By Erik Peper, PhD, BCB; Lauren Mason;
Richard Harvey, PhD; Lisa Wolski; and Jasmine Torres
San Francisco State University
Abstract
Gastroesophageal reflux disease (GERD), more commonly known as acid reflux, is a common and chronic disorder that affects up to 20% of people in the US. GERD is defined by regurgitation, or retrograde movement of stomach acid and gastric fluids into the esophagus. The three treatment options are lifestyle changes, medication, and surgery. A fourth option proposed here includes improving breathing patterns along with loosening clothing to decrease the hydraulic pressure on the stomach. Because mechanical pressure on the stomach can occur during various kinds of breath holding, coughing or a provocative diagnostic test such as Valsalva pressure that push the stomach content upward into the esophagus, and because wearing tight clothing can restrict abdominal expansion and/or abdominal breathing, biofeedback training provides an opportunity to address GERD symptoms. Dysfunctional breathing patterns that are characterized by rapid, shallow, and thoracic breathing is often associated with or triggered by a defense reaction. When teaching participants to wear looser clothing as well as master slower diaphragmatic, abdominal breathing, they may reduce the hydraulic pressure on the stomach.
The process of training healthy breathing as a non-drug option for addressing GERD is illustrated by a case example in which a 21-year-old female student who has had acid reflux for more than six years. In particular, she reported an average discomfort rating of 4, as measured from 0 to 5, and learned to shift her chest breathing to abdominal breathing through biofeedback training. By wearing looser more comfortable clothing, she maintained her ‘anti-GERD’ breathing practice during the year. Dramatically, after the first three weeks of practice, her discomfort decreased to an average of 2, and after one year to 0. Her breathing pattern systematically shifted from predominantly thoracic breathing (19 breaths/min) to abdominal breathing (7 breaths/min).
Discussed are three points: 1) the importance of breathing training to address GERD, which includes enhancing venous and lymph circulation and changing inter-abdominal pressure in the abdomen; 2) abdominal breathing as an early intervention strategy and prevention of acid reflux; and, 3) the importance of transferring breathing/stress management skills into daily life.
“For as long as I remember, I had stomach problems and when I went to doctors, they said I had acid reflux. I was prescribed medication, and nothing worked. The problem of acid reflux got really bad when I went to college and often interfered with my social activities. After learning diaphragmatic breathing so that my stomach expanded instead of my chest, I am free of my symptoms and can even eat the foods that previously triggered the acid reflux.”
–21-year-old woman student who has had symptoms since age 6
Gastroesophageal reflux disease (GERD), more commonly known as acid reflux, is a common and chronic disorder that affects up to 20% of people living in the US. GERD is defined as the regurgitation or retrograde movement of stomach acid and gastric fluids into the esophagus (Antunes & Curtis, 2017). The symptoms of GERD often include severe chest pains, heartburns, and can later result in the development of mucosal damage. Mucosal damage and chronic reflux in the esophagus often is a precursor to esophageal cancer and can cause further complications (Kim, 2013). As the prevalence of GERD increases, so do the risks of damage due to chronic exposure to stomach acid (e.g. acid reflux).
Unsurprisingly, symptoms of acid reflux mostly occur if someone begins lying down shortly after a meal, when stomach acid may more easily move to the esophagus with gravity. In addition, sleeping on a slanted bed with the head higher than the feet, so that the stomach content flows downward, often reduces GERD symptoms at night. Predictably, some behavioral recommendations for patients with GERD are to avoid lying down shortly after meals as well as sleeping on a slanted bed.
Acid reflux most commonly affects people over the age of forty, and males tend to have higher rates of complications. Diet, obesity, tobacco, and alcohol, among other factors such as genetics, are higher risk factors to the development of chronic acid reflux (Nwokediuko, 2012). Recommended lifestyle changes include dietary modifications, weight loss, and body position (Oliveria et al., 1999); thus, health care providers often advise obese patients to lose weight since it can significantly reduce GERD (Singh et al, 2011). Because treatment options for GERD not only include medications and surgery, but also lifestyle changes, some treatment options will be discussed next.
Treatment Options for GERD
There are generally three categories of treatment options for GERD patients: lifestyle changes, medication, and surgery. Lifestyle changes are typically the first line of treatment. This includes eating small bites of food, avoiding fatty or acidic foods, or any foods that may irritate or worsen symptoms of GERD (Surdea-Blaga, Negrutiu, Palage, & Dumitrascu, 2019). Weight loss in patients who are overweight has been associated with symptom reduction (Park et al, 2017), as well as avoiding alcohol and tobacco use, especially around mealtimes (Ness-Jensen & Lagergren, 2017).
Acid-suppressive medication most often include antacids, histamine-receptor antagonists, and proton-pump inhibitors (Bor & Kalkan, 2017; Zhang et al, 2017). Both antacids and histamine-receptor antagonists work to neutralize stomach pH. Although both of these medication types are generally prescribed for GERD patients, tolerability varies as there are some adverse side effects such as nausea, vomiting, and other side effects that lead to exacerbated gastrointestinal issues (Mendelsohn, 2018). Aside from side effects, these medications also cause pH to deviate from normal stomach pH that can cause other digestive complications (Beasley, Koltz, Lambert, Fierer & Dunn, 2015). Rather than decreasing stomach pH, proton pump inhibitors work to decrease the production of stomach bile. This treatment responds more poorly than antacids or histamine-receptor antagonists, has many more complications, and has a rising safety concern for its use (Nwokediuko, 2012). Anti-reflux surgery is an effective treatment option for long-term therapy but is not without complications. Disadvantages of surgical interventions include long-term medical maintenance, alongside complications such as dysphagia, bloating, as well as the risk of recurrence (Badillo & Francis, 2014).
Systemic Stress-Reduction Interventions
Behavioral interventions aim to reduce stress that is associated with acid flow up into the esophagus. Stress reactions related to acid reflux may be reduced by enhancing vagal tone through training such as heart rate variability biofeedback (Sowder et al, 2010; Sun et al, 2016). For example, Sowder et al (2010) as well as Sun et al, (2016) demonstrated that functional abdominal pain can be reduced with heart rate variability feedback training. In most cases, the increased vagal tone was achieved by breathing at about six breaths per minute.
Although many factors contribute to acid reflux, one common theme associated with behavioral interventions is to reduce the compressive forces on the stomach that would push the stomach acid into the esophagus. Furthermore, decreasing activities such as coughing or increasing pressure gradient across the diaphragm can reduce triggering acid reflux (Barham et al., 1995). An under-recognized compressive factor not listed is the pattern of respiration that involves the pressure and muscles around the stomach and esophagus. For example, during inhalation, the diaphragm flattens and descends, thereby pushing down on the abdominal content downward. If the abdomen cannot expand or extend fully, then the stomach becomes squeezed, thus increasing the risk of acid reflux. The factors that tend to restrict abdominal expansion include restrictive clothing, abdominal wall tightening, and obesity, in addition to the stress-breathing patterns that could be triggered by fear—all which may contribute to somatic discomfort and adverse symptoms.
In the late 19th and earlier part of the 20th centuries, physicians used a clinical diagnosis of neurasthenia primarily in women (Angst et al, 2010; Roelcke, 1997). The symptoms included fatigue, anxiety, headache, fainting, light-headedness, heart palpitation, high blood pressure, neuralgia, and depression. Neurasthenia was thought to be caused by a ‘weakness of the nerves’ (nervous exhaustion). Even though the diagnosis is no longer used in the same way as a century ago, similar symptoms still occur and are aggravated when the abdomen is constricted with a corset, or by stylish clothing (see Figure 1, below).

squeezes the abdomen.
The constricted waist compromises the functions of both digestion and breathing. When the person inhales, the abdomen cannot expand as the diaphragm is flattening and pushing downward. Thus, the person is forced to breathe more shallowly by lifting their ribs; this increases neck and shoulder tension as well as the risk of anxiety, heart palpitation, and fatigue (Cohen & White, 1947; Courtney, 2009). It also can contribute to abdominal discomfort since the abdomen is being squeezed by the corset and forcing the abdominal organs upward. Architects of the Victorian era recognized a need for space for a chair or lounge at the top of some stairs because people wearing corsets could faint, pass out, or otherwise experience breathlessness through the effort of climbing the stairs with restrictive clothing around their abdomen (Melissa, 2015).
During inhalation, the diaphragm flattens and attempts to descend, which increases the pressure of the abdominal content. In some cases, this causes the stomach content to be pushed upward into the esophagus resulting in heartburn and acid reflux, as shown in Figure 2.
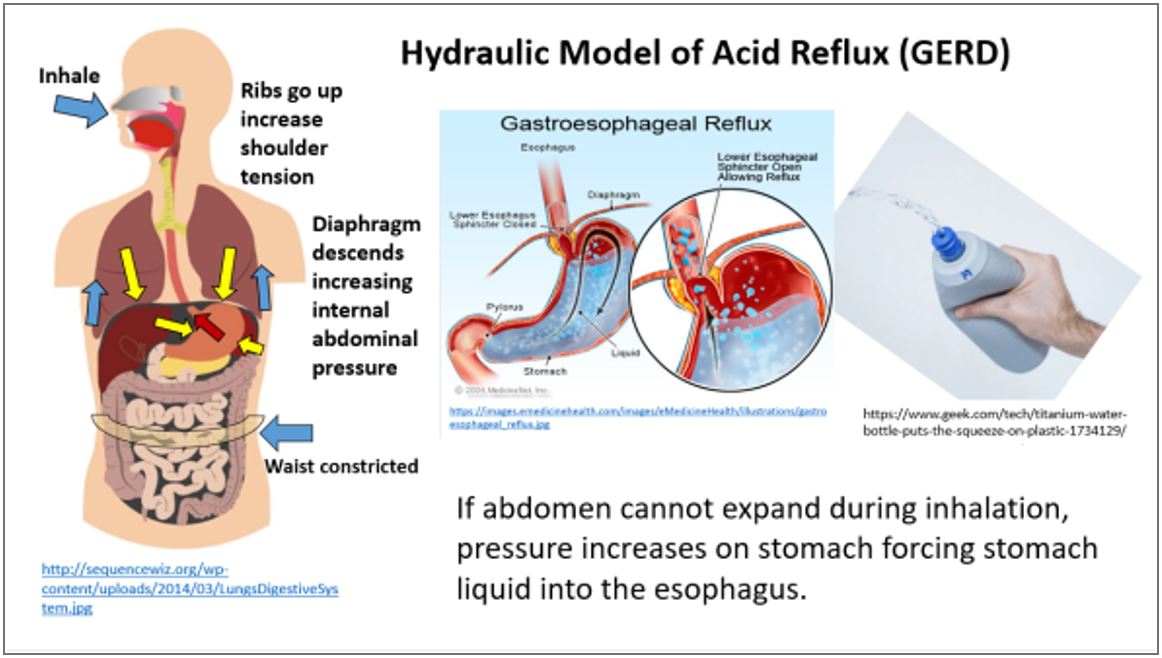
Educating Clients About the Hydraulic Model
Informing patients about the role of abdominal expansion during inhalation is seldom included in medical treatment approaches for two main reasons: most people think that breathing occurs in the chest, and training to breathe diaphragmatically takes time. It may be faster to treat a symptom of GERD with ‘acid-reducing’ medications compared to the training a client or patient to breathe correctly, which is a more curative albeit time-consuming path to patient health.
When educating clients about ‘full-body’ breathing that includes engaging both the chest and abdomen, it is useful to review some breathing patterns associated with acid-reflux symptoms. For example, when GERD patients breathe in their chest, they often pull in their abdomen –a pattern associated with fear. To reduce the inter-abdominal pressure on the stomach, the abdomen needs to expand during inhalation. Reducing inter-abdominal pressure includes wearing looser clothing that does not constrict the waist, a phenomenon referred to as designer jean syndrome (MacHose & Peper, 1991). When clothing around the waist is loosened, then the abdomen has the opportunity to expand in all directions in response to the downward movement of the diaphragm during inhalation.
Most people have experienced the benefits of loosening the waist when eating a large meal. The moment the stomach is allowed to expand, the person may begin to feel more comfortable. If you have experienced this benefit of unrestricted abdominal movement during breathing, ask yourself, “What could the long-term cost be of keeping the waist constricted?” A constricted waist such as from wearing tight clothing, from ‘designer jeans’ to a corset, may be as harmful to our health as having the emergency brake on while driving for a car. Furthermore, we are usually unaware that shallow, rapid breathing in our chest, especially with constrained abdominal movement, may contribute to symptoms such as anxiety, neck and shoulder tension, heart palpitations, headaches, abdominal discomfort such as heartburn, acid reflux, irritable bowel syndrome, dysmenorrhea and even reduced fertility (Cohen & White, 1947; Peper, Mason, & Huey, 2017; Domar, Seibel, & Benson, 1990).
Assessing Risk of Faulty Breathing
There are some simple behavioral steps for observing less healthy breathing patterns. For example, stand up and observe what happens when you take in what you feel is a ‘big’ breath and then exhale. Did you feel taller when you inhaled and shorter/smaller when you exhaled?
If the answer is YES, your breathing pattern may compromise your health. When you inhaled you most likely feel the muscles associated with lifting your chest, slightly arching your back, tightening and raising your shoulders, and lifting your head up while slightly pulling the stomach in. When you exhaled, you most likely feel muscles associated with the relaxing and collapsing the torso downward. Even the stomach muscles may have relaxed allowing the abdomen to expand. Unfortunately, expanding the chest while tightening the abdomen during inhalation is a dysfunctional breathing pattern, and the opposite of a breathing pattern that supports health and regeneration as shown in Figure 3.
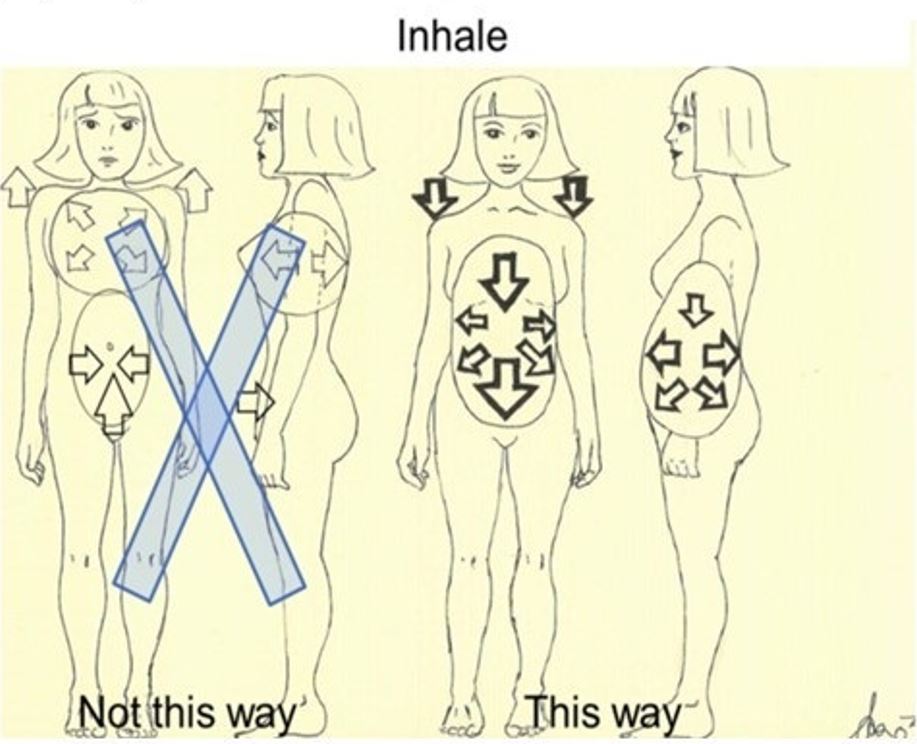
When you observe the breathing pattern of babies, young children, dogs, and cats, they are peaceful, breathing rhythmically into their belly. The abdomen is the main body area that appears to move during breathing. While breathing in, the abdomen expands in 360 degrees and when breathing out, the abdomen constricts and comes in. Similarly, when dogs or cats are lying on their sides, their stomach goes up during inhalation and goes down during exhalation.
Some people tend to breathe shallowly in their chest, as if they have forgotten to —or cannot– allow their abdomen and lower ribs to widen and extend during inhalation (Peper et al, 2016). Some factors contributing that restrict abdominal breathing include the following:
- Constriction by tight clothing such as “Spanx” (a modern form of corset?) to slim the figure, or by wearing tight fitting pants (‘designer jeans’) (MacHose & Peper, 1991). In either case, the abdominal content is pushed upward and interferes with unrestricted healthy breathing.
- Maintaining a slim figure by pulling the abdomen in (i.e. “I will look fat when my stomach expands; I will suck it in”).
- Avoiding post-surgical abdominal pain by inhibiting abdominal movement. Numerous patients have unknowingly shifted to shallow breathing in their chest to avoid pain at the site of the incision of the abdominal surgery such as for hernia repair or a Cesarean operation. A ‘guarded’ breathing pattern —guarding against the pain from abdominal surgery— trains a dysfunctional breathing pattern, which becomes the new ‘normal’ way of breathing unless they actively practiced diaphragmatic breathing to reverse the learned disuse of abdominal breathing muscles during recovery (Peper, Gilbert, Harvey, & Lin, 2015).
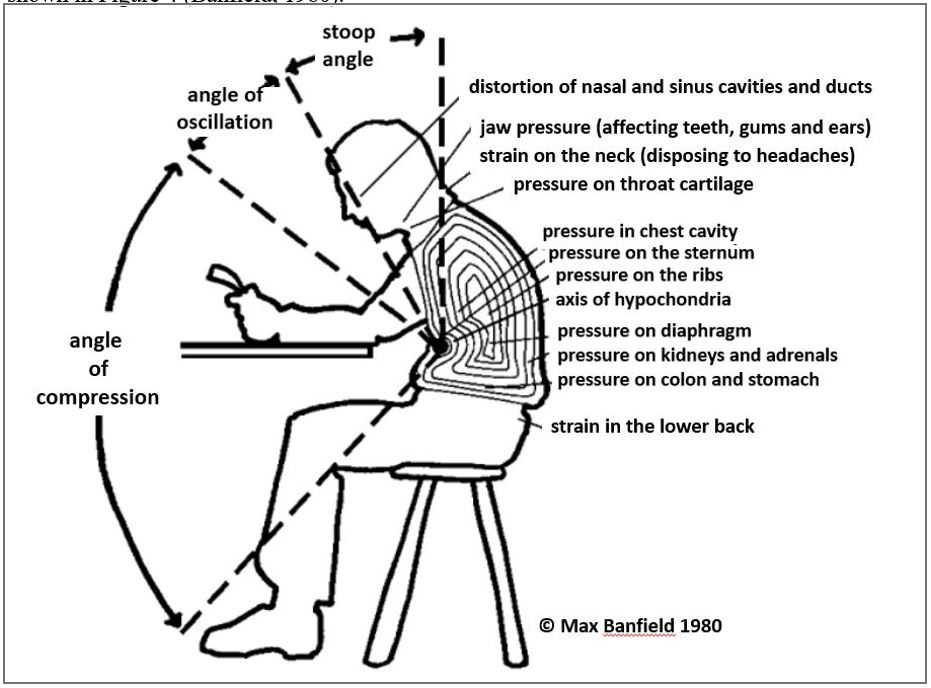
- Slouching as we sit to watch digital screens or, look down at our cell phone.
Observe how slouching affects the space in your abdomen. When you shift from an upright, erect position to a slouched or protective position, the distance between your pubic bone and the bottom of the sternum (xiphoid process) is significantly reduced. In the slouched/collapsed position, there is less space for the abdomen to expand in the protective collapsed position as shown in Figure 4 (Banfield, 1980).
Reproduced by permission from
http://users.chariot.net.au/~posture/
Regardless of why people breathe shallowly in their chest or avoid abdominal and lower rib movement during breathing, re-establishing healthy diaphragmatic breathing addresses a variety of symptoms such as hydraulic movement of acid from the stomach into the esophagus, anxiety, feeling faint, and complaints of various muscle aches associated with the chest and abdomen (Chen et al., 2017; Gilbert, 2003). Furthermore, students have reported that when they sit erect and shift to diaphragmatic breathing, which means the abdomen and lower ribs expand during inhalation and come in during exhalation, their symptoms such as acid reflux, irritable bowel disease and even menstrual cramping significantly decrease (Peper, Mason, Huey, 2017; Gibney, & Peper, 2003).
Case Example of Diaphragmatic Breathing to Reduce Acid Reflux
Participant: A 21-year-old female student who has suffered acid reflux (GERD-gastroesophageal reflux disease) frequently had to see doctors and has had a very long history of stomach problems since age 6. She was prescribed medications by all of her physicians, but none of them were very effective. Upon entering college, her acid reflux became especially severe. Her acid reflux started affecting her life in more ways than just stomach pain. She would avoid going out with friends with the worry of what they would eat and if it would cause her pain later. She started getting anxious and felt depressed because she felt that her acid reflux restricted her from living a normal life as a young adult. She had taken various over-the-counter antacid medications for a long time, as advised by her doctors, but these over-the-counter antacid treatments were not very effective. The more she took medications, the less effective it would become, and eventually, she completely stopped taking medications altogether.
The following is a typical procedure for assessing and training the participant.
Equipment and Pre-Baseline Stress Assessment: Breathing rate was recorded with respiratory strain gauges around the chest and abdomen (ProComp Infinity version 6.1, Thought Technology, Ltd). The participant sat comfortably for one minute. Respiration monitoring continued while she thought about a stressful memory for one minute, then let go of the stressor and sat comfortably for one minute.
Training: The learning of healthy breathing skills was part of a university class experience learning about biofeedback.
- She was coached in diaphragmatic breathing and instructed to wear looser clothing during the classroom training. During each session, she learned through biofeedback training to associate stressful thoughts with chest or abdominal breathing patterns.
- After several sessions over two weeks, a shift to predominantly diaphragmatic breathing occurred when she became more aware through breathing biofeedback of being stressed or breathing in her chest.
- Sessions also included training her to place her hands on her belly to generalize without the biofeedback devices what it felt like to breathe abdominally without instruments in a classroom.
- She also kept a weekly log during the semester to record severity of acid reflux on a relative scale of zero to ten, with zero being ‘not at all severe’ and 10 being the ‘most severe’.
- She also tallied up each time she was in a stressful event and whether she shifted her attention to her breathing during that time.
Post-Baseline Stress Assessment: Each post-session measurement included sitting comfortably for one minute. Respiration monitoring continued while she thought about a stressful memory for one minute, then let go of the stressor and sat comfortably for one minute.
Results: After training, her breathing pattern shifted from predominantly thoracic breathing (19 breaths/min) to abdominal breathing (7 breaths/min). She also had learned to maintain abdominal breathing during stress, as shown by comparing the pre- to post-stress assessments, shown by a representative graph in Figure 5.
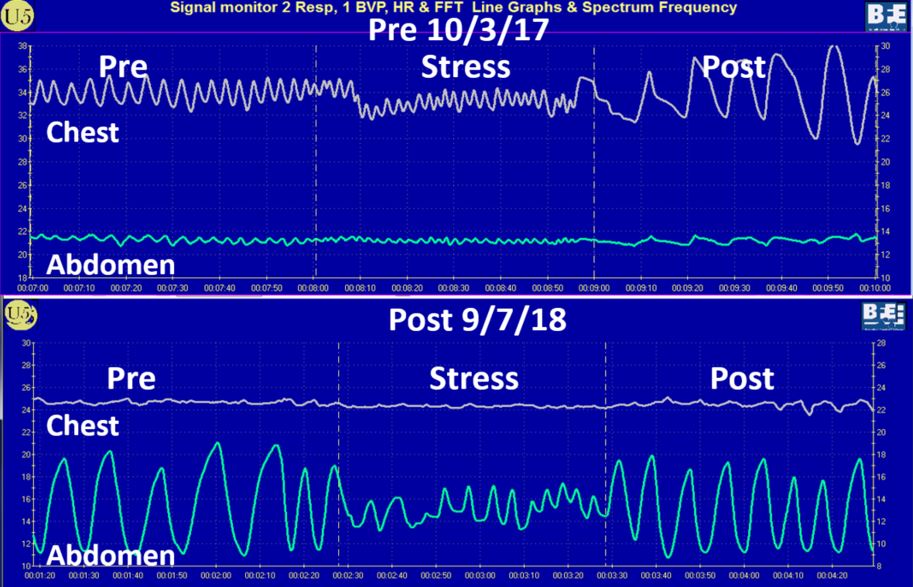
Her symptoms decreased within two weeks and she took no more medication.
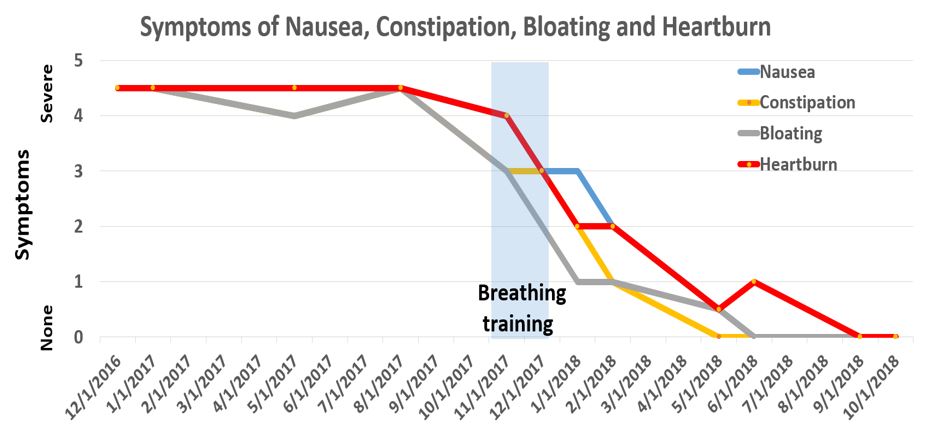
At the 11-month follow-up, she continued to be symptom free (see Figure 6).
Before Training
- She wore tight clothes that added pressure around her abdomen
- She restricted her diet to avoid foods that triggered symptoms.
After Training
- She wore looser fitting clothes that reduced the pressure on her stomach.
- She started eating foods that previously would have caused irritation, and was able to eat spicy or acidic foods and drink alcohol without evoking symptoms.
- Whenever she felt that she was about to have an episode of acid reflux, she calmed down and focused on her breathing while keeping her hands on her stomach, feeling it expand, and making sure she was not tightening her abdomen. Being more mindful of her breathing, she immediately noticed when she held her breath or started breathing thoracically, and she was able to remind herself to take deep breaths from the abdomen.
Discussion
After discovering biofeedback methods that allowed her to monitor her own breathing and learning diaphragmatic breathing techniques, she tried incorporating this knowledge in an effort to mitigate her symptoms of acid reflux. She soon observed that she breathed thoracically, through her chest, rather than allowing her abdomen to expand. When she first started to practice diaphragmatic breathing, it felt unfamiliar, unnatural and at times uncomfortable because she had unconsciously grown so accustomed to breathing predominantly in her chest.
After she learned to practice slower diaphragmatic breathing by allowing her abdomen to expand naturally during inhalation, her acid-reflux symptoms decreased. She also used imagery to describe what she experienced, stating that her lungs were like a balloon located in her abdomen. To create space for the diaphragm going down, she bought larger size pants so that her abdomen could spread out instead of squeezing her stomach.
In a follow-up one year later, she continued to incorporate diaphragmatic breathing and reported no symptoms of acid reflux.
Before learning abdominal breathing techniques using biofeedback training, she had to restrict her diet by avoiding certain foods. However, after having little to no symptoms of acid reflux, she started eating foods that would previously have caused irritation. Now, she is able to eat spicy or acidic foods, and drink alcohol without having GERD symptoms or affecting her stomach at all.
She had become aware that her tight clothes contributed to adding pressure around her abdomen and shifted wearing looser fitting clothes to alleviate the pressure on her stomach (Kahrilas, Talley & Grover, 2016). Whenever she felt that she was about to have an episode of acid reflux, she practiced techniques learned with biofeedback training to calm down and focus on her breathing, keeping her hands on her stomach, feeling it expand, and making sure she’s not tightening her abdomen. She reported being more mindful of her breathing, able to immediately notice when she holds her breath or breathe thoracically, and able to remind herself to take deep breaths from the abdomen.
To prevent problematic symptoms from returning, she practiced diaphragmatic breathing many times during the day. In addition, the moment she felt stressed and tightened her abdomen, she interrupted this tightening and re-established abdominal breathing. Practicing this was very challenging since she had to accept that she would still be attractive even if her stomach expanded during inhalation. In addition, each time she slouched, she shifted to an erect position that also allowed her abdomen to expand. (To appreciate the challenges involved and how to integrate breathing and awareness into daily life, watch her interview: https://peperperspective.com/?s=acid+reflux. Also, for a detailed description how this approach successfully cured irritable bowel see: https://peperperspective.com/2017/06/23/healing-irritable-bowel-syndrome-with-diaphragmatic-breathing/.)
Conclusion
A major reason why this case study was successful is that the student integrated the breathing pattern into her daily life. This meant buying looser fitting clothing and shifting to slow diaphragmatic breathing when she became aware of breathing in her chest as a reaction to stress or feeling an increase in abdominal pressure. What would be necessary for a simple behavioral breathing intervention to be the first strategy in the treatment of acid reflux? An obvious answer would be training practitioners to incorporate breathing biofeedback techniques into their practice. Participants, patients and clients should be trained to increase diaphragmatic breathing and to interrupt gasping and chest breathing patterns during the day. Using not only diaphragmatic breathing biofeedback training, but also heart rate variability (HRV) training could be a simple intervention for GERD (Keefer, 2018; Lerner & Wilner, 2017; Sun et al, 2016). Slower diaphragmatic breathing with the corresponding abdomen movement at about six breaths per minute helps reduce autonomic dysregulation and increase vagal tone. Healthy breathing regulation has profound self-healing effects that accrue over the lifetime. Whereas breathing biofeedback was found effective for reversing the symptoms of GERD in a college student, the principles of biofeedback training are applicable across a broad range of symptoms, from GERD to autonomic dysregulation. Holistic health treatment techniques that focus on behavioral approaches, including biofeedback training, should be taught as first-line interventions as a complement to all other healing arts.
*Correspondence should be addressed to Erik Peper, PhD, Institute for Holistic Healing Studies/Department of Health Education, San Francisco State University, 1600 Holloway Avenue, San Francisco, CA 94132. Tel: 510 681 6301; Email: epeper@sfsu.edu; Web: www.biofeedbackhealth.org; Blog: www.peperperspective.com