FSM advanced courses; and positive case reports were followed for the next fifteen years. Starting in 2015, the frequencies for the vagus were applied in atrial fibrillation, gastroparesis, vocal cord dysfunction, and small intestine bacterial overgrowth (SIBO) and appeared successful at restoring normal vagal stimulation and function.

PTSD is as hard to document as mental health and so FSM clinicians have limited data and no published case reports. Funding for non-pharmacologic treatment is hard to acquire in general and virtually impossible for unaffiliated clinicians, but the case report data is worth considering.
FSM in separate studies and case reports appears to address over activity and inflammation in the specific parts of the brain, raise serotonin levels, quiet central sensitization, quiet inflammation generally and specifically increases vagal tone. Reducing inflammation specifically in the small bowel could reasonably help repair a thin leaky gut. All of these effects would explain the success of the FSM protocol for treating PTSD.
It may not be possible to change the stress and threat in the world, but it appears possible to improve neurotransmitter levels, reduce inflammation, and improve mental health by restoring the healthy connection of everything to everything else in the brain. It’s worth a try.
Case Report
This case report is a compilation of similar cases to preserve patient confidentiality.
She was a 43-year-old woman with a precarious professional career in real estate sales. She could have been very successful, she said, but her stress levels were so high that she had trouble focusing on work and finishing the calls and the projects she needed to finish in order to close more deals.
“I sell condos in the most desirable area of Portland. This should be easy! My digestion is so weird. I bloat up and my stomach hurts after eating certain foods and lately it seems as if there are more of them that I react to. I don’t sleep well. Maybe 4-5 hours a night I wake up more tired than when I went to bed. My body gets stiff and sore with any exercise and I used to love exercise. I’m achy most of the time – not pain exactly just achy. My boyfriend is helping to pay the bills, but he is so controlling and crabby, I find myself doing things, or not doing things, to keep from making him mad. He gets mad when I spend time doing work instead of sitting with him.”
A hint to start: The answer is always in the history. Start with what the patient complains about but remember that this is hardly ever the real problem or the only problem.
- How long have you been with him?
- Does he ever hit you?
“No, just yells all the time about the most random things. I never know what to expect.”
“We’ve been together for 9 years, about one year after my divorce. I was a successful real estate agent in my twenties. And then we moved in together into this condo and I started getting tired all the time, stopped sleeping well, and my income fell off; and he started getting more controlling and seemed to enjoy the fact that he now made more money than I did. And he just loves to start arguments. It makes me so jumpy but now I need him to help financially.”
- What attracted you in the beginning? Why do you stay with him?
“He was cute and funny; we laughed a lot. He made good money, dressed well and drove a nice car. We were in the same business. He does property management.
Once we moved in together things changed as soon as I started to get tired and stopped sleeping. He got more controlling, and we fought more often. It’s been really bad for the last three years. I can’t focus well enough to do the kinds of complex deals I used to do so easily.”
- Would you mind if I asked you what your childhood was like? Did your parents fight all the time?
“Yeah, towards the end when I was a teenager, they fought a lot.”
- Did he ever hit your mom or you?
“No, but once they got divorced when I was 10, her next boyfriend yelled a lot at both of us. He hit her once I think but mostly, we had to be careful around him.”
- Did you ever have any accidents, serious illnesses, or surgeries?
“When I was little, I had some problem with my intestines- maybe I had to have surgery when I was 4 or 5 – see I have this little scar on my abdomen. But I got better fast. I got rear ended when I was 25 and I rear-ended someone when I was 19. No serious injuries though just sore for a few days, I get headaches now and then, but I see a chiropractor and get a massage and they go away.”
- Have you ever been molested, assaulted, or raped?
She squirmed a little at this matter-of-fact question, but since it was just in the same line as the other trauma questions, she avoided eye contact and answered it matter-of-factly: “The boyfriend used to come in my room at night when I was 11 or 12 and sit on my bed and talk to me like he was just being friendly, but then there was touching and some other stuff that was not right. But when I told my mom she said he was just being nice and we couldn’t afford to live without the money he brought in and I should figure out how to deal with it. So, I did. I started pretending I was already asleep and then I got a lock on my door.”
The physical exam was pretty basic and close to normal. Sensation, reflexes are all normal (+2 and brisk bilaterally). Abdominal palpation showed no signs of acute abdomen, but her belly was tender over the small bowel and cecum.
The only test ordered was salivary hormone testing for estrogen, progesterone, and salivary cortisol levels at four times during the day.
I don’t do relationship counseling, but it was clear that she had wandered into a relationship with a borderline personality, but the stress that causes wasn’t the only problem. Many women would have had no trouble leaving him. Why did she stay? Why was she tired? Why didn’t she sleep?
The diagnosis and treatment were determined by the history. Keys:
- The vagus nerve is turned off by infection, stress and trauma.
- Perimenopause is characterized by reductions in progesterone first. Estrogen falls 5 to 10 years later with menopause. Estrogen dominance results in fatigue, depression, and anxiety.
- Diurnal adrenal secretion of cortisol keeps inflammation down, gets you up in the morning, and goes down at night so you can sleep
Treatment with frequency specific microcurrent (FSM) involved quieting the limbic system, increasing vagal tone by increasing secretions in the vagus. The frequency to reduce the activity of the thalamus reduced her pain better than anything else although the frequencies for allergy reaction (to reduce histamine) also helped. Histamine stimulates class C pain fibers, which are slow unmyelinated fibers that create diffuse aching. We used FSM to treat the small intestine to reduce IBS symptoms and quiet the macrophage mediated IgG reactions. Macrophages consume the IgG complexes and then basically explode releasing histamine. To stop the histamine, you have to heal the small intestine and repair the leaky gut that creates the IgG complexes.
The FSM protocol for “brain fog” seemed to help with concentration and mood. She purchased a FSM home unit so she could run the PTSD and sleep protocols at home.
Salivary hormone testing was done to determine whether she needed hormone replacement or adrenal quieting or adrenal support. Genetic testing was done to determine if she had a methylation problem for B-12 or folate and to determine if she could phosphorylate B6. She had problems with folate methylation and supplementation with 5 mg of methyl folate a day helped with that. I usually give patients 5-HTP and P-5-P and that seemed to help with her mood and digestion.
Urine mold testing was done to determine if she had a mold infection from mold exposure in the condo she moved into with her boyfriend. That test was negative, so we didn’t have to deal with mold recovery.
Her homework involved seeing her ND for stool testing and treatment for parasites if necessary. There were no parasites but there was a need for butyrate for a month and probiotics.
Our clinic appointments were twice a week for four weeks. FSM produces rapid noticeable results which gave her hope after so many years of illness and anxiety. The hope was in itself helpful. Her symptoms changed within two weeks. As she recovered energy and was able to work more effectively, her income increased, and she moved out of the condo and separated from the difficult boyfriend. She had one follow up appointment at eight weeks and considered herself fully recovered. I don’t have any experience with treating this kind of case without the use of FSM.
References
- Warren K. Elevated markers of inflammation are associated with longitudinal changes in brain function in older adults. Journals of Gerontology. 2018: Vol 73; 770-778
- Liberzon I. The functional neuroanatomy of PTSD: a critical review. Progress in Brain Research, 2008: Vol 167; 151-168
- World Health Organization. Promoting mental health: concepts, emerging evidence, practice. Summary Report Geneva; 2004: World Health Organization
- Galderisi S. Toward a new definition of mental health. World Psychiatry. 2015: 14; 231-233
- Tracey KJ. The inflammatory reflex. Nature, 2002: 240; 853-859
- Sapolsky R. Stress and cognitive function. Current opinion in neurobiology. 1995:5; 205-216
- Crawford LJ. Neuroendocrine abnormalities in fibromyalgia. American Journal of the Medical Sciences. 1998: 315(6); 359-366.
- Crawford LJ. Neurohormonal perturbations in fibromyalgia. Rheumatic Disease Clinics of North America. 1996: 22(2); 267-284.
- Crawford LJ. Hypothalamic-pituitary-adrenal axis perturbations in patients with fibromyalgia. Arthritis and Rheumatism. 1994: 37(11);1583-1592.
- Neeck G. Hormonal Perturbations in Fibromyalgia Syndrome. Annals of the New York Academy of Sciences. 1999: 876; 325-338.
- Dessein PH. Hyposecretion of adrenal androgens and the relation of serum adrenal steroids, serotonin. Pain. 1999; 83(2): 313-319.
- Dessein PH. Neuroendocrine deficiency-mediated development and persistence of pain in fibromyalgia. Pain. 2000; 86(3): 213-215.
- Maes M. Serotonergic markers and lowered plasma branched-chain-amino acid concentrations in fibromyalgia. Psychiatry Research, 2000:97(1); pp11-20.
- Guyton AC: Textbook of Medical Physiology, Seventh Edition, WB Saunders Co., 1986
- McMakin C. Microcurrent treatment of myofascial pain in the head, neck and face. Topics in Clinical Chiropractic. 1998: Vol 5 (1); 29-35
- McMakin C. Microcurrent Therapy: A novel treatment method for chronic low back myofascial pain.” Journal of Bodywork and Movement Therapies, 2004: 8; 143-153
- McMakin C. Non-pharmacologic treatment of neuropathic pain using Frequency Specific Microcurrent. The Pain Practitioner. 2010: Fall; pp 68-73
- McMakin C. Cytokine changes with microcurrent therapy of fibromyalgia associated with cervical trauma.” Journal of Bodywork and Movement Therapies, 2005: 9;169-176
- Reilly W. Anti-inflammatory effects of interferential frequency-specific applied microcurrent. Proceedings of the National Health and Medical Research Council, 2004