

July 2003
Current Recommended Safe Levels of Vitamin A Intake
Do Not Cause Increased Fracture Rate
by Dennis Meiss, PhD and Elmer Cranton, MD
Abstract
Although recent reports suggest a potential link between excess vitamin A levels
and risk of fracture, detailed analysis of the data shows that fracture rates
increase only among individuals consuming more than the current recommended
upper level of safe intake of 3,000 RE (10,000 I.U.) established by the Institute
of Medicine. The level at which the rate increases is unclear but does not
occur until daily intake exceeds 10,000 I.U. Vitamin A antagonizes vitamin
D metabolism. Vitamin D deficiency can be potentiated by higher intakes of
vitamin A. This alternative explanation is supported by significantly greater
fracture incidence in Sweden, where sunshine is less prevalent and endogenous
vitamin D production is reduced and vitamin A intake is probably considerably
above 10,000 I.U. Changes to current recommendations for safe daily intake
of vitamin A are not justified at this time. A statistical correlation, if
it exists, is never by itself evidence for cause and effect.
Background
Recent studies suggest that high vitamin A intake in women1 and serum retinol
levels in men2may correlate with an increased risk of osteoporosis and non-traumatic
fracture. These independent studies conclude that the rationale for vitamin
A supplementation and food fortification may need to be reassessed but more
data is needed before a scientific consensus can be established. Unfortunately,
the public media misinterpreted these studies to conclude that the current
upper safe level of intake established by the Institute of Medicine at 10,000
I.U. per day is placing a significant proportion of the adult population
at risk. The media has gone so far as to deceptively report that there may
be significant risk at levels as low as 5,000 I.U. per day. Closer examination
of the data shows these media conclusions are unjustified.
The Harvard Nurses Health Study: Vitamin A Intake
The Harvard Nurses Health Study1 analyzed the relationship between dietary
intake of preformed vitamin A (retinol) from food and supplements and hip
fracture rates in 72,337 postmenopausal women followed for 18 years. Women
were divided into five equal groups (quintiles) ranging from the lowest consumption
of vitamin A (<4,167 I.U.) to the highest (>10,000 I.U.) The relative
risk of fracture correlated with only the highest levels of vitamin A intake,
indicating a 48% increased relative risk of hip fracture in those women consuming
more than 10,000 I.U. per day. That correlation was not associated with beta-carotene
intake.
While the authors report a correct index of relative risk, one gets a different
perspective when the actual incidence of fracture is evaluated (see Table 1).
Fracture incidence from the Harvard
Nurses Health Study
Table 1
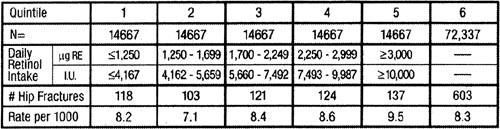
The number of hip fractures within the lowest quintile of vitamin
A intake over the 18-year span was 118 out of 14,667 or about 8 out
of every 1,000 women. Contrasting this with the highest quintile, 137
hip fractures occurred or about 10 out of every 1,000. Interestingly,
those in the second quintile had the lowest number of fractures while
the third and fourth quintiles had similar numbers of fractures (about
8 to 9 for every 1,000) compared to the first quintile. No significant
correlation with fracture risk occurs until currently recommended safe
levels of 10,000 I.U. daily are exceeded.
The data thus shows that dietary intake of less than 10,000 I.U. vitamin A
daily does not correlate with a statistically significant increase in incidence
of fracture. A potentially significant correlation is seen only among women
in the highest quintile. Unfortunately, the range of dietary intake in this
quintile was not reported. The increased risk of fracture can be skewed by
a few women whose vitamin A intake was greatly in excess of the 10,000 I.U.
cutoff. Women in the highest quintile are likely to be more affluent and consume
higher levels of supplemental vitamin A in addition to multiple supplements.
Without that data, the amount of vitamin A at which fracture incidence increases
significantly is unknown. Although actual doses consumed by those in the highest
quintile cannot be determined from the data, it can reasonably be assumed to
have been much greater than 10,000 I.U. daily.
The Swedish Men’s Study: Serum Retinol
Levels
The relationship between serum retinol levels and fracture rate was evaluated
in a population of Swedish men, 49 to 51 years of age at enrollment and followed
for 30 years.2 The study, involving 2,322 men, indicated that the risk of
fracture correlated directly with serum retinol levels. Men in the highest
quintile for serum retinol displayed a relative risk of 1.64 for any fracture
and 2.47 for hip fracture as compared with men in the middle quintile. Among
men with serum retinol levels in the 99th percentile (>103.12 µg
per dl or 3.60 µmol per liter), the increased risk of fracture was
approximately 7 times higher compared to men in the lower levels. Serum beta-carotene
levels had no association with relative risk.
Again, an alternative perspective is seen based upon the actual incidence rate
(see Table 2). While the first quintile with the lowest serum retinol levels
had fewer hip fractures compared to the fifth quintile with the highest serum
retinol levels (41 for every 1,000 versus 54 per 1,000), the middle quintiles
had a much lower incidence compared to the first quintile (24.6 vs 41.3).
Fracture incidence from the Swedish Men's Study
Table 2
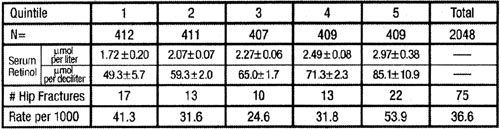
Analysis of the published method casts doubt on the reported association
between serum retinol and risk of fracture. Blood levels of retinol
were measured only once at the beginning of the study and the participant’s
reports of diet and supplement use 20 years later did not correlate
closely with their initial serum vitamin A levels. While this study
gives cause for some concern, other studies are contradictory, adding
support for alternative conclusions.
It is especially relevant to point out that the overall incidence of fracture
in the Swedish study was more than three times higher than that seen in the
Nurses Study. This suggests that factors other than vitamin A levels are contributing
to the rate of fracture.
General Comments
Because the two independent studies cited here were so large and the number
of fractures relatively small in proportion, minor increases in incidence
among the quintiles resulted in statistically significant correlations. However,
it is questionable whether these differences are clinically meaningful given
the similarity in fracture rates for all but the highest quintile. The data
suggests that there is an upper level of safe intake within the highest quintile
but offers no insight into what that level may be.
Vitamin A is metabolically antagonistic to vitamin D, affecting both intestinal
absorption and bone formation.4,5 Increased consumption of vitamin A - from
dietary sources, food fortification, and nutritional supplements - without
adequate vitamin D will therefore adversely affect calcium metabolism and bone
formation. Foods are routinely fortified with fully formed retinol, but not
with vitamin D. Instead, a synthetic vitamin D analog, activated ergosterol,
is commonly used. That is also true of many inferior vitamin supplements. Rich
sources of natural vitamin D are only found in fish liver oils and livers of
animals fed on fish. The only other significant natural source of vitamin D
is from exposure to sunlight. Unless individuals get enough sunshine on bare
skin and consume adequate amounts of vitamin D, a deficiency may occur, especially
in winter months in northern climates or if housebound. This may explain in
part the much higher overall incidence of fracture in the Swedish Men’s
Study. Additionally, the use of sunscreens can prevent vitamin D absorption
and increase vitamin D requirements.6 Vitamin D deficiency is common in the
elderly and appears to be on the rise.7-9 Vitamin D combined with calcium effectively
reduces bone loss and fractures, and improves bone mineral density.10
Vitamin D deficiency, potentiated by otherwise safe levels of vitamin A intake,
offers a more plausible explanation for any potential correlation between high
vitamin A intake and fracture risk. Antagonism between vitamins A and D can
be avoided by administering the two together in their natural and metabolically
active forms. That is how high-quality professional supplements should be formulated.
Bone growth and maintenance are under complex hormonal control (thyroid, vitamins
A and D, cortisol, testosterone, estrogen, and progesterone) and are dependent
upon the levels of many nutrients including calcium, magnesium, zinc, phosphorus,
and vitamin K. Additionally, lifestyle choices such as smoking, physical activity,
sugar intake, and exposure to sun also contribute to overall bone health. The
studies reported here do not support a strong cause and effect relationship
between vitamin A and fracture risk at levels consistent with current dietary
recommendations.
![]()
Conclusions
Although excessive levels of vitamin A may exert an adverse effect on bone
metabolism, the two studies cited here bear closer examination before concluding
whether current recommended safe levels of intake raise the risk of osteoporosis
and fracture. The lack of randomization or blinding in the methodology employed
in both studies means that the results must be treated with some caution.
The data suggests circumstantial support for a possible link between vitamin
A intake and fracture risk. However, direct evidence of cause and effect
with reduction in fracture risk must be confirmed under more rigid controlled
levels of vitamin A intake accompanied by adequate vitamin D.
These recent studies should not be used to change public policy on vitamin
A limit. They must be evaluated within the totality of credible science on
vitamin A safety. Thorough review of the available scientific evidence by the
Institute of Medicine resulted in a consensus position on a safe upper limit
of 10,000 IU per day.3 We agree that continuing research is needed to gain
a clearer understanding of what constitutes a safe level of intake for vitamin
A for the general public. However, we do not see convincing evidence that current
levels of long-term intake up to 10,000 IU daily are unsafe.
![]()
Correspondence:
Dennis Meiss, PhD
ProThera®, Inc.
4133 Mohr Avenue, Suite I
Pleasanton, California 94566 USA
925-484-5636
dennis.meiss@protherainc.com
![]()
References
1. Feskanich D, Singh V, Willett WC, Colditz GA. Vitamin A intake and
hip fractures among postmenopausal women. JAMA 2002;287:47-54.
2. Michaëlsson K, Lithell H, Vessby B, Melhus H. Serum retinol
levels and risk of fracture. N Engl J Med 2003;348;287-94.
3. Food and Nutrition Board, Institute of Medicine. Dietary Reference
Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper,
Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and
Zinc. Washington, DC: National Academy Press, 2001.
4. Rohde CM, Manatt M, Clagett-Dame M, DeLuca HF. Vitamin A antagonizes
the action of vitamin D in rats. J Nutr 1999;129(12):2246-2250.
5. Johanson S, Melhus H. Vitamin A antagonizes calcium response to
vitamin D in man. J Bone Mineral Res 2001;16(10):1899-1905.
6. Fuller KE, Casparian JM. Vitamin D: balancing cutaneous and systemic
considerations. South Med J. 200194(1):58-64.
7. Rao DS. Perspective on assessment of vitamin D nutrition. J Clin
Densitom 1999;2(4):457-64.
8. Thomas MK, Lloyd-Jones DM, Thadhani RI, Shaw AC, Deraska DJ, Kitch
BT, Vamvakas EC, Dick IM, Prince RL, Finkelstein JS. Hypovitaminosis
D in medical in-patients. N Engl J Med 1998;338(12):777-83.
9. LeBoff MS, Kohlmeier L, Hurwitz S, Franklin J, Wright J, Glowacki
J. Occult vitamin D deficiency in postmenopausal US women with acute
hip fracture. JAMA 1999;28;281(16):1505-11.
10. O'Brien KO. Combined calcium and vitamin D supplementation reduces
bone loss and fracture incidence in older men and women. Nutr Rev 1998
May;56(5 Pt 1):148-50.
Search
our pre-2001 archives
for further information. Older issues of the printed magazine are also
indexed for your convenience.
1983-2001
indices ;
1999-Jan. 2003 indices
Once you find the magazines you'd like to order, please use our
convenient form, e-mail subscriptions@townsendletter.com,
or call 360.385.6021 (PST).
All rights reserved.
Web site by Sandy Hershelman Designs
