by Scott Forsgren
Portions from an interview with B. Robert Mozayeni, MD
As someone who struggled with Bartonella for many years, I know all too well the devastation that this infection can have on one’s physical and mental health. While Bartonella can manifest in many different ways within the body, the challenges it presents extend far beyond the physical.
Bartonellosis is a poorly understood condition that is routinely overlooked by mainstream medicine. As a result, many cases go undiagnosed, leading to significant and unnecessary human suffering and substantial costs to society. While available testing options for Bartonella have improved greatly in recent years, there is still no perfect Bartonella assay available. Even when bartonellosis is confirmed through testing, the success of available treatment options is variable, and Bartonella may establish itself as a chronic infection that requires long-term management.
Fortunately for many of us, humans are not the only species affected by the genus Bartonella. In fact, much of the available research comes from the veterinary community, where Bartonella is much more widely acknowledged and better understood than in human medicine.
Veterinary Medicine Leads to Help for Suffering Humans
Edward Breitschwerdt, DVM, is an infectious disease specialist at North Carolina State University College of Veterinary Medicine, an adjunct professor of medicine at Duke University, and chief scientific officer at Galaxy Diagnostics. Early in his career, he focused on vector-borne, intracellular pathogens, including Rocky Mountain spotted fever (caused by a Rickettsial bacterium) and Ehrlichia. Ehrlichia was discovered in animals decades before it was identified in humans. His attention later shifted to Bartonella due to the historical association of one Bartonella species, Bartonella henselae, with cat-scratch disease (CSD).
The connection between the newly discovered bacterium and CSD was initially made by a rickettsiologist, Dr. Russ Regnery at the CDC, who recognized similarities between a newly isolated bacterium from an AIDS patient in Texas and bacteria visualized in lymph nodes of patients with CSD. Regnery made the first isolate of Bartonella henselae from a cat and showed that cats can become chronically infected. This work was the catalyst that led Breitschwerdt down the path of unraveling the mysteries of Bartonella.
As Breitschwerdt lectured at veterinary conferences about Bartonella illnesses in dogs, numerous veterinarians approached him to discuss their own health challenges, such as multiple sclerosis-like conditions and rheumatoid-like diseases. Many had been sick for several years with no clearly defined diagnosis. When he started testing these veterinarians for Bartonella, his research team found that many of them tested positive for Bartonella DNA in their blood. If it were not for the translational research initially done with animals, the genus Bartonella and the disease bartonellosis would likely be even lesser known than they are today. This may be another example in which dogs truly are man’s best friend. Over the next two decades, research would demonstrate that dogs often develop the same pathologies as those of their human counterparts.
Bartonella Basics
Bartonella was named after A. L. Barton, who in 1909 identified organisms that adhered to red blood cells. Bartonella is a genus of gram-negative, aerobic bacteria belonging to the Bartonellaceae family and Rhizobiales order. It is in the Alphaproteobacteria class, which is part of the Proteobacteria phylum. Bartonella organisms are considered facultative intracellular parasites, meaning that they may resort to parasitic activity although they do not rely on a host to complete their life cycle. Other well-known pathogenic Alphaproteobacteria include Rickettsia, Anaplasma, Ehrlichia, and Brucella species.

While Bartonella can infect healthy people, it has generally been believed by mainstream medicine that the infection is cleared by the immune system in the majority of cases. Many view these bacteria as opportunistic pathogens in conditions wherein the immune response may be suppressed, such as in AIDS and chronic Lyme disease. As the ability to identify Bartonella has improved, patients with numerous long-term illnesses have been found to harbor the bacteria in their blood and tissues. Additional research is needed to determine what role Bartonella plays in these illnesses. Persistent bloodstream infection with numerous Bartonella species is increasingly being linked to a host of chronic illnesses.
Bartonella targets erythrocytes (red blood cells), endothelial cells, microglial cells, macrophages, and CD34 progenitor cells.1 Once the infection is in the body, it commonly resides in red blood cells and in the endothelial and pericyte cells lining the blood vessels throughout the body. Bartonella may use these cells and various tissues in the body to hide from the immune system and to establish a chronic, persistent infection.
Bartonella and Human Infection
According to Breitschwerdt, there are nearly 40 different species of Bartonella known today, and 15 of these have been found to infect human beings (see Table 1). The more commonly known Bartonella species include Bartonella henselae, Bartonella quintana, and Bartonella bacilliformis.
Bartonella henselae is the causative agent in CSD. In addition, this Bartonella species can cause numerous symptoms in both immunocompetent and immunocompromised individuals. Infection may result in bacteremia (presence of bacteria in the blood), myocarditis (inflammation of the middle layer of the heart wall), peliosis hepatis (a vascular condition which results in blood-filled sacs in the liver), neuroretinitis (inflammation of the neural retina and optic nerve), bacillary angiomatosis (a proliferation of blood vessels leading to tumorlike masses), enlarged lymph nodes, and fevers.
Bartonella quintana is known as the causative agent in trench fever. It was first described during World War I as over a million soldiers in Europe became infected after exposure to the human body louse. Urban trench fever has reemerged among homeless populations around the world. It may present with fever, severe headaches, back and leg pain, and skin rashes. It can be a factor in endocarditis and may result in bacillary angiomatosis in those coinfected with HIV. Evidence of Bartonella quintana has been found in the dental pulp of soldiers from Napoleon’s Grande Armée, and many of his soldiers died from infectious diseases, including trench fever and epidemic typhus (Rickettsia prowazekii).2
Bartonella bacilliformis leads to a condition known as Carrión’s disease, or Oroya fever. Carrión’s disease was named after Daniel Alcides Carrión, a Peruvian medical student who died after an experiment where he inoculated himself with the bacterium. Bartonella bacilliformis is found primarily in Peru, Columbia, and Ecuador and is transmitted by sand flies. It can have a mortality rate of 40% to 90% in untreated patients.
More recently, other Bartonella species have been associated with human infection. Bartonella clarridgeiae may lead to CSD. Bartonella elizabethae, Bartonella vinsonii subsp. berkhoffii, and Bartonella vinsonii subsp. arupensis may be factors in endocarditis. Bartonella grahamii has been found in the ocular fluids of a human with neuroretinitis.3 Bartonella washoensis has been implicated in myocarditis.4
Candidatus (an interim status for a yet-to-be officially named organism) Bartonella melophagi was discovered in 2009 by Dr. Ricardo Maggi, a research microbiologist working with Breitschwerdt, while testing human blood specimens.5 Candidatus Bartonella mayotimonensis has been identified in a case of endocarditis, and recent evidence suggests that bats may be the reservoir for this Bartonella species.6,7 In that research publication, a compelling statement was made: “This case reinforces the hypothesis that any Bartonella species can cause human infection.”
Human infection with Bartonella may be the result of arthropod vectors, including fleas (and flea feces), biting flies such as sand flies and horn flies, the human body louse, mosquitoes, and ticks; through bites or scratches of reservoir hosts; and potentially from needles and syringes in those who are drug addicted. Needle stick transmission to veterinarians has been reported. Bartonella henselae and Bartonella clarridgeiae have been transmitted to cats through blood transfusion. Recently, 3.2% of healthy blood donors in Brazil were found to carry at least one of these two cat flea-associated Bartonella species in their blood.8 Bartonella DNA has even been found in dust mites.9 Fleas have been shown to be infected with Bartonella henselae, Bartonella clarridgeiae, Bartonella koehlerae, and Bartonella quintana; body lice with Bartonella quintana; and ticks with several species of Bartonella.10 Vector biologists and others with extensive arthropod exposures are at increased risk for acquiring Bartonella infections.
Working or living with flea-infested pets or other animals is a notable risk factor for Bartonella, so much so that up to 28% of veterinarians tested positive in one study compared with 0% of controls.11 Cats and dogs exposed to arthropod vectors and that live in close proximity with people put humans at increased risk for acquiring Bartonella infections. The concentration of Bartonella in the blood of an infected cat may be as high as a million times that of an infected human. Recent evidence indicates that many of the Bartonella henselae strains that commonly infect cats are not found in humans, suggesting that virulence factors play an important role in determining pathogenicity and whether or not a cat poses a risk for transmission of a pathogenic strain to a human.
Animals that are exposed to fleas and ticks have a high likelihood of being infected with Bartonella. About half of all cats may be infected with Bartonella, as high as 80% of feral cats and near 40% of domestic cats.12,13 In one study that tested 108 domestic dogs in Peru serologically, 67 of the dogs were seropositive for Bartonella rochalimae, while 43 dogs were seropositive for B. vinsonii berkhoffii.14 In a study of dogs in Iraq, the seroprevalence of Bartonella infection was 47.4%.15 An incidence of 10% has been reported in healthy dogs in the eastern United States, and 35% of coyotes were seropositive for B. vinsonii subsp. berkhoffii in California, with 28% being bacteremic.16
Additionally, although presumably an infrequent mode of transmission, evidence now suggests that Bartonella may be transmitted from mother to child in utero, potentially leading to birth defects.17
Bartonella Symptoms
The symptoms of Bartonella may affect numerous body systems and can range from mild to severe, and may even be fatal.18 Breitschwerdt’s own father passed away from complications associated with Bartonella infection.19 One may be asymptomatic or may never become symptomatic enough to pursue medical evaluation. Presenting symptoms may wax and wane over time.
The more common symptoms of Bartonella include swollen lymph nodes, gastritis, sore soles of the feet most noticeable in the morning, fasciculations (muscle twitching), headaches, abdominal pain, striae (irregular areas of skin that look like stretch marks), skin rashes, tender subcutaneous nodules in the extremities, fevers, anxiety, depression, anger, and obsessive-compulsive thoughts or behaviors.
B. Robert Mozayeni, MD, has a private rheumatology practice in Rockville, Maryland, and is a leading expert in the treatment of Bartonella. He serves as chief medical officer for Galaxy Diagnostics and works closely with Breitschwerdt. In a recent interview for this article, Mozayeni explained that he sees a pattern of symptoms in his patients with Bartonella infection. He noted that bartonellosis is primarily an infection of the blood vessels, the blood components, and the bone marrow. While Borrelia burgdorferi, the causative agent in Lyme disease, can be found in the blood and as well as outside the vascular system, Bartonella species primarily congregate within red blood cells, endothelial cells, and bone marrow cells. It may also be found in cysts, having been isolated from an otherwise “benign” breast cyst in one patient.
As bartonellosis is principally an infection of the vascular system, it leads to inflammation and endothelial proliferation, disrupting blood flow at the small vessel level, such as in the capillaries and arterioles. The end result is compromised microcirculation throughout the body which can lead to the appearance of fluctuating and migrating symptoms. The manifestation of symptoms is largely associated with where in the body the blood flow compromise happens to be located.
Pain in the soles of the feet upon waking, for example, is likely due to inflammation of the blood vessels in an area that endures ongoing microvascular trauma as a result of regular weight-bearing activity; the pain is then exacerbated by the presence of Bartonella and small vessel inflammatory disease.
Patients may present with POTS (postural orthostatic tachycardia syndrome) or other forms of dysautonomia wherein the autonomic nervous system is affected; this is another manifestation of small vessel disease. The nerves of both the sympathetic and parasympathetic nervous system are compromised in their function due to changes in microcirculation and interruption in blood flow.
In every patient, Bartonella is infecting the vascular system throughout the body. Endothelial infection with Bartonella can damage veins and the valves of veins. Endothelial cells also line the heart valves. However, such infection can progress to infiltrate the deeper connective tissue of the heart in rare cases. This type of deeper heart valve infection with Bartonella is usually detected too late and almost always leads to heart valve replacement surgery. In a recent study of healthy coyotes in California, Bartonella DNA was found in the heart valves of 17% of the coyotes studied, and DNA of the bacterium was preferentially amplified from the aortic valve, the valve most commonly involved in both dog and human endocarditis.20 Fortunately, as a rheumatologist, Mozayeni has not seen anyone in his patient population who has developed serious heart valve complications as a result of Bartonella infection.
Some believe that devitalized teeth and jawbone cavitations may be associated with Bartonella infection. Mozayeni collaborates with an endodontist who indicated that Bartonella “is big in the endodontal scientific literature,” as it is known to cause cysts around dental roots that may lead to chronic, hard-to-diagnose head and face pain. Additionally, Mozayeni has observed a very high incidence of root canals in his practice which may be related to a compromise of small blood vessels that feed the dental pulp, another manifestation of small vessel disease. Although a single case report, a veterinarian infected with Bartonella henselae and Bartonella vinsonii subsp. berkhoffii developed neurological symptoms and periodontal disease concurrently.21
Numerous symptoms that have been associated with human Bartonella infection are listed in (see Table 2). Although incompletely studied at this time, there may be variations in symptom presentation depending on the specific Bartonella species involved, the virulence of the infecting strain, the status of the host immune response, and, as noted, where in the body the microcirculation is most impaired.
Bartonella and Psychological Manifestations
Bartonella patients often describe a number of psychoemotional manifestations of the infection. These may include anxiety, depression, anger, obsessive-compulsive thoughts or behaviors, rage, and even suicidal thoughts.
Mozayeni shared that small vessel disease manifests in the central nervous system and the brain and affects executive function, often leading to mild or moderate cognitive impairment. As people become increasingly unable to process information, anxiety may develop. While there is generally no dementia or long-term memory impairment, short-term working memory and reaction time are often affected. “People become unable to think their way out of a negative thought, which leads to anxiety and fear,” shared Mozayeni.
Mozayeni has said, “Many neuropsychiatric conditions can often be traced back to an infectious cause.” A common pattern may be that a patient initially presents with anxiety, which goes hand in hand with depression if not treated. They are two sides of the same coin. Over time, as a result of overstimulation, neurotransmitter depletion may lead to depression.
In a recent post on his blog, “LymeMD,” Daniel A. Jaller, MD, stated, “Bartonella, as I know it, is frequently associated with specific neuropsychiatric symptoms, which may include: irritability, anxiety, rage and many others.”31
More and more clinicians are beginning to recognize the impact of Bartonella on psychological well-being. Further research is needed to validate what these experienced clinicians have observed and to highlight that Bartonella‘s impact extends far beyond its physical manifestations. Many of those that have personally experienced Bartonella can attest to having experienced a number of these distressing neuropsychiatric symptoms.
Bartonella Testing
Bartonella presents a diagnostic challenge for clinicians. A number of different laboratory tests exist to support the confirmation of Bartonella infection. However, cases of Bartonella infection may exist even when available tests are negative. Although current diagnostic tests have limitations, it is of critical importance to attempt to confirm a diagnosis of bartonellosis before embarking on a long, costly, and complex treatment regimen. As has been stated in the medical literature for many decades, “The kindest form of therapy is an accurate diagnosis.”
The first option is an antibody test looking for IgM and IgG antibodies in serum using an indirect fluorescent antibody (IFA). Many commercially available antibody tests focus primarily on Bartonella henselae and Bartonella quintana, a small subset of the Bartonella species that can cause human disease. Bartonella testing that relies on an antibody response is generally not very sensitive, as Bartonella has many properties that allow it to evade the immune system. Diagnostically relevant production of antibodies is not generally observed with Bartonella infection. As many as 85% of those chronically infected with Bartonella, confirmed through DNA amplification of blood or tissue, may have negative test results with IFA assays (for antibody detection).32 Further, there is a potential for cross-reactivity between Bartonella and other organisms such as Coxiella burnetii and Chlamydia, which further complicates interpretation of the results.33 Furthermore, antibodies indicate evidence of prior exposure and do not confirm active infection.
Traditional PCR testing for Bartonella is available, though these assays were designed to only detect Bartonella henselae and Bartonella quintana DNA in the patient’s specimen, thus potentially missing many cases of Bartonella infection. Another challenge with traditional PCR testing is that Bartonella often infects humans at very low levels, making it difficult to detect with standard PCR techniques.
Three of the top specialty laboratories for Bartonella testing include Fry Laboratories, Galaxy Diagnostics, and IGeneX.
Fry Laboratories (Scottsdale, Arizona) offers IgM and IgG IFA testing for Bartonella as well as Bartonella PCR testing using molecular diagnostics. The Bartonella spp. by PCR testing screens for numerous clinically relevant species of Bartonella using a genuswide PCR method. Additionally, they offer assays using a modified May-Grünwald and other stains; however, these stains are not specific for Bartonella.
Galaxy Diagnostics (Research Triangle Park, North Carolina) has emerged as one of the more recent options for Bartonella testing. Its ePCR panel uses the BAPGM (Bartonella alpha-Proteobacteria growth medium) platform to optimize results. Bartonella are usually present in very low numbers. Therefore, an initial step to culture the blood and “enrich” the number of “copies” of Bartonella is usually necessary to enable PCR detection. Three of four positive tests are usually enabled by the enrichment culture step. All PCR-positive results are confirmed by DNA sequencing to confirm Bartonella and to identify the species. Galaxy specializes in Bartonella testing and has emerged as a leader in the field.
IGeneX Inc. (Palo Alto, California), a respected laboratory in vector-borne infections, offers IgM and IgG IFA testing, PCR testing, and a Bartonella FISH (fluorescent in situ hybridization) assay. The advantage of the FISH assay is that it looks for Bartonella RNA and thus does not rely on the response of the host immune system in order to identify the presence of the organism.
It has been suggested that vascular endothelial growth factor (VEGF) may be elevated in a subset of those infected with Bartonella.34 It is believed that Bartonella may produce VEGF to stimulate its growth in the endothelium or VEGF may result from endothelial inflammation and infection. There may be an association between Bartonella-induced VEGF and various skin lesions such as bacillary angiomatosis or even striae. Some have suggested that monitoring VEGF throughout treatment may serve as an indicator of treatment progress, but Mozayeni has not found this to be a consistently reliable marker.
Mozayeni has found that patients solely infected with Bartonella can have elevated C4a levels, an inflammatory marker commonly high in patients with Lyme disease or those with biotoxin illnesses such as mold illness.
Galaxy Diagnostics ePCR
With the Galaxy ePCR Panel, there has been a confirmed positive rate of 9.2% as compared with only 0.98% for traditional PCR testing Conventional IFA testing identifies exposure but cannot confirm presence of active infection In terms of sensitivity, the ePCR is reported to be 10 times more sensitive than PCR and is 100% specific; each positive ePCR test result is confirmed by DNA sequencing Conventional IFA testing is reportedly only 66% to 76% specific, which means that even when the result is positive, it may not be the result of Bartonella infection.
There is a cyclical nature of Bartonella bacteremia that may influence test results Bartonella generally resides in the tissues that line the blood vessels and is not consistently found in the bloodstream This makes testing more difficult and potentially leads to higher false negative test results This drawback is minimized by Galaxy’s True Triple Draw which collects three blood samples over a 7 to 8-day period to maximize test performance The ePCR is believed to have a 90% reduction in false negatives as compared with conventional PCR testing
In order to optimize the sensitivity of the testing, it is recommended that patients be tested prior to starting antibiotics or be off all antimicrobial therapies, including antimicrobial herbs, for 2 to 4 weeks prior to the blood draws Bartonella exists in human blood in very low amounts and maximizing the numbers in the blood optimizes test results
For those with chronic Bartonellosis, the ePCR test panel is an ideal tool as compared with conventional IFA testing which generally has high false negative rates for chronically infected individuals IFA testing may be a better option for classical CSD.3
Bartonella is a stealth infection The bacteria have a long division time of around 22 to 24 hours which makes diagnostic testing much more difficult as compared with testing of more rapidly dividing bacteria A special growth environment was needed for Bartonella species, and it was an innovation from Breitschwerdt’s research team at North Carolina State University College of Veterinary Medicine that led to a new culture medium. Considering that Bartonella is often found in sand flies, fleas, lice, and other insect vectors, an insect biochemical composition was evaluated as opposed to a conventional mammalian growth medium. This became the “secret sauce” of the Galaxy Diagnostics ePCR platform and is known as BAPGM (Bartonellaalpha-Proteobacteria growth medium) With this enrichment medium, Bartonella is exponentially grown to levels that can be detected with a PCR assay, making false negative test results much less common, even in those with low levels of Bartonella
The Galaxy Bartonella ePCR is designed to detect all known pathogenic Bartonella species Although blood is the most readily available diagnostic specimen, BAPGM enrichment prior to PCR has facilitated the detection of various Bartonella species in cerebrospinal fluid, joint fluid, aqueous fluid, and pathological effusions such as pleural, pericardial, and abdominal effusions.
Bartonella Prevalence in Humans
Mozayeni began working with patients with small vessel disease (SVD), relying on a careful subcortical neurological examination to find evidence of the disease in the nervous system Once he had a group of patients who met the criteria for SVD, he started testing this group for evidence of Bartonella infection.
Studies were done comparing 296 of Mozayeni’s patients (some with a prior diagnosis of Lyme disease); 192 high-risk patients with animal exposures or veterinarians with fatigue, joint pain, and arthritis; and 32 healthy medical school volunteers serving as controls.
Of the 32 controls, only 1 had positive Bartonella antibodies and none of the 32 had a positive test using the BAPGM platform The high risk patients had a seropositivity rate of 49%; whereas Mozayeni’s patients had a positive rate of 63% Using ePCR testing, 24% of the high risk group were positive; whereas 41% of Mozayeni’s patients had a positive test result which means that one or more Bartonella species were isolated or DNA of the bacteria was PCR amplified.3
Based on serological testing, blood donors have a Bartonella positivity rate of around 3.6%, veterinarians between 6% and-9%, and forestry workers between 10% and 40%. The Mozayeni patient population was higher than any of these groups. Importantly, serology may underestimate active infection with Bartonella in 50% and 75% of bacteremic individuals; therefore, serology has diagnostic limitations and the true prevalence of infection may be even higher than what is noted in these studies.
Bartonella and Lyme Disease
Bartonella has been described as a common c-infection found in people with Lyme disease Mozayeni hypothesizes that the reason some patients with Lyme disease do not improve with treatment is because the emphasis may often be put on the wrong infections. Practitioners may focus on Borrelia burgdorferi, the causative agent of Lyme disease, rather than Bartonella, Babesia, and various protozoa such as Protomyxzoa rheumatica.3 It may be these other microbial burdens that create the majority of the symptoms in what many refer to as “Lyme disease” rather than Borrelia itself.
“The paradigm in Lyme disease has been that one of the reasons the disease persists is because Borrelia has a complicated genome, is a smart organism that is very stealthy, has different forms, and evades the immune system,” said Mozayeni. He continued, “We are now entering a second way of thinking about it, a ‘Lyme 2.0.’ We are trying to understand the ecosystem and the microbiome of the different organisms that are involved.”
As common as Bartonella may be in those with Lyme disease, it can certainly exist on its own Many people with Bartonella alone may not express symptoms severe enough to be recognized and may be asymptomatic carriers. Over the long term, Mozayeni hypothesizes that carrying Bartonella chronically may cause a variety of common human diseases including arthritis, arteriosclerosis, and a host of other conditions. Bartonella is known to cause immune suppression in dogs and is immunosuppressive in humans, which may make people more prone to harbor other opportunistic microbial burdens and may fail to make antibodies to germs which might enable their serological detection.
Conventional Treatment Approaches
The most frequently used antimicrobial drugs for Bartonella are those that can enter the cell as the microbe is most commonly found intracellularly. While treatment is often successful in reducing symptoms, there are those where persistent infection has been identified “There is increasing evidence of treatment failures in people with normal immune systems, and it is not uncommon to see relapses in immunocompromised patients who were treated for six weeks or longer.”3
According to the Infectious Disease Society of America, erythromycin and doxycycline are drugs of choice with clarithromycin or azithromycin as alternatives For those with central nervous system disease, they suggest that the combination of doxycycline and rifampin may be the preferred treatment. They note that in immunocompromised patients with repeated relapses such as in those with HIV, treatment may need to be indefinite.3
Bartonella is susceptible to numerous antibiotics in vitro, but many of these have only bacteriostatic activity; they inhibit reproduction but are not bactericidal; they do not kill the bacteria. Gentamicin and, to a lesser extent, Rifampin have been found to be bactericidal.4 However, Gentamicin may only be bactericidal when the bacteria emerge from the red blood cells and are extracellular.
Based on a 2004 study, antibiotics which may be helpful in the treatment of Bartonella include doxycycline, erythromycin, rifampin, doxycycline with rifampin, doxycycline with gentamicin, gentamicin and ceftriaxone with or without doxycycline, chloramphenicol, ciprofloxacin, or streptomycin.41
The Lyme and Tick-Borne Diseases Research Center at Columbia University has recommended that azithromycin or doxycycline combined with rifampin, clarithromycin, or a fluoroquinolone may be useful regimens.42
Some practitioners have found drugs such as ciprofloxacin (Cipro), levofloxacin (Levaquin), gemifloxacin (Factive), and moxifloxacin (Avelox) to be helpful in those with Bartonella, though these drugs may lead to long-term tendon damage and ruptures, retinal detachment, and a host of other symptoms that may persist long after these medications have been stopped. They may result in what is known as fluoroquinolone toxicity syndrome, or what some term as having been “floxed.” Mozayeni has suggested that the risks of these medications may outweigh the benefits, and he rarely uses quinolone antibiotics for the treatment of Bartonella.
Mozayeni generally uses clarithromycin or azithromycin, though there is a higher resistance to azithromycin in animals. He later adds rifampin with clarithromycin. If a patient is on other medications whose metabolism may be impacted by rifampin, he may then use Mycobutin. He has not found a need to treat any of his Bartonella patients with IV therapies except in rare cases where patients cannot take pills. He has noted that antibiotics used for the treatment of Borrelia burgdorferi, the causative agent in Lyme disease, may push Bartonella organisms further into the cells making treatment more challenging.
Both adrenal health and thyroid health should be considered before treating with these antibiotics, especially rifampin, in order to allow the patient to better tolerate the treatment. Mozayeni has found that one pitfall in Bartonella treatment is related to adrenal fatigue. Adrenal issues must be identified and managed to optimize therapy tolerance. Rifampin, a cytochrome P450 inducer, causes a more rapid metabolism of sterol hormones and can lead to severe symptoms where a Herxheimer-like reaction is juxtaposed with a condition of depleted adrenals and low cortisol. This can put the patient into adrenal crisis with greatly amplified symptoms including severe pain and hemodynamic instability. This reaction may be mistaken for a Rifampin allergy and therapy stopped. Thus, withdrawal of a useful drug may result in a lost opportunity to treat and lead to treatment failure.
The pharmaceutical protocol that Mozayeni utilizes in his practice has been shown to work well for many of his patients. If someone is extremely ill and may not be strong enough to tolerate treatment with antibiotics, he may start with herbal antimicrobial and supportive interventions. It will take time and additional data to determine whether or not the herbal approaches prove to perform as well, but they are useful considerations. After an antibiotic regimen is complete, Mozayeni may then move a patient to more natural Bartonella treatment options. These may be more sustainable and can be used for longer-term maintenance therapy if needed.
Once someone is infected with Bartonella, it is possible that they will never fully clear the infection; it may become a matter of how the infection manifests within the body. Response to treatment of any regimen may vary based on the immune status of the host, the response of the immune system, and the infecting Bartonella species.
Alternative Treatment Approaches
While pharmaceutical options for Bartonella treatment are often very helpful, those with chronic Bartonella infection may benefit from looking at natural solutions. These may be combined with pharmaceutical options or used alone.
Mozayeni has an interest in allicin, an extract from garlic, and sulforaphane, a compound derived from cruciferous vegetables. Sulforaphane has broad spectrum antimicrobial properties against both gram-negative and gram-positive bacteria while also being anti-inflammatory, supporting detoxification, and serving as a powerful antioxidant.
Stephen Harrod Buhner is a one of America’s preeminent herbalists and wrote Healing Lyme Disease Coinfections: Complementary and Holistic Treatments for Bartonella and Mycoplasma in 2013.43 It contains some of the most current information on herbal and holistic treatment of Bartonella. In the book, Buhner goes into extensive detail on Bartonella characteristics, symptom presentation, cytokine shifts that may occur, and natural treatment options based on his own clinical experience and literature reviews.
Buhner has created a protocol that is outlined in his book and consists of therapeutic options such as Sida acuta, Isatis, Houttuynia, Alchornea cordifolia, Japanese knotweed, EGCG, hawthorn, cordyceps, L-arginine, milk thistle, and others. He further outlines interventions that may be helpful based on specific symptom presentations. The book is a very detailed resource on Bartonella and is highly recommended for anyone who wants to learn more.
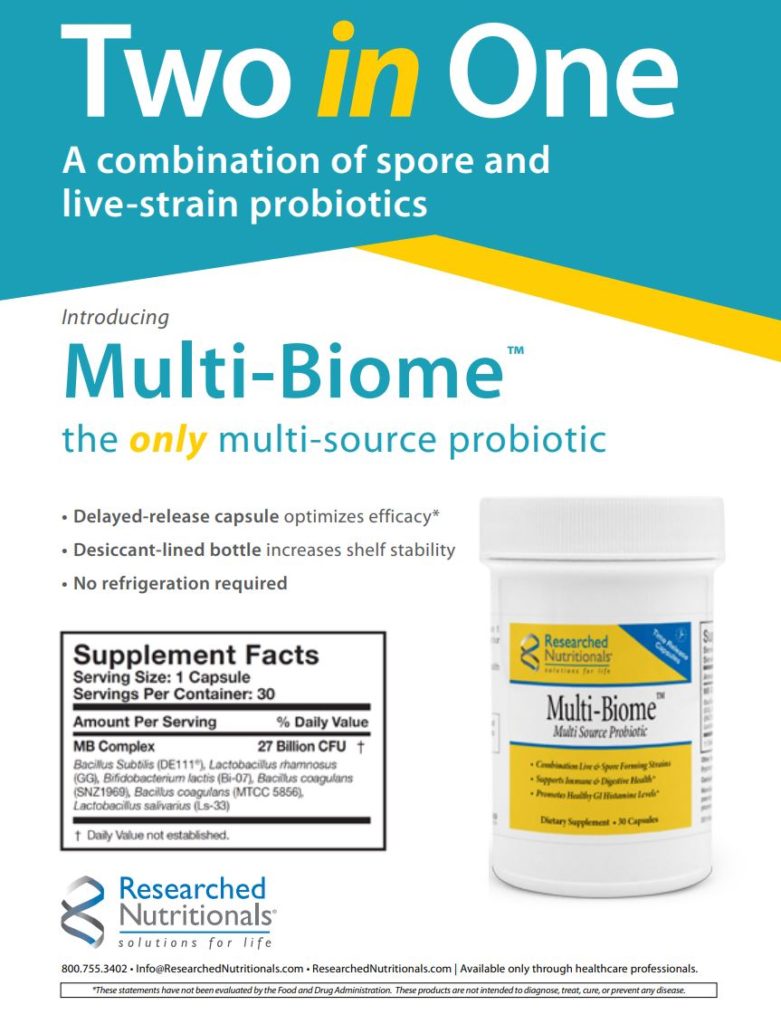
Many other natural products or formulations are available that some practitioners have found helpful. These include Beyond Balance MC-BAR-1 and MC-BAR-2; BioPure Quintessence, O3 Oil Gamma, Lyme and Co-Infection Nosode Drops, Cryptolepis, and Czaga (chaga); Byron White Formulas A-BART; Maypa Herbals Formula Bart; Jernigan Nutraceuticals Lymogen, NutraMedix Samento, Banderol, Quina, Cumanda, and Houttuynia; Researched Nutritionals BLt Microbial Balancer #1, CryptoPlus Microbial Balancer #2, and LymPlus Transfer Factor; Deseret Biologicals Bartonella Series Therapy; Woodland Essence C.S.A. Formula; Mountain States Health Products Bartonella Nosode; Professional Formulas Tick Pathogen Nosode Drops; Dr. Zhang’s HH and HH-2; freeze-dried garlic, and others. Injectable artesunate administered by a doctor has been found to be of clinical benefit. Some practitioners have found essential oils of clove, thyme, marjoram, melaleuca, cypress, rosemary, and cinnamon to be helpful.
Recently, at the American Academy of Environmental Medicine workshop, low-dose antigen (LDA) therapy for Lyme disease was introduced by Ty R. Vincent, MD, and has reportedly been helpful for those dealing with Bartonella and other Lyme-related issues.
Synergistic Treatment Options
While the underlying microbial burden itself must be addressed, there are a number of synergistic interventions that may improve patient outcomes. Mozayeni has noted that the most proximal cause of symptoms of Bartonella is the small vessel disease, and addressing this aspect of the condition is an important part of the treatment program. Two primary areas of focus include evaluating and treating coagulopathies and reducing inflammation.
Small vessel disease results in a form of brain injury, though the injury does not have to be permanent. Treatment must be approached in a manner very similar to how a brain injury would be treated. The nerves may be stunned or hibernating as a result of trauma; these may be resuscitated with glutathione, hyperbaric oxygen, or other interventions.
Bartonella often causes low grade inflammation in the body. This can manifest in more significant ways, such as inflammatory arthritis or a neurovascular problem, in people with specific MHC (major histocompatibility complex) or HLA (human leukocyte antigen) genetic predispositions. The infection may result in chronic, low-grade, smoldering symptoms even in those that considered themselves to be asymptomatic. How the disease manifests is determined by the biological terrain and how the host immune system responds to the infection and less by the infection itself.
For hypercoagulation, agents that dissolve clots or help to reduce clot formation may be helpful. The more the blood pH is acidic, the more coagulation is likely to be a concern. Substances that alkalinize the body help to reduce microscopic clot formation. High dose vitamin C, apple cider vinegar, and an alkaline diet are useful tools. Incorporating fresh vegetables into the diet both helps alkalinize the system and introduces enzymes that help to break down clots and biofilms (a polysaccharide layer produced by a community of organisms that serves to protect them from antimicrobial therapies).
Boluoke, lumbrokinase, or serrapeptase are commonly considered, as are Wobenzym and Researched Nutritionals InflaQuell. When patients are not improving with or tolerating treatment, Mozayeni’s first question is often whether they are keeping up with their enzyme intake; he finds that 80% to 90% of the time they are not. During a Herxheimer reaction, enzymes and alkalinization can often provide relief. If neurological symptoms are severe, low-dose Lovenox or heparin may be considered and often leads to dramatic improvement.
Reducing inflammation using natural options such as curcumin, quercetin, and astaxanthin may be very helpful.
Treatment may include a focus on the health of the lining of the endothelium where Bartonella congregate.
Nitric oxide is produced in the endothelium and may be impaired when the endothelium is unhealthy. Thus, therapies such as Xymogen AngiNOX, Thorne Perfusia Plus, or L-arginine, which increase nitric oxide production, may support blood vessel health. Increasing nitric oxide production may counteract some of the detrimental effects of Bartonella.44 Low-dose baby aspirin may reduce the stickiness of the platelets.
In Chinese medicine, the herb Dan Shen (Salvia miltiorrhiza) is a “blood-invigorating” herb that is thought to make the blood flow more freely and has angiotensin-blocking properties. Vinpocetine is derived from the periwinkle plant and leads to dilation of blood vessels and improved blood flow. Hawthorn berry, in a form called Cratoxy, may support cardiovascular health and dilate the blood vessels. As a blood vessel dilator and platelet inhibitor, Ginkgo biloba may be beneficial.
Prevention and Management of Pet Exposure
In Bartonella patients with pets in the home, consideration should be given to the potential for reexposure from the pet or from fleas or ticks that these animals may bring into the home. Cats represent a higher risk for human exposure, though dogs may present with more symptoms when infected. Anyone infected with Bartonella and living with household animals should consider having their animals evaluated and treated for the infection in order to minimize the potential for reinfection. Veterinarians are generally well versed in testing and treatment of animals with Bartonella. Most importantly, keeping fleas and other vectors from infesting pets will reduce and potentially eliminate the possibility of transmission from a pet to a family member.45
Conclusion
While more and more is being learned about Bartonella and its impact on human health, there are still many unknowns that require further exploration. We are learning and will continue to learn. Very few medical doctors are familiar with Bartonella and people suffer needlessly, as bartonellosis is rarely on the list of differential diagnoses for the conditions that it may cause. Most infectious-disease doctors have very limited or no experience with identifying or treating Bartonella and believe that it is generally a benign condition that resolves without treatment.
Thanks to our animal friends and those who care for them, there is an ever-increasing focus on Bartonella and human health implications. The work of Drs. Ed Breitschwerdt and Robert Mozayeni has enlightened many about this previously underestimated microbe and continues to lead to improved testing and treatment options for both animals and humans. While getting people to recognize Bartonella has been a struggle, the tide is shifting.
Available tests have notably improved over the past several years, and treatment options are available that generally lead patients to higher ground. While there is more work to be done, the mysteries of Bartonella are beginning to unravel. Here’s to your health!
In Memoriam
Linda “Angel” Heming worked closely with me for many years on a number of the articles that I have written. She was a warrior in the Lyme community and gave so much of herself to help other people. Given the time commitment required for each article, I was unable to do as many as I once did. A year ago, Linda asked me whom she could get who would interest me enough to do another article. At that time, I responded that an article on Bartonella with Drs. Ed Breitschwerdt and Robert Mozayeni would be compelling. Linda unfortunately became ill with another battle with cancer and passed away in October 2014. It was a great loss to the Lyme community. About a week after she passed, I was connected with a colleague of Drs. Breitschwerdt and Mozayeni, and an opportunity to do this article presented itself. Of course, I couldn’t say no, as it was clear to me that Linda was still running the show. You will be missed and truly are an angel!
Scott Forsgren is a health writer, advocate, and coach. He is the editor and founder of BetterHealthGuy.com, where he shares his now 18-year journey through the world of Lyme disease and the myriad of factors that it often entails. He has been fortunate to have written for publications such as the Public Health Alert, Explore!, Bolen Report, and Townsend Letter. Scott was personally affected by Bartonella for many years and today enjoys a state of good health. More information on his work is available at http://www.BetterHealthGuy.com.
Dr. B. Robert Mozayeni is an expert in translational medicine, the science and art of advancing medical science safely and efficiently. He is the chief medical officer of Galaxy Diagnostics. He specializes in autoimmune diseases and the effects of chronic infection and inflammation on vascular physiology and neurovascular conditions commonly seen with autoimmune and neurovascular diseases. He has a clinical practice in Rockville, Maryland. I thank him for his time in participating in this article and sharing his experience with the treatment of Bartonella. For more information, visit http://tmgmd.com.
Disclaimer
Information is not intended to treat, diagnose, cure, or prevent any disease. Nothing in this text is intended to serve as personal medical advice. All medical decisions should be made only with the guidance of your own medical authority.
Portions of the information presented in this article come from various conferences as well as an interview with Dr. Robert Mozayeni for the purposes of this article.