Page 1, 2, 3, 4
If cortisol supplements are taken in small bits (5 to 10 mg of hydrocortisone, for example) every half hour at the very beginning of the flu (in the minutes or first hour that the infection/inflammation begins), the flu disappears within one to two hours,91 as explained later when discussing cortisol therapy.
Table 2. Physical Complaints of Cortisol Deficiency
(Particularly frequent and intense in stressful conditions)
- Fatigue-like fatigue with the desire to lie down
- Deformed joints
- Tensed muscles
- Allergies: skin, nose-ear-throat with reddish coloration of inflamed zones, asthma, food allergies
- Tachycardia
- Intolerance to medications
- Palpitations, especially in stressful conditions
- Frequent infections: Sore throat, red eyes, ear pain, flu, etc.
- Excessive sweating in armpits, on hand palms, and on foot soles
- Reduced appetite
- Localized pains in structures that are put under pressure, such as the eyes, abdomen, joints, tendons, and muscles
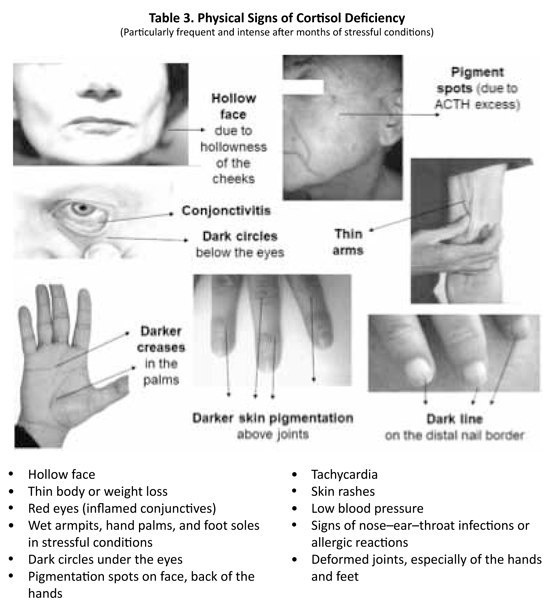
- Weight loss in people caused by a low appetite
Physical signs of cortisol deficiency also predominate at physical examinations. Four types of signs are found differing from each other by their cause: hyperpigmentation, malnutrition, adrenaline excess, low blood pressure, or inflammation (See Table 3).
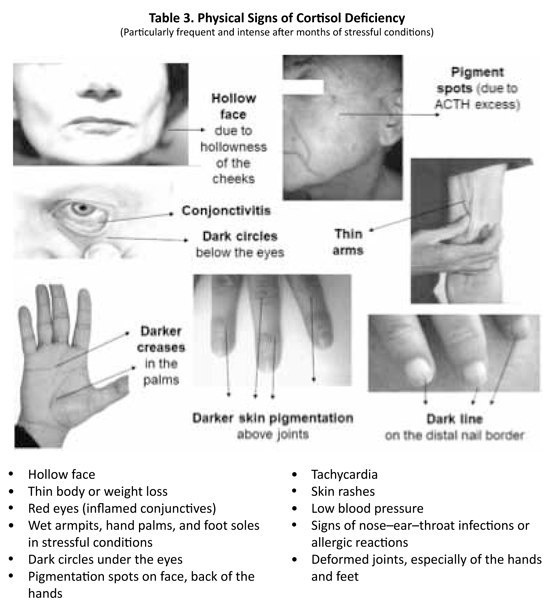
Pigmentation signs are specific to primary adrenal deficiency or Addison's disease, where the adrenal glands are weak but not the pituitary gland, which overproduces the hormone ACTH to stimulate cortisol production.82-83,92-93 As ACTH is a pigmenting hormone, pigmentation increases with greater intensity in some areas: dark circles under the eyes, hyperpigmented skin folds, and spots on the face and body. In cortisol deficiency, the pigmentation is irregular and reflects desperate attempts by the body to increase cortisol production by the adrenals. When it is not successful, it pours down increasingly greater amounts of ACTH, pigmenting the skin, which darkens even without sun exposure.
Cortisol-deficient patients also tend to have a hollow face and often thin body94-96 because they eat less or absorb the food less because their intestines are less effective at absorbing food.
The reduced food intake usually results from poor appetite, particularly for protein-rich foods, such as meat, because the nitrogen contained in the proteins tends to accumulate in the blood, a process called "azotemia." The deficient food absorption in the intestines is the consequence of the inflammation of the intestinal mucosa, impairing its absorptive actions. Patients with cortisol deficiency also weigh less because they lack body water due to the loss of cortisol's water-retaining effects.
As most patients overproduce adrenaline and noradrenaline to compensate for the cortisol deficit, signs of adrenaline excess, such as wet armpits, palms, and soles and trembling fingers, tachycardia,95 and acute systolic hypertension (the "white coat" arterial hypertension) may be found during the physical examination.
 As cortisol is also a hormone that raises the blood pressure, the blood pressure is often low at rest in people with a lack of cortisol.69,97-98 Finally, signs of inflammation are often found due to the loss of cortisol's anti-inflammatory effects: conjunctivitis, otitis, rhinitis, eczema,99-100 psoriasis, arthritis (with joint deformations, especially in the fingers), 101-105 gastritis, enteritis, colitis, and so on. As cortisol is also a hormone that raises the blood pressure, the blood pressure is often low at rest in people with a lack of cortisol.69,97-98 Finally, signs of inflammation are often found due to the loss of cortisol's anti-inflammatory effects: conjunctivitis, otitis, rhinitis, eczema,99-100 psoriasis, arthritis (with joint deformations, especially in the fingers), 101-105 gastritis, enteritis, colitis, and so on.
Cortisol deficiency favors the development of the following pathological conditions: allergies, including asthma and eczema, and generalized inflammatory diseases, such as rheumatoid arthritis,101-105 lupus erythematosus disseminatosus,106 systemic sclerosis, etc. Also, Hodgkin's disease and lymphomas may be facilitated by cortisol deficiency, as these diseases tend to regress with cortisol treatment.107-109
Laboratory Tests to Screen for Cortisol Deficiency
Three types of cortisol tests may help diagnose cortisol deficiency: blood, saliva, and 24-hour urine. They are all complementary to each other.
Firstly, blood or, better, serum tests of total cortisol,110 free cortisol, and transcortin (the protein that transports cortisol to the target cells in blood)111 can be assessed. Total cortisol consists of all cortisol found in the blood, regardless of whether it is bound or not to a transporting protein. Free cortisol is the small fraction of total cortisol that is not bound to any protein and easily diffuses into cells. The usefulness of testing for transcortin is that high levels of this transporter attach to cortisol excessively, so it remains in blood much longer, not sufficiently getting into the target cells.
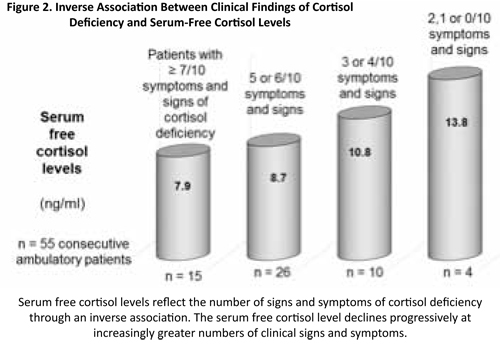
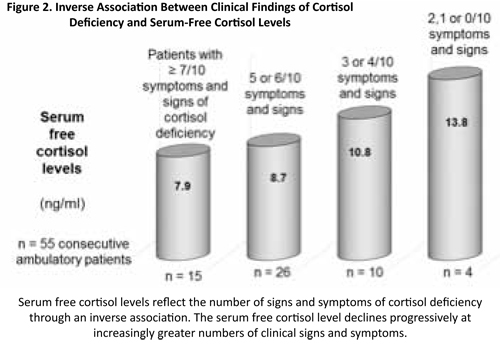
In the previous study where the prevalence of cortisol deficiency in our clinic was studied, we also checked the relationship between clinical findings and serum levels of free cortisol in 55 consecutive patients (36 females, mean age: 50.6 years; 19 males, mean age: 42.0 years). The study showed that serum levels of free cortisol reflect the number of signs and symptoms of cortisol deficiency relatively well through an inverse association. Progressively lower serum-free cortisol levels are observed with increasingly greater numbers of clinical signs and symptoms (on a scale from 0 to 10) as pictured in Figure 2.112
The ACTH-stimulation test is another blood test that evaluates the adrenal reserve, whether the adrenal glands have sufficient cortisol stored to supply supplementary cortisol in case of increased need. Injecting ACTH, the pituitary hormone that stimulates the secretion of cortisol, into a vein directly stimulates the adrenal glands. Check it every 30 minutes by withdrawing a blood sample and measuring the increase of cortisol obtained. Any doubling or more of the level of cortisol from the initial level indicates an adequate adrenal reserve and the likelihood that there is no cortisol deficiency. Unfortunately, in most clinics, the test is done by injecting 250 µg of ACTH, a huge overdose. Almost any adrenal glands, even weaker ones, will react to this overdose. Two studies have shown that using a more natural or physiological dose of 1 µg of ACTH allows for a much better differentiation between patients with adrenal deficiency from subjects without it. Whenever the cortisol level does not double with ACTH (whatever the initial serum cortisol level is), it indicates an intermediate degree of deficiency in the adrenal reserve.113 Studies have shown that critically ill patients in emergency rooms whose adrenal glands do not secrete enough cortisol after an ACTH injection die in the following days and weeks, while most other patients with good ACTH test survive.114-115 Thus, an abnormally low ACTH test helps detect critical persons who need a cortisol supplement for survival.
The saliva cortisol test checks the cortisol circadian rhythm with four samples taken at distant times.116-117 A higher morning peak of cortisol must appear in this test. Burnout patients usually have an insufficient morning cortisol peak. In the most severe cases, the cortisol morning rise may even be absent, and the cortisol circadian rhythm flat and inexistent.
The 24-hour urine test evaluates the excretion of cortisol and its metabolites in the urine during a full day and night cycle. The urinary cortisol level in this test reflects cortisol production during a 24-hour period.118-124 The measurement of cortisol's major metabolites, the 17-hydroxycorticoids, informs on cortisol's metabolic activity – how much cortisol is really used for action – during the same period.125-128 It is important to collect baseline urinary excretions of adrenal hormones, which are representative of the patient's adrenal activity, not stress-induced ones. Patients should therefore collect their urine in relaxed, sedentary conditions during the 24 hours that precede the test and during the 24 hours of the urine collection) to avoid increases in cortisol metabolites due to physical activity or high-stress conditions.
In all these tests, the measurements of protective anabolic hormones, such as DHEA, the sex hormones, and IGF-1, should be included, as most treatments with cortisol include one or more of these hormones in the treatment to ensure an adequate catabolic/anabolic hormone balance.
Cortisol Reference Ranges
Cortisol reference ranges are statistical ranges, not health ranges. If the reference range for cortisol in laboratory tests would be a range of serum levels corresponding to health, cortisol deficiency would only be diagnosed in 2.5% of the population, those whose cortisol level is below the lower reference limit.
However, the laboratory reference limits for cortisol are purely statistical parameters. Just as for other hormones, 2.5% of the population statistically have a cortisol level above the upper limit, 2.5% have a value below the lower limit, and the cortisol level of the remaining 95% is within the reference range,129 regardless of whether these subjects have a deficiency. The laboratory "normal" limits are, thus, not limits separating "healthy" levels, which would be all the levels within the reference interval, from the levels that are below or above the reference interval and that would correspond to levels of cortisol deficiency or excess. Reference limits only indicate where a patient's hormone level is compared to that of other patients who attend that laboratory.
Even if an entire population is deficient in a hormone, such as postmenopausal women who are all deficient in estradiol, 95% of this population would still have a hormone level within the reference range.
Both low and high serum cortisol levels within the reference range are associated with increased risks of pathology and mortality. Hormone levels are not necessarily adequate when they are within the "normal" range between the upper and lower reference limits of the laboratory tests. On the contrary, for most hormones – including cortisol – scientific research has shown that many serum levels within the reference range are significantly associated with disease and even mortality.130-150
Researchers have shown that serum cortisol levels within the reference range but near the lower reference limit are usually inadequate because they are associated with an increased likelihood of disease, suggesting that these lower levels within the reference range should also be treated. In my experience, borderline low limits are also associated with complaints and physical signs of cortisol deficiency. Studies have also shown that cortisol levels near the upper limits may be associated with an increased risk of disease, suggesting that the optimal cortisol level in sedentary conditions should be an average level, neither too high nor too low. However, in stressful situations, cortisol levels may need to increase to provide additional energy to respond to the stress; this is the reason that levels near the upper limit were associated with better outcome than lower levels in some studies.
Page 1, 2, 3, 4
|
![]()
![]()
![]()
![]()