|
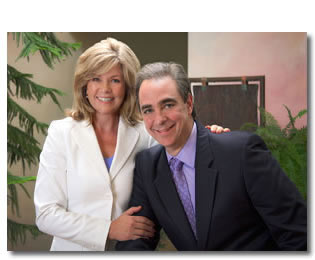
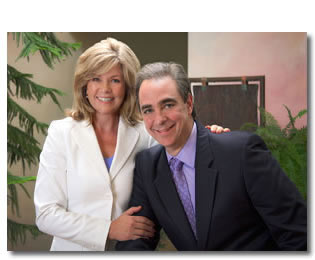 Drs. Steve and Sandi Amoils have traveled the world looking for the best of alternative medicine. Originally from South Africa, they met in medical school and found that they both had a deep interest in the nature of healing. As a teenager, Steve had been a highly-ranked competitive swimmer when he developed severe chronic fatigue. Despite the best medical advice and care, his condition did not improve until he met an acupuncturist who was able to help him regain his health. Subsequently he was able to successfully complete both college and medical school. Despite the significant stress and reduced sleep schedule in his later role as a physician, the fatigue never returned. Drs. Steve and Sandi Amoils have traveled the world looking for the best of alternative medicine. Originally from South Africa, they met in medical school and found that they both had a deep interest in the nature of healing. As a teenager, Steve had been a highly-ranked competitive swimmer when he developed severe chronic fatigue. Despite the best medical advice and care, his condition did not improve until he met an acupuncturist who was able to help him regain his health. Subsequently he was able to successfully complete both college and medical school. Despite the significant stress and reduced sleep schedule in his later role as a physician, the fatigue never returned.
As a result of these experiences, Steve came to question what constitutes true healing and when he met Sandi, he found that she also had a deep sense of inquiry about health and medicine. This led them on a quest of sorts, traveling the globe for two years after medical school, living and working in different cultures, observing how illness was treated. They visited African medicine men, Philippine psychic surgeons, and herbalists worldwide, and subsequently apprenticed with an acupuncturist in Japan. The following year while working in London as physicians, they traveled Britain and Europe observing the healing modalities that the Europeans were using. This search for healing has continued. Today they are fascinated with how modern modalities such as genomics, nanotechnology, and computer technology are applied in health services and healing.
These experiences have deepened their understanding of complementary therapies and continue to inform and enrich how they practice medicine. While they came to believe that there was no such thing as the magic bullet, they began to see synergy between various therapies and realized that these treatments could be combined in new ways to maximize benefit to the patient. The challenge was to determine which therapies provide the greatest synergistic effect and how to integrate that benefit to achieve a quantum shift in the health of their patients.
In 1999, they opened the Alliance Institute for Integrative Medicine (AIIM) in Cincinnati at the request of the CEO of the Health Alliance, a consortium of hospitals, physicians, and specialists. In 2004 their center was chosen by the Bravewell Collaborative as one of the leading clinical integrative medicine centers in the country. Since then they have collaborated with other centers in advancing the field of integrative medicine by sharing information and participating in clinical trials. The Amoils took their center private in 2007 and now oversee approximately 25,000 patient visits a year.
Autoimmune Conditions
Nancy: I know you have an exceptional approach to the diagnosis and treatment of pain. Tell us about how you work with autoimmune patients.
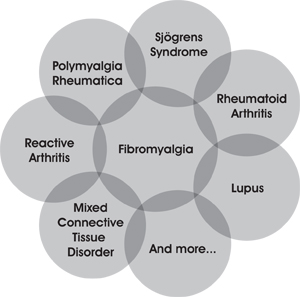
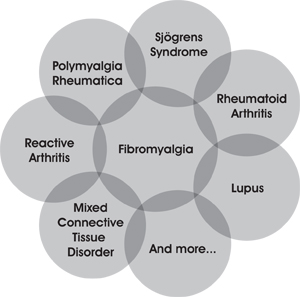
Steve Amoils, MD: With autoimmune diseases, much of the pain that we see is driven by both arthralgia and fibromyalgia. When we speak of fibromyalgia we are talking about fatigue with generalized aches and pains. We've found that if we can treat those two conditions, often we can effect real change. Viewing pain across a spectrum, if we think in terms of a Venn diagram, in the middle of the diagram is fibromyalgia driving all the other symptom patterns.
We target these conditions through a five-pronged approach: 1) expanded conventional medical options, 2) stress and neurotransmitter assessment and treatment, 3) nutritional, metabolic, and immune status evaluation and treatment, 4) functional hormonal evaluation and treatment, and 5) structural and bioenergetic balance assessment and treatment.
Venn Diagram
Nancy: How do you assess these patients to get a really clear picture of what they need?
Steve: There are two different vantage points. One approach is to assess these five areas, see which one is likely to give the highest yield, and then start with a therapeutic trial of a medication, supplement or a treatment modality. When I see a patient with pain and depression, I might utilize a treatment modality such as acupuncture or massage. I would also recommend that patient an antidepressant like Cymbalta (which targets both pain and depression) or I might recommend some supplements that will do the same thing. I then watch for the degree to which their pain improves. If I think that their problem is inflammatory in nature, then I may give them an anti-inflammatory medication or supplement. If it's myofascial, I may try acupuncture first, and see if we can get the trigger points to calm down. The other approach is to provide an in-depth evaluation of each of the five prongs, and then come up with a personalized plan. The patient is always at the center of this conversation. We need to take into account their needs and desires.
Sandi: We are constantly assessing what is best for the patient. Do we need more of one thing, or a combination of everything? We need to factor in cost, the time they have available, the length of time they have been ill, their support systems, and a host of other factors.
Nancy: So in a way I'm hearing a step-by-step assessment similar to the approach you use to treat chronic pain, but it's broader. What else about your approach do you feel is important?
Steve: At this point, integrative medicine is an all-inclusive term for a field that tends to be highly variable. The providers that do stress reduction are not necessarily doing body work. The body workers are not usually doing functional medicine. The functional medicine people are usually focusing primarily on biochemistry and nutrition. Few providers are integrating all of these approaches. That is why we continue to work on developing a model that provides all these therapeutics in-house at one location.
Sandi: We always use a functional medicine systems- approach when dealing with autoimmune issues. We address nutritional factors, oxidative stress, inflammation and detoxification issues. We can try a therapeutic intervention and observe how the patient reacts, or utilize a functional lab workup to better evaluate what he or she needs. Testing in this area is becoming much more sophisticated. If we know for instance that someone has an IL-6 or TNF-a SNP, we may want to utilize supplements or lifestyle changes that inhibit the expression of these genes. We are constantly working with diet and nutrition, and will assess gut hyperpermeability and the gut microbiome when possible. We always address stress and psychological issues since these compound immune imbalances. The goal is to find a way to modulate the patient's immune system, to downregulate it.
Pain Disorders
Nancy: Do the majority of your patients have pain conditions, and how do you manage to see so many patients?
Steve: At least 70% of our patients have pain. They may not have pain as their primary issue, but 70% to 80% experience some degree of pain. We are able to serve more people because we use an integrative team-based model that includes a physician-acupuncturist on every team, so patients can be medically assessed and then treated with an integrative approach simultaneously.
Nancy: How long does it typically take to resolve chronic pain – these problems tend to be so individual and so complex.
Steve: The rule of thumb we give to patients is 50% reduction in their pain in four treatments. That's what we're aiming for.
Sandi: We cannot help everyone; we do struggle with some patients. In terms of how we see so many patients, we have many different therapists working under one roof. Everyone sees individual patients and they also work together on some of the treatments.
We recently participated in the SIMTAP study, practice-based research involving nine centers across the country. This study, sponsored by the Bravewell Collaboration, documented various therapeutic approaches to the treatment of chronic pain using integrative medicine. Patients on average had experienced chronic pain for more than eight years. Those who enrolled were 81% white, 73% female, with an average age of 49. Each center enrolled approximately 50 patients, provided treatment, and then followed them over a period of six months. We used standardized questionnaires that the patients answered, looking at depression scores, quality of life, etc. The study also included lab work documenting hs-CRP and vitamin D levels for all patients, pre- and post-study.
The outcomes overall were quite remarkable. On average there was a significant reduction in pain and in the level and frequency of depression, as well as improvement in quality of life. When the data were run for each individual center, on average the patients seen at our clinic had a 50% reduction in pain.
Nancy: Amazing – 50% reduction in six months is an astonishing outcome!
Sandi: For this study, each center had their own "black box" approach to chronic pain. Practitioners utilized the modalities and proprietary protocol of the center where they practiced. In our approach, individual patients are seen by both physicians and therapists. We have chiropractors, Rolfers®, and massage therapists, as well as nurses who do energy healing. We also provide stress reduction classes, and we have a nutritionist who works with people on their diets.
Our signature treatment for pain is a series of combination therapy sessions, which we refer to as an ACE session, consisting of acupuncture, chiropractic, and energy work. In a single visit patients are assessed and treated using all three modalities. Initially they are seen by a chiropractor. Then a physician sees the patient (all our physicians are acupuncturists) so the doctor provides an acupuncture treatment, and addresses any medical aspects of care that may need to be discussed whether that involves supplements, testing, or other issues. Once the acupuncture needles are in place, a nurse provides energy healing to deepen the treatment. The entire treatment takes about an hour, and almost always, patients leave feeling deeply restored.
We may also use frequency specific microcurrent provided by a chiropractor or one of the physician acupuncturists. We have a physician who provides prolotherapy for patients with joint pain. For each particular patient, our goal is to identify the special combination of therapies that will be most effective. As a team, we tend to have good communication – we refer to one another and confer with each other about the patients. If we are not resolving their pain, then we know we have to make changes in what we're doing or explore other treatment options. This is a very real-time focus on clinical effectiveness, and we tend to work quite well with one another using this process. Our goal is to create a cohesive team of providers who understand what everyone on the team is doing.
Steve: Another key to our pain treatment is that we are very attuned to the effects of chronic stress on chronic health issues. We make it a point to address stress disorders very thoroughly, using an in-depth systemic approach we've developed from a functional medicine model.
Sandi: For us everything depends on what our patients want. We offer a range of options from CDs and different classes to one-on-one health coaching. We refer out if needed, and we also have classes here. In terms of stress reduction, often just acupuncture or massage therapy is highly stress reducing. We have a Duke-trained integrative health coach, as well as very impressive naturopath who works hand-in-hand with our physicians. Understanding the benefit of Functional Medicine really brought our model to new level and expanded the types of health issues we are able to address. We have had very encouraging outcomes with chronic pain beyond our initial expertise in biomechanical and acupuncture pain management. For example, one woman who suffered from a twenty-year history of chronic headaches had them resolve overnight with the correct amino-acid supplementation, while another woman with a similar clinical picture had a fatty acid deficiency that was resolved with a fish oil supplement.
Nancy: Sounds like you are always watching for that tipping point, staying attuned to which therapy is going to make the difference. That is a very Zen approach – to be that present and that dialed in to what is going to create change.
Steve: We've observed that pain does not improve in a linear fashion. It is like a pendulum: you have to nudge the patient toward normal. Then they revert back to their earlier set point. At that stage, you have to nudge them again, and you must continue to periodically nudge the body toward a feeling of optimal health, getting them accustomed to the experience of being pain-free. That is a back and forth process, and the art is to be able to nudge the body when you need to. Initially, patients with pain come in for treatment once a week. Over time, we wean them off the therapy. After that, they tend to come in once every two weeks, then every three weeks, eventually every month, and then every six weeks. Despite their progress, they often find that they start to develop some mild aches and pains, and that's why it is important to continue to see them periodically.
It is also important to put control back in the hands of the patient, in terms of when and how to reduce their pain. This can be extremely effective. Once they realize that X therapy is reducing their pain by Y amount, then they will tell you, "I need a treatment here," or "I need to see you this often." You're transferring the locus of control from the doctor to the patient, which is something we really appreciate.
We hold ourselves to a very high standard. If the patient keeps coming back saying, "My pain is no better," we need to adjust what we are doing. Periodically we have to cease treatment because we are not seeing improvement. We don't want to waste our patients' time or money. We are exceptionally honest about that. When we ask patients in a month's time whether they are better, if their answer is, "Maybe." or "Possibly." or "A little bit." that's not better. Better is when they come in and say, "Wow, I feel fantastic! I've got my life back."
Assessing our patients' readiness for change is another important piece of this. Our goal is to help our patients make vital changes – to help them transform their lives, experience more happiness, less pain, and fewer overall health problems. To achieve that, they need to be ready for change. Typically people need different things at different points in their lives. Some patients just want periodic symptom reduction, while others want an entire lifestyle transformation. We are there to partner with them in their decision making, but only they can decide how and when they are going to implement the resources that we can provide them. The key is understanding their readiness for change and giving them an approach they can handle. That is the basis for a powerful and personalized approach that is simultaneously pro-active and preventive as well.
Click to view chart: Multidimensional Diagnosis for Chronic Pain Conditions
Stress and Neurotransmitter Assessment and Treatment
The patient's adaptive stage of stress is evaluated. Diurnal salivary cortisol levels, salivary DHEA, and urinary neurotransmitter levels are evaluated. Patients are divided into various stages of stress:
a. The Exhilaration Phase: Patient unlikely to seek treatment in this stage. Testing results tend to be variable.
b. Wired and Tired Phase: Cortisol generally drops in the morning ("tired") and increases at night ("wired"). Glutamate, epinephrine and norepinephrine may be elevated. Serotonin and GABA may be increased.
c. Exhausted Phase: Cortisol is generally decreased throughout the day. DHEA levels are generally lower. Epinephrine, norepinephrine, serotonin and GABA may be decreased.
d. Exhausted and Inflamed Phase: Results are similar to the exhausted phase, but pro-inflammatory cytokines are elevated, while anti-inflammatory cytokines decrease. Insulin resistance increases.
e. Overwhelmed and Depleted Phase: Cortisol diurnal rhythms are lost. Cortisol levels are low.
Epinephrine, norepinephrine, serotonin, and GABA levels are generally low. Patients are usually clinically depressed. Autonomic testing reveals autonomic dysfunction including neurally mediated hypotension and reduced heart rate variability
Treatment options include acupuncture or massage to reduce stress, behavioral approaches such as health coaching or stress management classes, exercise programs such as yoga, tai chi or chi gong, supplements including stress adaptogens, and/or medications. |
Steve Amoils, MD, and Sandi Amoils, MD
Steve and Sandi Amoils are the founders and Medical Directors of the Alliance Institute for Integrative Medicine (AIIM) in Cincinnati. Board-certified in family medicine, they also serve as Adjunct Assistant Professors in the Department of Medical Education at the University of Cincinnati. Sandi is the president-elect of the American Academy of Medical Acupuncture (AAMA), while Steve serves as president of the Ohio Chapter of the AAMA. Both act as co-Principal Investigators for ongoing research with the Bravenet Practice Based Research Network.
After completing medical training in South Africa, they spent two years traveling the world, seeking out and studying healers in indigenous medical systems. They later immigrated to the U.S. in 1988, completed family practice residency programs at the University of Cincinnati, and subsequently studied medical acupuncture with Dr. Joseph Helms at UCLA, and functional medicine with the Institute for Functional Medicine. Together with their team of physicians and therapists, the Amoils have been offering a comprehensive integrative approach through their center, the Alliance Institute for Integrative Medicine, since 1999, pioneering what they term Transformational MedicineTM. In 2008, they formed the non-profit Integrative Medicine Foundation (www.IntegrativeMedFoundation.org) with the goal of educating both physicians and the public on the benefits of Integrative Medicine, performing research, and serving the underserved utilizing Integrative Medicine.
Contact
Alliance Institute for Integrative Medicine
6400 East Galbraith Road
Cincinnati, Ohio 45236
513-399-6305
Fax: 513-791-5526
Website: www.MyHealingPartner.com
Resource
Written by Drs. Steve and Sandi Amoils, Get Well, Stay Well: Optimal Health through Transformational Medicine is a user-friendly guide that explains many of the basic concepts of functional medicine in a way that patients can understand and apply. The book opens with an insightful look at the interplay between chronic stress and chronic illness to help readers begin retracing their steps back toward health. Building on this foundation, the nutrition section emphasizes low-stress eating, including concepts such as glycemic load, genetic expression, and sustainable weight loss, as well as optimal digestive health and detoxification. Hormone chapters cover the interaction between stress, cortisol, and sex hormones, as well as topics such as PCOS, hormone testing, and supplementation. The chapters on pain alone are worth the price of the book and provide in-depth information on the perspective reviewed in this article. This work is a must-have that integrative providers will want to make available to their patients.
Interview and Editorial
Nancy Faass, MSW, MPH, is a writer and editor in San Francisco who has worked on more than 40 books for publishers that include Elsevier, Harper, McGraw-Hill, Mosby, New Harbinger, New World Library, North Atlantic, and other presses. Director of The Writers' Group, her work also includes articles, white papers, and writing for the web. For more information see www.HealthWritersGroup.com.
|
![]()
![]()
![]()





 Drs. Steve and Sandi Amoils have traveled the world looking for the best of alternative medicine. Originally from South Africa, they met in medical school and found that they both had a deep interest in the nature of healing. As a teenager, Steve had been a highly-ranked competitive swimmer when he developed severe chronic fatigue. Despite the best medical advice and care, his condition did not improve until he met an acupuncturist who was able to help him regain his health. Subsequently he was able to successfully complete both college and medical school. Despite the significant stress and reduced sleep schedule in his later role as a physician, the fatigue never returned.
Drs. Steve and Sandi Amoils have traveled the world looking for the best of alternative medicine. Originally from South Africa, they met in medical school and found that they both had a deep interest in the nature of healing. As a teenager, Steve had been a highly-ranked competitive swimmer when he developed severe chronic fatigue. Despite the best medical advice and care, his condition did not improve until he met an acupuncturist who was able to help him regain his health. Subsequently he was able to successfully complete both college and medical school. Despite the significant stress and reduced sleep schedule in his later role as a physician, the fatigue never returned.