By Jeremy Mikolai, ND
Carnitine is a general term used to refer to the amino acid derivative L-carnitine (LC) and its closely related metabolic counterparts, acetyl-l-carnitine (ALC), and propionyl-l-carnitine (PLC). Participation of LC/ALC in shuttling of fatty acids into mitochondria for beta-oxidation is well known and largely understood, but its participation – and that of its derivatives – in other body processes is less completely understood. However, the therapeutic applications for these agents in diverse pathologies of any age and gender cannot be overstated. Their efficacy has been demonstrated on important pathologies of the cardiovascular system, peripheral vascular system, nervous system, in the redress of infertility in both males and females, and in several conditions that are specific to the male urogenital organs. We will consider two of these areas: Peyronie’s disease (PD) and erectile dysfunction (ED).
Propionyl-l-carnitine (PLC) is a derivative of L-carnitine. As a manufactured agent, it is most often delivered as glycine propionyl-l-carnitine (GPLC). Its therapeutic effect has several important applications in the vascular system, including in the treatment of peripheral vascular disease (PVD), healing of ulcers from PVD, improved walking distance in intermittent claudication, congestive heart failure, and angina.1-5 Repeated studies show PLC supplementation increases circulating nitrate.6 More nitrate does not prove increased vasodilation or conclusively elucidate one or more mechanisms of action for the therapeutic effect of PLC, yet its effect on diseases of ischemic pathophysiology are demonstrable.
Peyronie’s disease (PD) is a fibrotic disorder of the tunic albuginea (TA) of the penis resulting in pain, penile deformity (especially during erection), and palpable changes/nodularity at the areas of local fibrosis. The causes of PD are incompletely understood, but several risk factors are known including local ischemia and previous trauma. PD is not uncommon and may affect 3-9% of the male population, likely more. PD is characterized by an acute phase of 12 months, which often includes pain, and a chronic phase thereafter in which pain may resolve but in which deformity and plaque formation may progress. Erectile dysfunction is a common co-morbidity of PD.7
Interlesional injections appear to be the present minimally invasive treatment of choice for PD with interferon preparations showing significant effects on penile curvature, plaque size, penile pain, and erectile function. Surgical correction is typically reserved for disease that has progressed over at least 12 months and results in penetrative inability or other severely impaired sexual satisfaction. The procedure of choice is often incision and grafting, especially with multifocal disease, severe curvature, or desire not to suffer loss of penile length resulting from other procedures.
Cavallini et al (2002) evaluated the efficacy of PLC (2 g/day) versus tamoxifen (40 mg/day) for three months in 60 patients, all of whom were also receiving interlesional verapamil infiltrations (10 mg/wk) for 10 weeks. Another group of 15 individuals with resistant PD were treated with the verapamil/PLC regimen. In both groups taking PLC, significant improvements were seen in penile curvature, plaque size, disease progression, and International Index of Erectile Function (IIEF) scores. None of these effects were seen in the tamoxifen group.8
Peyronie’s disease, which affects 3-9% of men, can improve with
supplemental acetyl-l-carnitine/propionyl-l-carnitine treatment
While Cavallini study above was published in 2002, the Gokce et al review (2013) of Peyronie’s disease demonstrates no significant effect on PD from either interlesional verapamil injections or oral tamoxifen.7 A 2007 study by Safarinejad demonstrated no significant effect from PLC versus vitamin E on similar outcomes in PD.9 More recent data supports a dose of 3-3.5 grams/day of PLC as necessary for likely improvement in PD.7
Biagiotti and Cavallini previously studied the effect of ALC in 48 PD patients randomized to two groups, one taking ALC 1 g two times/day, one taking tamoxifen 20 mg two times/day, each for three months. Their results demonstrated significant improvements in pain and disease progression, penile curvature, and plaque size in the ALC group versus only decreased plaque size in the tamoxifen group, which also had significantly more side-effects.10
Acetyl-l-carnitine (ALC) is derived from the acetylation of carnitine and is used as a coenzyme A (CoA) donor in the mitochondria as acetyl CoA combines with carnitine to form ALC, which is transported out into the cytosol leaving CoA available for further beta-oxidation of fatty acids.
ALC has diverse and complex action upon the nervous system ranging from antiapoptotic effects to nerve regenerative properties, including increased neuronal structural element synthesis, increased growth factor sensitivity, and analgesic action that may be attributable to a reduction of glutamate in the neuronal synapse.11
ALC is a neuropathy intervention par excellence; it demonstrates effect in nerve damage repair and nerve regeneration in primary trauma as well as in chronic neuropathies such as diabetic neuropathy. A 2017 review by Veronese et al demonstrated that, in a review of 711 patients with diabetic neuropathy, ALC oral supplementation resulted in improved pain perception as well as improved motor and sensory nerve conduction velocities and amplitudes. In other words, ALC resulted in improved nerve function.12
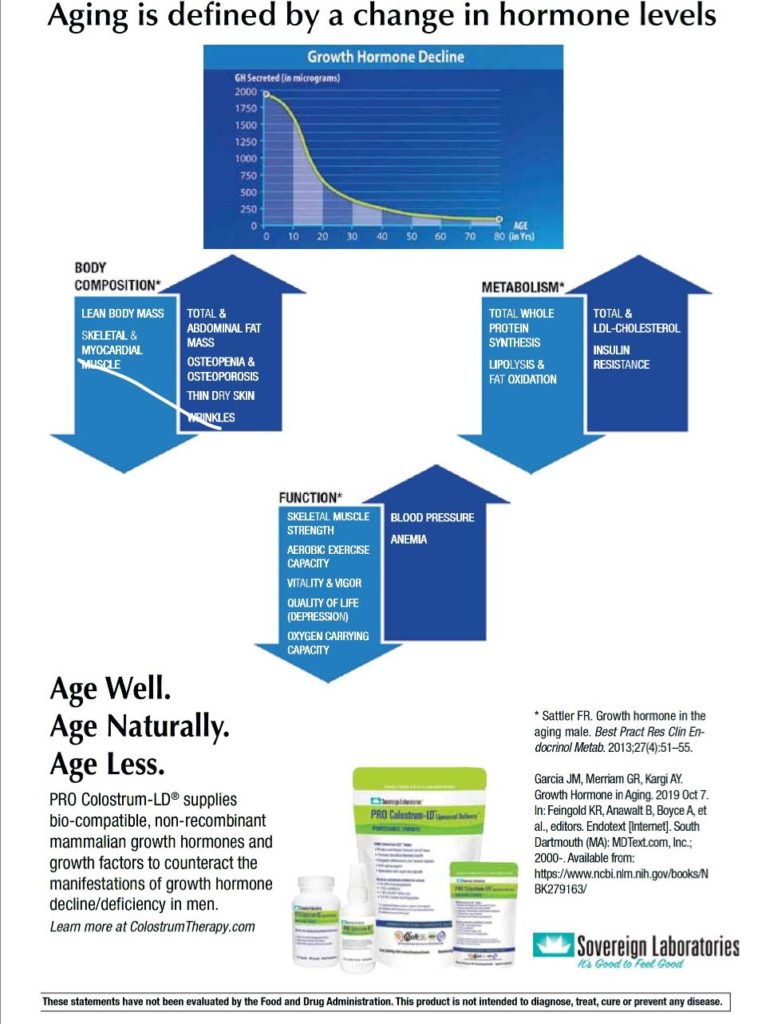
Vasodilator activity may explain the role of PLC in the improvement of male sexual dysfunction, erectile dysfunction, and some symptoms of decreased sex hormone production with age (“andropause”); but that mechanism does not seem to explain all of the effects of the combination of PLC and ALC in the treatment of these disorders. None the less, oral supplementation of 2 grams/day each of ALC and PLC has demonstrated profound effects on male sexual function and associated symptoms.
Compared to supplementation with either high dose testosterone intramuscular injection or placebo, supplementation of ALC/PLC for six months demonstrated significantly superior results compared to testosterone on improvements in nighttime erections and IIEF score. Both testosterone and ALC/PLC were superior to placebo on numerous outcomes, including peak end systolic and diastolic blood flow velocities, resistive index, nighttime erections, IIEF score, Depression Melancholia Scale score, and fatigue scale score.13
It is important to note that the Huo et al (2016) review found that there is no significant benefit to sexual function, mood, psychological well-being, or cognitive function resulting from testosterone supplementation in men with low testosterone.14
Erectile dysfunction is a common disorder in men, especially aging men, and may be primary or secondary in its cause or often both. While psychological factors are virtually ubiquitous as contributing or propagating factors, the initiating insult may be psychological, metabolic, vascular, nervous system, or primary urogenital in origin. It may be secondary to trauma, iatrogenic intervention, T2D, high blood pressure, high cholesterol, vascular disease, nerve damage and other issues.
The development of 5-phosphodiesterase inhibitors (5-PDEi) such as sildenafil and tadalafil revolutionized the treatment of erectile dysfunction in men, though these agents do not work for every individual. Intracavernosal injections of trimix (combination of alprostadil-prostaglandin, papaverine-vasodilator, and phentolamine-alpha adrenergic blocker) are effective for some men who fail oral 5-PDEi therapy.
Prostatectomy is a primary iatrogenic cause of erectile dysfunction in men with a history of prostate cancer or severe benign prostatic hyperplasia. Regardless of the method of resection, nerve damage and erectile dysfunction are always risk factors. Cavallini et al (2005) studied 96 patients who had undergone bilateral nerve-sparing radical retropubic prostatectomy in three groups. Group 1 took a placebo, group 2 took 2 grams/day each of PLC and ALC as well as sildenafil 100 mg as needed for sexual activity, while group 3 took only 100 mg sildenafil as needed.15
While both groups 2 and 3 had significant improvement in IIEF score, group 2 scores were significantly greater than group 3 in erectile function, satisfaction, orgasm, and sexual well-being. The percentage of each group reporting satisfactory sexual intercourse were 7%, 88%, and 51%, respectively. Moreover, only the ALC/PLC treatment group demonstrated improvements in intracavernous injection tests after the treatment period—again, signaling that ALC/PLC is affecting an improvement of this natural function, a healing, which is not occurring in other treatment contexts.
Case Reports
Case 1: Mike was a 41-year-old male with a six-year history of Peyronie’s disease, which he felt began with a flare of psoriasis. He reported extreme pain and phimosis for the first year, followed by a severe hour-glass restriction circumferentially around the shaft of the penis just proximal to the glans penis with painful erection, limitation of erection size, and sexual satisfaction. A 1 mm round palpable nodule fixed within the TA was appreciable. His history was also significant for untreated mild-moderate recurrent major depression, type 2 diabetes mellitus (T2D) that was moderately controlled through diet and exercise, moderate plaque psoriasis, and a remote history (11 years prior) of penile fracture, which was treated with non-surgical conservative management and presumed to have healed completely.
Mike started GPLC 1,500 mg twice daily and ALC 500 mg twice daily. He reported increased libido and decreased depression and fatigue within the first week of use. At four weeks follow up, he reported a 25% improvement in erection size and early signs of resolution of his fibrosis, including painless erections, lack of skin breaks, and resolution of some fibrosis. At eight-weeks follow up, Mike had near resolution of all symptoms with continued improvements in fatigue and depression. While his TA nodule was still palpable at eight weeks, it was resolved completely by the six-month follow up visit. Mike had no reported negative off-target effects.
Case 2: Patrick was a 23-year-old male newlywed and recently graduated engineer with ADHD that was well-controlled on guanfacine, 2 mg every night at bedtime. He complained of erectile dysfunction, including difficulty reaching full tumescence, difficulty maintaining tumescence, and anorgasmia as well as premature ejaculation. He continued to have nighttime erections. He had no significant physical exam or laboratory abnormalities. He had a history of incompletely controlled irritable bowel syndrome without red flags and no other significant personal, social, medical, or family history.
Patrick started ALC/PLC, 1/1.5 grams two times per day. Within one week he reported complete improvement in sexual function and also reported significant gastrointestinal side effects, primarily loose stools. He stopped the ALC/PLC protocol, and we addressed this acute issue. He continued to have improvement in sexual function for several weeks and then decided to resume ALC/PLC, which he did without side effects and with return to what he considered to be full improvement for several more weeks of treatment. He was then able to discontinue treatment with continued full satisfactory function.
Case 3: Clint was a 59-year-old male who was referred to me for cardiac evaluation after he was found to have unexplained fluctuating NT-proBNP levels; our work-up revealed severe asymptomatic three-vessel coronary artery disease. He had only recently sought care and was under treatment but, at this time, was severely hypertensive, hyperlipidemic, and diabetic with a HgbA1c over 10%. He was seen by a cardiothoracic surgeon, had a very successful three-vessel bypass surgery, a very rapid recovery, and was seen for follow up less than three months after surgery with no pain, exercising daily, controlled blood sugar and blood pressure, on 10 mg of rosuvastatin, but no other medications and asking to address erectile dysfunction. He had tried Trimix, which had worked for him but was not of routine interest to him; he had failed sildenafil oral tablet at an unknown dose. He began ALC/PLC 1/1.5 gram, two times per day; after one month without improvement, he doubled his dose. After two months of treatment, he was lost to follow up without known improvement.
I discussed with this patient that it would be optimistic to expect the ALC/PLC protocol to show significant results in less than six months, but I certainly do expect that he would have had appreciable improvement over a longer treatment period. The logical next step in his case would have been to clear him for sexual activity (with his cardiologist or surgeon, or to order or perform an exercise tolerance test) and then prescribe a 5-PDE inhibitor of adequate dose and dosage form for an adequate trial as he may well benefit from combination treatment even having previously failed 5-PDEi alone.
In the integrative management of Peyronie’s disease, as well as in almost every case of erectile dysfunction, there is a central place for the therapeutic application of ALC and PLC. Moreover, in virtually every case necessitating these agents, the skilled clinician will likely find their appropriate application leads to the improvement of one or more important comorbid conditions.
Jeremy Mikolai graduated with highest honors from the National College of Naturopathic Medicine in Portland, Oregon in 2010. He then completed three years of clinical residency training, including one year as chief resident. His clinical training focused on family practice integrative medicine with extensive additional training in cardiovascular diseases. Following residency, he completed an additional year of integrative cardiology fellowship.
https://www.sequoianaturalmedicine.com
References
1. Brevetti G, et al. Superiority of L-propionylcarnitine vs L-carnitine in improving walking capacity in patients with peripheral vascular disease: an acute, intravenous, double-blind, cross-over study. Eur Heart J. 1992;13:251-5.
2. Persico G, et al. The early effects of intravenous L-propionyl carnitine on ulcerative trophic lesions of the lower limbs in arteriopathic patients; a controlled randomized study. Drugs Exp Clin Res. 1995;21:187-98.
3. Brass EP, et al. A systematic review and meta-analysis of propionyl-l-carnitine effects on exercise performance in patients with intermittent claudication. Vasc Med. 2013;18:3-12.
4. Anand I, et al. Acute and chronic effects of propionyl-l-carnitine on the hemodynamics, exercise capacity, and hormones in patients with congestive heart failure. Cardiovasc Drugs Ther. 1998;12:291-9.
5. Bartels GL, et al. Anti-ischaemic efficacy of L-propionylcarnitine- a promising novel metabolic approach to ischaemia? Eur Heart J. 1996;17:414-20.
6. Bloomer RJ, Tschume LC, Smith WA. Glycine propionyl-L-carnitine modulates lipid peroxidation and nitric oxide in human subjects. Int J Vitam Nutr Res. 2009;79(3):131-41.
7. Gokce A, et al. Current and emerging treatment options for Peyronie’s disease. Res Rep Urol. 2013;5:17-27. Published online 2013 Jan 14.
8.. Cavallini G, et al. Oral propionyl-l-carnitine and intraplaque verapamil in the therapy of advanced and resistant Peyronie’s disease. BJU Int. 2002 Jun;89(9):895-900.
9. Safarinejad MR, Hosseini SY, Kolahi AA. Comparison of vitamin E and propionyl-L-carnitine, separately or in combination, in patients with early chronic Peyronie’s disease: a double-blind, placebo controlled, randomized study. J Urol. 2007 Oct;178(4 Pt 1):1398-403; discussion 1403. Epub 2007 Aug 16.
10. Biagiotti G, Cavallini G. Acetyl-L-carnitine vs tamoxifen in the oral therapy of Peyronie’s disease: a preliminary report. BJU Int. 2001;88:63–67.
11. Sergi G, et al. Effects of acetyl-L-carnitine in diabetic neuropathy and other geriatric disorders. Aging Clin Exp Res. 2018 Feb;30(2):133-138.
12. Veronese N, et al. Effect of acetyl-l-carnitine in the treatment of diabetic peripheral neuropathy: a systematic review and meta-analysis. Eur Ger Med. 2017;8(2):117-122.
13. Cavallini G, et al. Carnitine versus androgen administration in the treatment of sexual dysfunction, depressed mood, and fatigue associated with male aging. Urology. 2004 Apr;63(4):641-6.
14. Huo S, et al. Treatment of Men for “Low Testosterone”: A Systematic Review. PLoS One. 2016; 11(9): e0162480.
15. Cavallini G, et al. Acetyl-L-carnitine plus propionyl-L-carnitine improve efficacy of sildenafil in treatment of erectile dysfunction after bilateral nerve-sparing radical retropubic prostatectomy. Urology. 2005 Nov;66(5):1080-5.